Unlock Every Dollar, Simplify Every Step
The Challenge Practices Face
Healthcare organizations lose billions every year to denied claims, delayed payments, fragmented billing workflows, and poor patient collections. The result: rising administrative costs, frustrated staff, and missed revenue opportunities.
CERTIFY Health’s Revenue Cycle Management Software fixes this.

Revenue Cycle Management Healthcare + Merchant Billing Under One Roof

Front-End Precision
Real-time insurance verification, co-pay capture at check-in, automated reminders, and integrated patient billing.
Back-End Strength
Clean claims submission, denial prevention, and merchant-grade payment routing built on PCI DSS and HIPAA compliance.

Collections Simplified
Text-to-Pay, balance reminders, and online payment portals that work for every patient.
Outcome: Lower denials. Faster collections. Predictable cash flow.
Key Features of Our Healthcare RCM Software That Drive Revenue
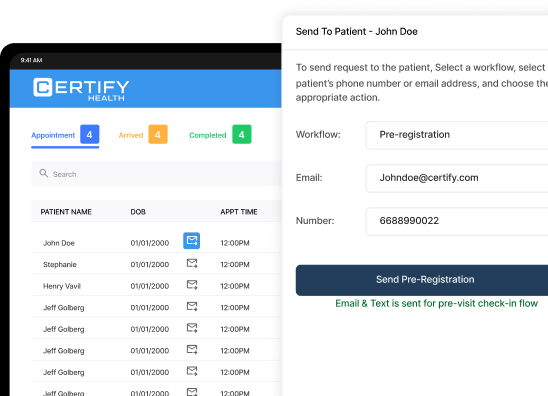
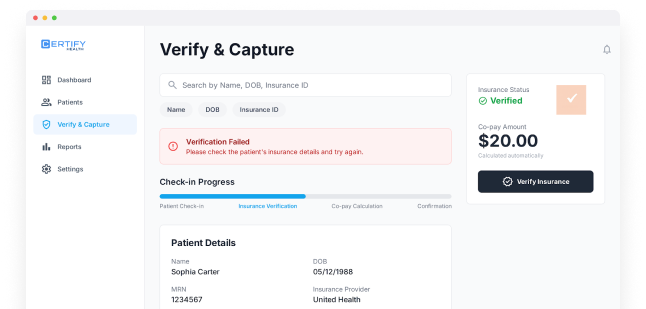
Insurance Eligibility Verification
Reduce denials at the source.
Learn More
Co-Pay & Balance Capture
Prompt payments at check-in, plus automated follow-ups.
Learn More
Why  Revenue Cycle Management Software Is Different
Revenue Cycle Management Software Is Different
Automated Payment Reminders
We’re not just healthcare billing; we bring merchant-level payments experience to your RCM.
Proven ROI
Practices recover millions in missed payments annually using CERTIFY Health.
Interoperable by Design
Works seamlessly with Epic, Cerner, NextGen, Dentrix, and other major EHR/PM systems.
Compliance First
HIPAA, HITRUST r2, PCI DSS, SOC 2, and GDPR built in.
Results That Matter
25%
fewer claim denials
with real-time eligibility.
40%
faster patient collections
through automated digital payment tools.
50%
front-desk workload reduction
via automation.
Millions
in recovered revenue
for multi-location practices and DSOs.
How Our RCM Software Works
Verify & Capture
Insurance eligibility + co-pay at check-in.
Practice Management (PMS)
Scheduling automation, ASAP List, staff tasking.
Practice Management (PMS)
Scheduling automation, ASAP List, staff tasking.

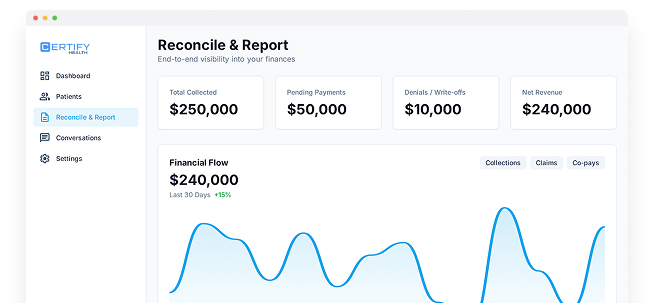
Reconcile & Report
End-to-end visibility into every dollar.
Built on Trust and Compliance

Trusted by Healthcare Practices Nationwide
CERTIFY Health’s revenue cycle management platform supports dental, vision, behavioral health, urgent care, and specialty practices across the U.S, optimizing financial performances.
FAQs
How does CERTIFY Health’s revenue cycle management software help prevent claim denials?
Denied claims are one of the biggest revenue leaks for healthcare practices. CERTIFY Health’s RCM software reduces denials by up to 40% through real-time insurance eligibility verification, accurate patient data capture, and compliance validation before submission.
What kind of payment options does the revenue cycle management software support for patients?
Our healthcare RCM software is built with a patient-first payment experience. It supports credit, debit, ACH, and digital wallets through PCI DSS–compliant merchant payment routing.
Patients can pay via text (Text-to-Pay), online portal, or automated reminders, helping you improve collection rates without adding manual follow-up work.
Can CERTIFY Health’s revenue cycle management platform integrate with my existing EHR or PMS?
Yes. CERTIFY Health is interoperable by design. Our healthcare revenue management cycle integrates seamlessly with major systems like Epic, Cerner, NextGen, Dentrix, and even in-house systems, without disrupting your existing workflows.
That means your team can continue using their current tools while CERTIFY Health automates the revenue operations behind the scenes.
What results can practices expect after implementing CERTIFY Health’s RCM platform?
Practices using CERTIFY Health’s revenue cycle management system typically experience:
- 40% fewer denials from real-time verification
- 60% faster patient collections via digital payment tools
- 50% less front-desk workload through automation
- Millions recovered in missed revenue for multi-location practices and DSOs
It’s a data-driven transformation, not just a software upgrade.







