Table of Contents
Introduction
Wait—have you ever imagined your practice making front-page news for all the wrong reasons?
A single slip-up. One unencrypted file. Thousands of patient records leaked.
Cue lawsuits, media frenzy, and millions in fines. That’s not just a PR nightmare—it’s a career-ending disaster.
Scary? It should be. Protecting PHI (Protected Health Information) is not just a legal requirement. It is a sacred trust between you and your patients.
This is where the HIPAA Act steps in. But don’t mistake it for some dusty compliance checklist. The role of HIPAA is way bigger—it’s the backbone of patient confidence and operational credibility in healthcare.
The consequences of HIPAA non-compliance? Brutal. Financial ruin. Reputational damage. Operational chaos. And yes—legal action that can shut your doors for good.
This guide breaks down everything:
- What the HIPAA Act covers? (in plain English)
- The real-world consequences of HIPAA non-compliance
- Battle-tested strategies to lock down compliance and protect what matters most—your patients and your practice.
What is the HIPAA Act?
The Health Insurance Portability and Accountability Act (HIPAA) was implemented on April 14, 2003, with a focus on achieving two primary objectives:
- Make healthcare more efficient by standardizing electronic data exchange
- Protect sensitive patient data like
But here’s the twist: What started as a law to ensure health insurance followed you from job to job quickly evolved into a powerful PHI protection framework.
Why does this matter today?
Because today everything is digital—EHRs, patient portals, telehealth visits, text messages. And without strict rules, patient privacy would be toast. That’s where the importance of HIPAA kicks in.
HIPAA doesn’t merely tag your practice as “compliant”—it requires you to genuinely safeguard PHI (Protected Health Information) whenever it is generated, accessed, distributed, or stored.
How does HIPAA impact the healthcare industry?
If you are a healthcare provider, health plan, or clearinghouse, you are legally responsible for safeguarding PHI. No shortcuts. Here’s what HIPAA enforces:
- Confidentiality: Only the right people see the right data
- Integrity: Data stays accurate and unaltered
- Availability: Info is accessible when it’s needed—securely
So when you hear “Introduction to HIPAA,” know this:
- It’s not just a boring legal acronym.
- It’s the foundation of digital trust in modern healthcare.
- And if you are not taking it seriously, you are already behind.
You Might Also Like to Read our Blog on: The Ultimate Guide to Healthcare Compliance for Medical Practices
Key HIPAA Rules Impacting Healthcare Practices
TL; DR:
What are the key HIPAA Rules?
The five key HIPAA rules are as follows:
- Privacy Rule: Patients have the right to access, correct, and control who sees their health info. No sharing PHI without consent—ever.
- Security Rule: Protect electronic PHI (ePHI) using technical, administrative, and physical safeguards.
- Enforcement Rule: Break the rules? Expect investigations, fines, and hipaa penalties for non-compliance from HHS.
- Transaction Rule: Standardizes electronic data like claims, authorizations, and payments.
- Unique Identifiers Rule: Assigns unique IDs to providers, plans, and employers (e.g., NPI).
HIPAA Privacy Rule: Your Patient’s Data, Their Rights
Imagine a patient asking to see their medical records—under HIPAA, they have every right to access them.
The HIPAA Privacy Rule sets nationwide standards for how you protect medical records and personal health information. It gives patients real power:
- The right to access their health records
- The right to request corrections
- And—most importantly—the right to control who sees their information
No, you can’t just fax their chart to anyone. Disclosing PHI without patient consent? That’s a major no-no.
HIPAA Security Rule: Locking Down ePHI
The HIPAA Security Rule acts like a digital gatekeeper, guarding the entry to your sensitive data. The main goal is to use force to safeguard electronic PHI (ePHI).
Covered entities and business associates must implement:
- Administrative safeguards (like training and risk assessments)
- Physical safeguards (like secure access to hardware)
- Technical safeguards (think encryption and secure logins)
Confidentiality, integrity, and availability aren’t just buzzwords—they’re the core requirements.
HIPAA Enforcement Rule: Break the Rules, Pay the Price
HIPAA takes it seriously. The HIPAA Enforcement Rule explains what the Department of Health and Human Services (HHS) can do to:
- Investigate violations
- Enforce compliance
- And drop civil penalties like a hammer
No policy? No audit trail? No security measures? You are a target. This rule ensures everyone in healthcare is accountable.
HIPAA Transaction Rule: Standardize or Get Stuck in Paperwork
The HIPAA Transaction Rule forces healthcare to speak the same digital language. It standardizes electronic transactions—think:
- Claims
- Eligibility checks
- Authorizations
- Payments
It even mandates standard code sets like ICD-10 for diagnoses and CPT for procedures. Translation: less admin chaos, more automation.
(Bonus) HIPAA Unique Identifiers Rule: One Code to ID Them All
This one’s often forgotten, but it’s crucial. The HIPAA Unique Identifiers Rule assigns standard identifiers to:
- Providers (NPI)
- Health plans
- Employers
- Patients (in limited use)
Think of it as HIPAA’s way of saying, “Let’s stop confusing John Smith with John S. Smith.”
Each of these rules plays a critical role in the HIPAA ecosystem. Skip one—and you’re not HIPAA compliant. Worse? You are risking your patients’ trust and your practice’s future.
Also, Read our Blog on: A Complete Guide on HIPAA Compliance in Patient Intake
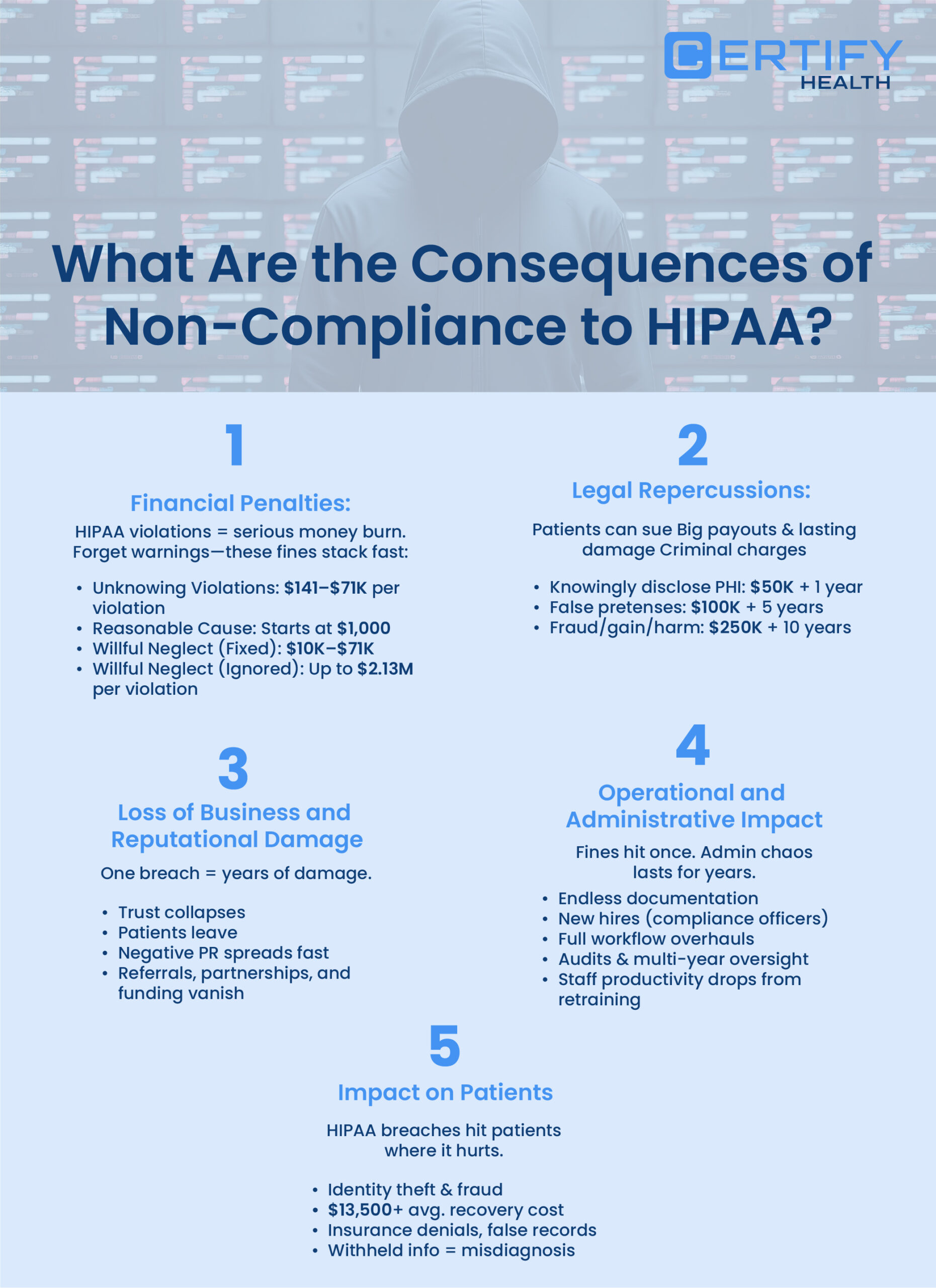
What Are the Consequences of Non-Compliance to HIPAA?
TL; DR
What Are the Consequences of Non-Compliance to HIPAA?
- Financial Penalties: One violation can cost up to $2.13 million—and yes, the fines stack.
- Legal Repercussions: Civil lawsuits and criminal charges can follow, including jail time.
- Reputation Damage: Public breaches destroy patient trust and drive business away.
- Federal Exclusion: You can be barred from Medicare, Medicaid, and lose major revenue streams.
- Operational Burden: Investigations trigger audits, reports, and resource-draining compliance overhauls.
- Admin Overload: Staff get buried in paperwork, pulling focus from patient care.
- Patient Fallout: Data breaches lead to identity theft, delayed care, and broken trust.
The consequences of non-compliance with HIPAA extend far beyond simple regulatory violations – they can fundamentally alter an organization’s trajectory and survival prospects.
Understanding these implication of HIPAA non-compliance helps healthcare organizations recognize the critical importance of robust compliance programs.
1. Financial Penalties
Financial penalties are the first and most brutal wake-up call when you drop the HIPAA ball.
These aren’t symbolic. They are business-ending.
We are discussing civil monetary penalties that scale fast—and don’t stop.
Here’s how the consequences of non-compliance with HIPAA can wipe out your bottom line:
HIPAA’s Four-Tier Penalty Civil Penalties Structure:
Based on how bad the violation is—and how much you should’ve known better.
Unknowing Violations
→ $141 to $71,162 per violation
→ Max annual cap? $2.13 million
Reasonable Cause
→ Starts at $1,000 per violation
→ Still hits the $71K
Willful Neglect (Corrected within 30 days)
→ $10,000 to $71,162 per violation
Willful Neglect (NOT corrected)
→ The heavy-hitter: $71,162 to $2.13 million per violation
Annual Maximum:
Let that sink in: $2+ million for a single type of violation—and that’s before you add legal fees, PR clean-up, or remediation costs. Indeed, it deteriorates further.
- Multiple violations? The fines stack. Fast.
- Repeat offenses? Your annual cap explodes.
- Inflation? To keep the sting strong, these penalties are modified annually.
For small and mid-sized healthcare practices, this isn’t just painful—it’s existential.
2. Legal Repercussions
When it comes to HIPAA, financial penalties are just the beginning. The legal repercussions? They cut deeper—and last longer.
Civil Lawsuits: Patients Can—and Do—Sue
If a data breach impacts someone, they can personally sue your practice. These civil lawsuits often result in payouts that far exceed the original HIPAA fines for non compliance.
Think: damages, settlements, legal fees—and a reputation that may never recover
Criminal Penalties: When HIPAA Violations Turn Felonious
Jail Time: For egregious violations involving intent to sell, transfer, or use health information for commercial gain or malicious harm, individuals can face up to 10 years in prison. The Department of Justice classifies criminal penalties into three levels based on intent and severity:
HIPAA Criminal Penalty Levels
-
Level 1 – Basic Violations: Up to $50,000 fine and 1 year in jail for knowingly mishandling PHI.
- Level 2 – False Pretenses: Up to $100,000 fine and 5 years in jail for obtaining PHI under false pretenses.
- Level 3 – Intentional Misuse: Up to $250,000 fine and 10 years in jail for using PHI for profit, personal gain, or harm.
3. Operational and Reputational Damage
What really crushes a healthcare organization after a HIPAA violation? Loss of business and reputational damage—the kind that sticks around long after the fines are paid.
As discussed earlier – One Breach. One Headline. A Whole Lot of Fallout.
The moment a HIPAA violation hits the news, the negative publicity spreads like wildfire.
It’s not just industry outlets. It’s Twitter. Facebook. Local media. Patient groups. And the damage doesn’t stop when the headline fades.
- Trust tanks
- Loyal patients leave
- New patients stay away
In healthcare, trust is currency—and once it’s gone, it’s tough (and expensive) to earn back.
When people believe their privacy is not safe, they search for other options. And it’s not just the directly impacted patients—entire communities take notice. Word spreads. Reviews tank. Competitors benefit.
Suddenly, you’re not just fixing compliance issues—you’re trying to rebuild your entire reputation.
Federal Program Exclusion: The Nail in the Coffin
Believe it can’t become worse? HIPAA non-compliance can get your practice excluded from Medicare, Medicaid, and other federal programs.
Translation?
- A massive chunk of your revenue—gone overnight
- Regaining eligibility takes time, resources, and painful red tape
- Many practices never financially recover
In healthcare, reputation isn’t isolated—it’s interconnected. Once you’re flagged as non-compliant, it doesn’t just scare patients.
- Business associates back off
- Referring physicians stop referring
- Hospitals and institutional partners cut ties
The bitter truth here is nobody wants to risk getting pulled down with you.
4. Individual or Administrative Impact
Fines make headlines. But behind the scenes? It’s the operational impact that quietly drains your practice day after day.
The Admin Avalanche Begins
Once a violation is reported, that’s when the real work truly begins. Investigations. Documentation. Compliance reports. More documentation.
That’s when the administrative burden spikes—fast.
- Staff are pulled from their regular duties
- Leaders scramble to develop and execute action plans
- Patient care takes a backseat to paperwork
Compliance is no longer just an IT or legal concern—it’s a shared responsibility across the entire organization.
Corrective Action = Organizational Overhaul
Enforcement agencies don’t just ask for a quick fix. They demand long-term, measurable change—and that comes at a cost.
Your organization may have to:
- Hire full-time compliance staff
- Deploy new technologies
- Restructure workflows from top to bottom
These action plans are resource-heavy, slow-moving, and non-negotiable.
External Oversight = Constant Pressure
Violators often face:
- Independent audits
- Ongoing reviews
- Corporate Integrity Agreements (yes, multi-year obligations)
That means years of monitoring, reporting, and adapting your operations under strict scrutiny.
Staff Retraining Slows Everything Down
Staff retraining is necessary—but it hurts productivity in the short term.
- Time spent in training is time away from patient care
- New policies = new workflows = more room for error
- The adjustment period can feel like starting from scratch
What are the other consequences of HIPAA non compliance?
A compliance breach can have serious repercussions:
- Employment impact: Staff may face dismissal if they violate regulations.
- Financial consequences: Loss of income can occur due to termination or imposed sanctions.
- Reputation risk: The organization’s public image and trust can suffer.
- Corrective measures: Regulatory bodies like the OCR may mandate audits, training, or other interventions to prevent future violations.
5. Impact on Patients
When Protected Health Information (PHI) is exposed, it’s not just a privacy issue. For the patient, it’s a deeply personal crisis.
Risk of Identity Theft and Fraud: The Real-Life Fallout
A single data breach can lead to:
- Medical identity theft
- Insurance fraud
- Illegal access to prescriptions
- Fake medical records
The risk of identity theft isn’t theoretical—patients often spend 200+ hours and over $13,500 to resolve it. And even then, the damage may linger.
When Patients No Longer Trust You
HIPAA breaches break the trust patients place in providers. That fear has real consequences:
- Patients delay or avoid care
- They withhold important symptoms or history
- Misdiagnosis and mistreatment become more likely
The result? Worse outcomes—and a relationship that may never fully heal.
View our Latest Blog on The Complete Guide to HIPAA-Compliant Payment Processing in Healthcare
How to Prevent HIPAA Non-Compliance?

Protentional consequences of HIPAA violations can be prevented, it demands a proactive, multi-layered strategy that covers technical safeguards, administrative policies, and human behavior.
Comprehensive Risk Analysis and Management
A robust risk assessment program is the cornerstone of HIPAA compliance.
Organizations must perform comprehensive risk analysis to identify where PHI is created, stored, or transmitted. This includes evaluating both technical threats (like cybersecurity gaps) and non-technical risks (like staff behavior).
Results should drive action plans to address the most critical vulnerabilities first, ensuring ongoing monitoring and mitigation. Prioritizing risks ensures smarter use of resources—and stronger PHI protection.
Robust Security Measures
Robust security measures—as required by the HIPAA Security Rule—include administrative, physical, and technical safeguards.
This means clear policies, restricted physical access, encryption, role-based access, and audit trails. These controls work together to secure ePHI from unauthorized access or breaches.
Organizations must continuously update safeguards or adopt new technologies like CERTIFY Health’s HIPAA Compliant Solutions for Practice Management to ensure PHI protection without compromising patient care.
Employee Training and Awareness
Employee awareness and training guarantees that all team members, regardless of role, are aware of their HIPAA obligations.
New staff must be trained promptly quickly, with updates given whenever policies change. Customize training based on job roles to cover PHI handling, proper disclosures, and incident reporting. Frequent refreshers and continuous communication foster a security-first mentality.
Documented training programs demonstrate compliance and reinforce your organization’s commitment to PHI protection through education-driven action plans.
Strict Policies for Business Associates
Vendors accessing PHI must follow strict rules—this is where Business Associate Agreements (BAAs) come in.
These contracts outline acceptable data use, breach notification protocols, and required safeguards. Conduct due diligence and regular audits. Subcontractors? They need their own agreements too.
Continuous monitoring and clear action plans help maintain control over third-party access and support full PHI protection across the care network.
Prompt Breach Notification
Even with safeguards, breaches can happen—prompt breach notification is key to damage control.
HIPAA requires notifying affected individuals within 60 days, with large breaches also reported to HHS and the media. Business associates must notify covered entities so they can act fast.
Having a well-defined breach response action plan, including containment and investigation steps, helps preserve trust and demonstrates your commitment to transparency and PHI protection, even in worst-case scenarios.
Conclusion
HIPAA compliance goes beyond just meeting legal standards—it’s about upholding patient trust and ensuring their safety. Consequences of non-compliance in healthcare range from fines and legal action to harm to one’s reputation and prolonged business interruption.
The good news? Proactive strategies work. With comprehensive solutions like CERTIFY Health’s Practice Management Software you can perform risk analysis, take robust security measures, and prompt breach notification, you build a solid defense that protects both your patients and your practice.
The choice is simple: stay ahead with smart compliance—or fall behind and pay the price.
























