Table of Contents
Introduction
Revenue cycle management (RCM) is the pulse of a financially healthy practice. From scheduling and insurance verification to billing and payment collection, every step either safeguards your profitability or erodes it.
Yet many practices still rely on outdated, manual processes that cause inefficiencies, delays, and denials. This guide explores common RCM challenges, proven strategies to boost collections, and ways to future-proof your practice with digital solutions.
What is Revenue Cycle Management in Healthcare?
Revenue Cycle Management (RCM) involves the administrative and clinical processes used to capture, track, and collect revenue for patient services.
It encompasses:
- Patient registration
- Insurance verification
- Claims submission
- Managing denials
- Payment posting
- Reporting and analytics
An efficient RCM workflow helps healthcare providers receive payments more quickly and accurately.
Picture this: You’re running a successful healthcare practice, but every month feels like a financial roller coaster. Claims get denied, payments trickle in slower than expected, and your staff spends more time chasing payments than focusing on patient care. Sound familiar?
Here’s the thing – you’re not alone. The healthcare industry is drowning in financial chaos, with revenue cycle management becoming more complex than ever. But what if we told you there’s a way to transform this chaos into a well-oiled profit machine?
Welcome to the revolution of RCM automation with CERTIFY Health, where streamlined workflows meet boosted profitability.
The Healthcare Financial Crisis: More Than Just Numbers
Healthcare practices today face unprecedented financial pressures. Claims denial rates have risen to 11.81%, which is a worrying statistic. That’s not just a statistic – that’s thousands of dollars in lost revenue for every practice.
But here’s where it gets interesting. While studies say claim denials have increased, the global revenue cycle management market is experiencing explosive growth, reaching $151.91 billion and projected to hit $451.29 billion by 2034. This indicates that healthcare practices are desperately looking for solutions.
The reality? Over 78% of health systems are now adopting some sort of automated RCM solutions, not because it’s trendy, but because it’s becoming essential for survival.
Understanding Revenue Cycle Management: The Financial Heartbeat of Healthcare
Revenue cycle management healthcare goes far beyond billing—it includes managing the entire financial process for each patient encounter, from registration all the way to final payment.
Think of it as your practice’s financial heartbeat, pumping life-sustaining cash flow through every aspect of your operations.
The RCM process includes various RCM stages:
- Patient registration and scheduling
- Insurance verification and authorization
- Charge capture and medical coding
- Claims submission and processing
- Payment posting and reconciliation
- Denial management and appeals
- Patient billing and collections
When these revenue cycle in healthcare stages work seamlessly together, they create what every practice dreams of: steady cash flow, reduced claim denials, and enhanced patient satisfaction.
Did you know? 💡
As per MGMA report, 40% of medical practices fell short of their revenue goals in 2021. Why? A big part of the problem was old-school, manual processes—think endless paperwork, phone tag with payers, and slow data entry.
These bottlenecks didn’t just drain time—they also delayed reimbursements and sent days in A/R soaring.
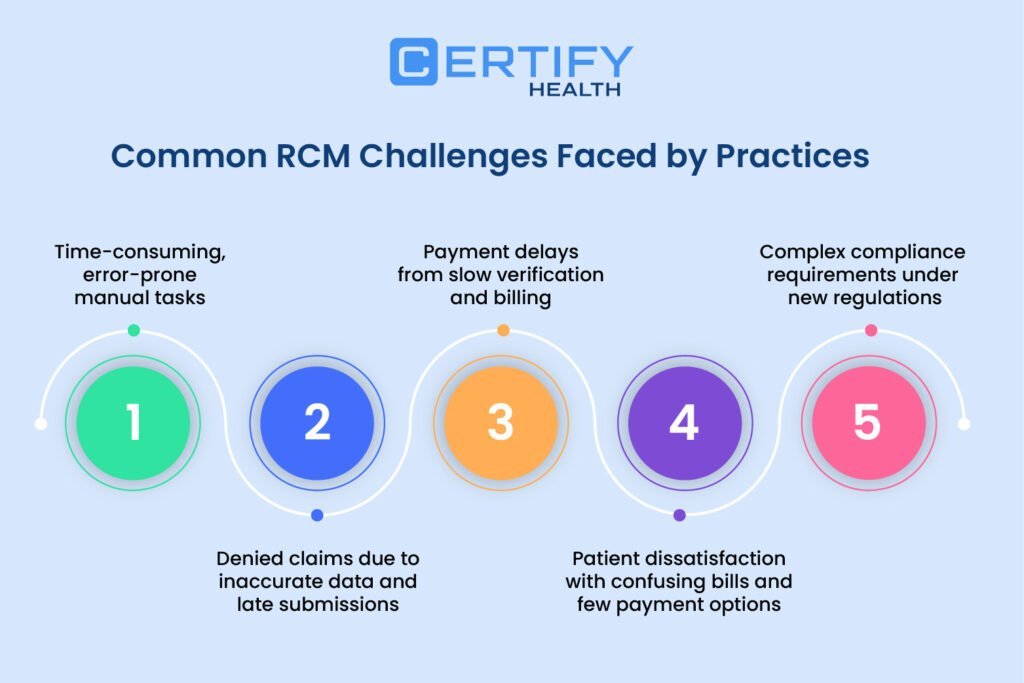
Common Revenue Cycle Management Challenges
TL; DR
Common Revenue Cycle Challenges Faced by Healthcare Practices
Delayed Claims and Reimbursements
- Manual claim filing processes are slow and prone to errors.
- Payment delays result in cash flow gaps and increased A/R days.
High Rate of Claim Denials
- Denials often stem from incorrect patient data or coding errors.
- Up to 65% of denied claims go uncorrected and unsubmitted.
Patient Payment Gaps
- Out-of-pocket expenses are rising, but practices still struggle to collect.
- Many patients delay or default due to lack of financial clarity.
Poor Front-End Processes
- Inefficient patient intake and eligibility checks lead to errors early on.
- This mismanagement snowballs into downstream billing issues.
Manual Processes
Every time your staff notes down your patient’s insurance number or retypes information into a system, they are at risk of errors. Manual processes are not only time-consuming, but result in high error rates.
Multiply that by dozens of patients every day, and you are staring at a steady drip of lost revenue that floods by the end of the year. This time-intensive workflow binds your staff to hours chasing missing information or reworking claims, which further adds to administrative costs.
Solution? You need automated solutions that can handle front-desk manual tasks with accuracy, like digital patient registration, digital intake, real-time insurance verification, automated payments, etc. It will streamline your workflow, stop the billing cycle from stretching out, and help your practice keep up with good cash flow.
Claim Denials
Claim denials are the biggest threat to your practice’s steady cash flow.
Coding errors, missing documentation, or even simple typos in names or DOB can result in claim denials. This creates a vicious cycle where practices spend valuable resources overturning denials while their cash flow suffers. Most claim denials are preventable and occur because of breakdowns in your RCM process.
You just need to fix the breakdowns through the right RCM solution like CERTIFY Health’s revenue cycle management software. It can automate the front-end revenue cycle management, reduce errors and delays, and flag issues before they become denials.
Slow Payments
Finally—after manually verifying every patient’s insurance coverage, tracking down co-pays and deductibles, coding procedures, creating bills, and submitting everything to the insurance companies—your staff has to do what?
Wait.
Wait for payments that trickle in slowly, no matter how hard they’ve worked. Why? Because of payer processing times, delayed billing, and late submissions.
And those slow payments? They don’t just dent your bottom line—they choke your ability to care for patients. When cash flow dries up, you can’t invest in new equipment. You can’t hire more staff. You can’t grow your practice.
RCM automation is the key to breaking this cycle. It streamlines claims submission, automates payment posting, and offers digital payment options to patients. It accelerates your payment cycle and keeps cash flowing steadily into your practice
Patient Dissatisfaction
Here’s a painful truth: patient dissatisfaction with your billing can be just as damaging as claim denials. Patients no longer want surprises—and they definitely don’t want to rely on only one method of payment, especially when it comes to healthcare.
If your revenue cycle is stuck in the past, your patients will move to another provider without hesitation.
In today’s healthcare, there’s no room for confusing bills, limited payment options, and poor patient communication.
Your practice needs a solution that can create accurate bills, provide upfront estimates, and offer multiple payment methods—just like CERTIFY Health’s patient payment management software.
It not only delivers digital statements but also lets patients pay before they walk in for treatment, choose from different payment options, and receive automated reminders so they can set up auto-payments.
Regulatory Pressures
Regulatory pressures are one of the fastest-growing challenges in revenue cycle management healthcare. From the No Surprises Act to ever-changing payer requirements, the rules are always shifting—and the penalties for non-compliance can be severe.
You’re making a recipe for disaster if you manage compliance manually. It’s too easy to miss a new requirement or overlook a critical update. And when mistakes happen, the consequences go beyond denied claims—they can include hefty fines, audits, and even legal action.
The right RCM platform like CERTIFY Health takes the guesswork out of compliance. With built-in rules engines, real-time updates, and expert support, you can stay ahead of regulatory changes and protect your practice from costly mistakes.
How CERTIFY Health Streamlines the Revenue Cycle for Healthcare Practices
CERTIFY Health doesn’t just offer an RCM platform – it delivers a complete revenue cycle automation transformation that addresses every pain point in your financial workflow.
TL; DR
7 Essential Steps to Fix Revenue Leaks in RCM
Automate Insurance Eligibility Verification
Leverage CERTIFY Health’s real-time eligibility checks to cut down on denied claims and eliminate manual errors.
Digitize Patient Intake and Registration
Simplify data gathering by using online intake forms, which cut down on paperwork and guard against data entry errors.
Offer Transparent Cost Estimates Upfront
When patients clearly understand their financial responsibility early on, they’re more likely to pay on time.
Enable Digital and Mobile Payments
Boost collection rates with CERTIFY Health’s Text2Pay, card-on-file options, and secure patient payment portals.
Use RCM Analytics to Identify Bottlenecks
Monitor key metrics like denial rate, clean claim rate, and A/R aging to uncover inefficiencies and drive improvements.
Automate Claims Scrubbing and Submission
Improve accuracy and accelerate payment cycles by automating claims validation and submission workflows.
Follow Up with Automated Denial Management
Practice management tools like CERTIFY Health help you quickly correct, track, and resubmit denied claims for faster reimbursement.
Patient Scheduling
Ever wish your calendar could just fill itself?
With CERTIFY Health’s patient scheduling software, it practically does. Patients can book appointments online—no more endless phone tag or “please hold” music.
The result? Fewer no-shows and a lighter load for your front desk. Picture your team dedicating more time to assisting patients instead of chasing confirmations.
That’s not just convenient—it’s a game changer for your workflow. Why complicate scheduling when self-scheduling can make it easy?
Patient Pre-Registration
Paperwork mountain? Not here.
CERTIFY Health lets patients pre-register online, collecting all the details you need before they even walk in. No more deciphering handwriting or missing insurance info.
Everything’s digital, accurate, and ready when the patient arrives. It’s like having your ducks in a row—before you’ve even had your morning coffee. Less chaos, fewer errors, happier staff.
Insurance Verification
Ever played “Guess That Coverage” with a patient’s insurance? Not fun.
CERTIFY Health’s real-time insurance verification software helps you know exactly what’s covered—before the visit. No more surprises at checkout.
Patients are in the loop, your team’s not scrambling, and billing gets a whole lot smoother. Why gamble with coverage when you can know for sure?
Charge Capture
Blink and you’ll miss it—unless you’re using CERTIFY Health.
Every service, every procedure, every detail is automatically captured and documented. That means accurate billing, fewer missed charges, and a lot less “wait, did we bill for that?” moments.
Your revenue cycle just got a turbo boost.
Medical Coding
Coding headaches? Not anymore.
CERTIFY Health integrates with coding tools (or your favorite outsourced team) to keep every code current and correct.
No more second-guessing or frantic Google searches. Just clean, compliant coding that gets claims paid faster. Because your team has better things to do than untangle code confusion.
Claims Submission
Push a button. Done.
CERTIFY Health sends claims directly to payers electronically, ensuring that all necessary information is included. No more printing, stuffing envelopes, or chasing faxes.
Claims get where they need to go—fast. That means quicker payments and less time spent wondering, “Did they get it?” Spoiler: They did.
Claims Processing
Out of sight, out of mind? Not with CERTIFY Health.
You get real-time tracking on every claim, with instant alerts if something’s denied or rejected. No more waiting in the dark or losing track of claims in the shuffle.
You are always aware of everything, and nothing goes unnoticed. Think of it as your claims command center.
Payment Posting
Cha-ching—payments posted in real time.
CERTIFY Health reconciles payments and updates ledgers automatically, so your financial records are always spot-on. No more manual entry marathons or late-night number crunching.
You see what’s paid, what’s pending, and what needs attention—at a glance. That’s clarity you can bank on.
Denial Management
Denied claims? Don’t just sigh—solve them.
CERTIFY Health flags denials instantly and helps you fix issues before they become revenue leaks. Plus, built-in analytics show you patterns, so you can stop problems before they start.
It’s like having a denial detective on your team, working 24/7 to keep your cash flow healthy.
Accounts Receivable (AR) Follow-Up
Nobody loves chasing overdue balances.
CERTIFY Health’s patient engagement software automates reminders and follow-ups, so patients know what they owe and how to pay. No more awkward calls or sticky notes piling up.
Your AR shrinks, your collections go up, and your staff can finally breathe a little easier.
Patient Statement Processing
Ever wish patient billing was as easy as sending a text?
With CERTIFY Health, it is. Digital statements and e-invoices go out automatically—no more printing, folding, or mailing. Patients get upfront, timely info, and you get payment faster. Goodbye, billing bottlenecks.
Hello, happy patients (and accountants).
Patient Payment Collection
Let’s make paying painless.
CERTIFY Health offers digital payment options—Text2Pay, kiosks, online portals, even custom payment plans. Patients choose what works for them, and your collections don’t miss a beat.
No more “the check’s in the mail.” Just fast, secure payments that keep your practice moving forward.
Reporting & Analytics
What’s working? What’s not?
CERTIFY Health’s real-time dashboards give you the answers—instantly. Track trends, monitor KPIs, and spot opportunities to boost cash flow.
No more flying blind or waiting for end-of-month reports. You receive the insights you require exactly when you require them. Now that’s smart practice management.
CERTIFY Health’s RCM platform automates and optimizes each stage of the revenue cycle:
Front-End Revenue Cycle Management
Front end revenue cycle management with CERTIFY Health starts before patients even walk through your door. The platform’s real-time eligibility checks and deductible validation ensure accurate coverage verification, while transparent cost estimates build patient trust from the first interaction.
The seamless integration with existing EHR/PM systems means no disruption to your current workflows, just enhanced efficiency and accuracy.
Mid Revenue Cycle Management
Mid revenue cycle management is where CERTIFY Health’s RCM automation truly shines. Automated charge capture and medical coding integration eliminate manual errors, while seamless electronic claims submission with payer integration accelerates processing times.
The platform’s proactive claim monitoring system provides real-time alerts for denials or rejections, enabling immediate corrective action instead of reactive firefighting.
Back-End Revenue Cycle Management
Back-end revenue cycle optimization focuses on turning approved claims into actual cash. CERTIFY Health’s automated payment posting and real-time reconciliation ensure accurate financial records, while the denial management system proactively identifies and resolves issues before they impact cash flow.
The digital patient payment tools – including Text2Pay, kiosks, portals, and mobile options – provide multiple convenient payment channels that significantly boost collection rates.
Patient Engagement
Here’s where CERTIFY Health breaks the traditional mold. While most RCM solutions focus purely on back-office efficiency, CERTIFY Health understands that enhanced patient satisfaction drives better financial outcomes.
The platform’s digital statements and e-invoices provide crystal-clear communication, while custom payment plans and auto-scheduled options make it easier for patients to pay their bills on time. The result? Automated reminders that cut overdue balances by 25%.
Why Your RCM Strategy Needs an Upgrade?
Healthcare finance is evolving. Payers are more complex, patients expect digital options, and regulatory compliance is tighter than ever. Practices using outdated billing software or fragmented systems are losing revenue they could otherwise secure.
Here’s where integrated, end-to-end RCM platforms make a difference.
Proven Results: The CERTIFY Health Difference
CERTIFY Health: A Practice Management Software Built for Providers RCM
CERTIFY Health streamlines every touchpoint of the revenue cycle:
| Feature | CERTIFY Health | Traditional RCM |
|---|---|---|
| Eligibility verification | Real-time, automated | Manual, error-prone |
| Digital intake | Integrated and paperless | Physical paperwork |
| Patient payments | Text2Pay, card-on-file | In-office collections only |
| Claim submission | Automated and optimized | Delayed and manual |
| Denial management | Real-time alerts and resubmissions | Slow or missed resubmissions |
| Analytics | Live dashboards and RCM KPIs | Limited or no visibility |
CERTIFY Health’s RCM implementation delivers measurable results that directly impact your practice profitability:
- Faster payment cycles through streamlined workflows
- Fewer denials via proactive verification and monitoring
- Higher collections enabled by digital tools and flexible payment options
- Reduced overdue balances through automated patient engagement
- Enhanced patient satisfaction via transparent, convenient financial interactions
These aren’t just promises – they’re outcomes experienced by practices across specialties and sizes.
Implementation Success
RCM implementation with CERTIFY Health isn’t just about technology deployment – it’s about practice transformation. The process includes:
Seamless integration with your existing systems ensures minimal disruption while maximizing benefits. Expert support guides you through system selection and customization, while comprehensive staff training ensures optimal utilization from day one.
Ongoing support includes continuous updates and customer service, ensuring your RCM platform evolves with your practice’s changing needs and industry regulations.
Conclusion
The healthcare industry stands at a crossroads. You can keep struggling with manual processes, slow payments, and revenue leakage, or embrace revenue cycle automation that’s transforming financial performance everywhere.
CERTIFY Health’s RCM platform is more than software—it’s a complete solution. From front-end revenue cycle management to back-end revenue cycle optimization, it drives real improvements in cash flow, collections, and patient satisfaction.
Don’t let inefficient processes drain your practice profitability.
Ready to experience the difference? Book your CERTIFY Health Demo today
FAQ's
Absolutely. Modern RCM solutions help practices offer convenient online payment options, clearer billing statements, proactive communication about costs, and faster resolution of billing questions, all of which lead to a smoother and more satisfying patient experience.
























