Table of Contents
Introduction: Why Follow-Up Management Is a Clinic’s Hidden ROI Engine
Let’s start with evidence.
Outpatient patient follow up within 7 days of discharge has been consistently associated with significant reductions in 30-day readmissions for high-risk conditions such as heart failure (HF) and acute myocardial infarction (AMI), particularly among older adults.
That matters because 30-day readmissions are not just clinical failures; they are financial events. They affect:
- CMS quality performance
- Value-based reimbursement
- Risk-adjusted contracts
- Total cost of care
- Public reporting scores
In other words, structured outpatient follow up directly influences your clinic’s revenue stability and reputation.
Yet most clinics still treat follow up management as an administrative afterthought….a reminder, a call, a task completed in isolation.
That’s the strategic error.

Patient Follow-Up Is a Quality Lever
Follow-up is where continuity either holds or breaks.
Done properly, it improves:
| Patient retention | Continuity drives lifetime value |
|---|---|
| Patient satisfaction | Patients feel monitored and supported |
| Adherence rates | Medication and care plan compliance improves |
| Patient reported outcomes | Symptom control and functional improvement |
| Clinical quality reporting metrics | Improved data for value-based care and compliance |
Done poorly, it produces:
- Preventable readmissions
- No-shows
- Medication non-adherence
- Fragmented care
- Revenue leakage
The clinics that outperform competitors operate a structured follow up workflow tied to measurable outcomes.
The Financial Multiplier Effect
Follow-up impacts more than readmissions.
Consider the compounding model:
- Early follow-up reduces complications
- Fewer complications improve patient experience
- Better experience increases patient satisfaction
- Higher satisfaction increases patient retention
- Higher retention increases lifetime patient value
That loop is highly operational.
If your clinic loses patients after one acute episode, the problem may not be access. It may be weak follow-up continuity.
Follow-Up as Clinical Quality Management
In modern outpatient care, follow-up is part of clinical quality management.
It connects:
- Risk stratification
- Care coordination
- Workflow integration
- Outcome tracking
- Continuous improvement
When integrated correctly, follow-up becomes a measurable system.
And here’s the uncomfortable truth:
Most clinics treat follow-up like a checkbox. In reality, it is a quality measure with measurable financial, clinical, and patient-loyalty impacts.
If you don’t structure it deliberately, variability creeps in.
Variability increases risk.
Risk increases cost.
“More calls” alone wouldn’t suffice. The goal is engineered, risk-adjusted, outcome-driven follow up management.
The Strategic Shift
Stop asking: “Did we send the reminder?”
Start asking:
- Did the patient improve?
- Did we reduce risk?
- Did we intervene early enough?
- Did we protect retention?
That shift turns follow-up from an operational task into a true ROI engine.
In the next sections, we will break down five practical, implementation-ready steps to transform follow-up from a checkbox into a competitive advantage. This also involves using automation where appropriate, embedding workflow integration, tracking outcomes rigorously, and empowering patients intentionally.
Because in outpatient care, continuity directly translates to margin.
5 Steps to Improve Clinic Patient Follow-Up Management
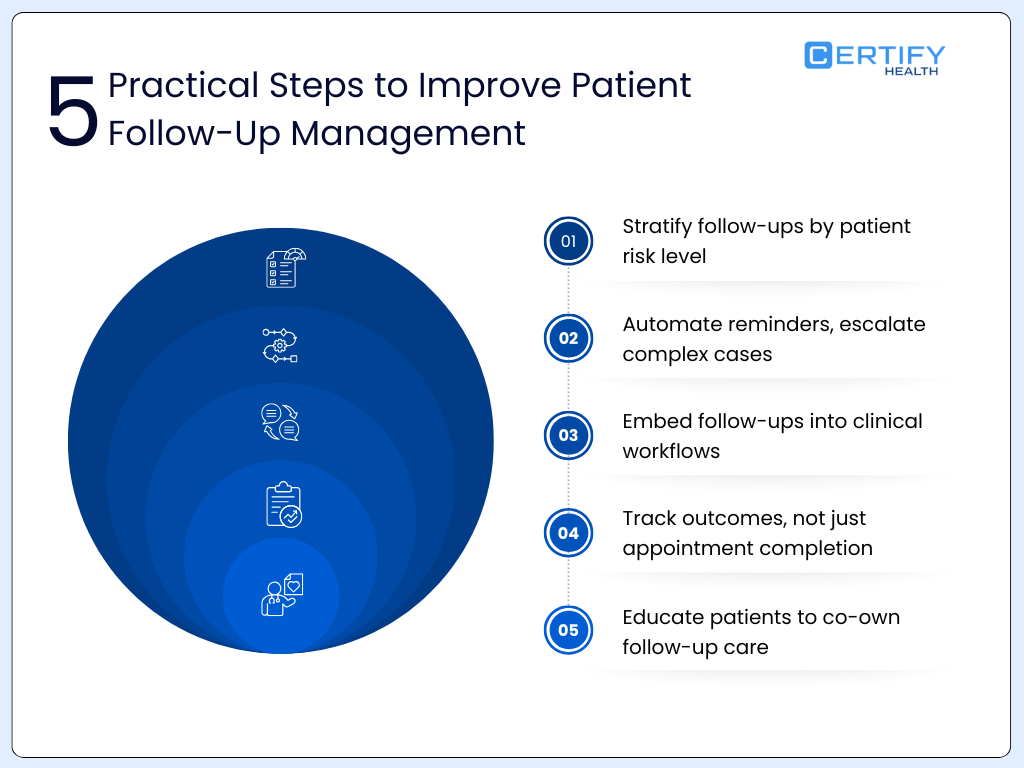
1. Define a Risk-Stratified Follow-Up Protocol
If follow-up is your ROI engine, risk stratification is the ignition system.
Not every patient benefits equally from early outreach. Research consistently shows that early outpatient follow-up after discharge is associated with lower 30-day readmission rates, particularly among older adults and high-risk cohorts.
For example:
- Studies in heart failure populations show 7-day follow-up is associated with 8–15% relative reductions in 30-day readmissions.
- Medicare data analyses suggest patients seen within 7 days of discharge have significantly lower readmission risk compared to those without early follow-up.
- However, the same magnitude of benefit is not observed in low-risk or younger cohorts, indicating diminishing returns when applied universally.
That means one thing:
Early follow-up works but only when applied intelligently.
Build Clear Risk Categories
Your follow up protocol should automatically classify patients into risk tiers at visit completion.
High Risk
- Recent hospitalization (≤30 days)
- ≥2 chronic conditions
- Heart failure, COPD, AMI, advanced diabetes
- Polypharmacy (>5 medications)
- Prior 30-day readmission
- Documented social instability
In Medicare populations with heart failure, baseline 30-day readmission rates can range from 20–25%. Early follow-up in this group shows the strongest risk reduction signal.
Moderate Risk
- Stable chronic disease
- Medication adjustment
- Recent ED visit
- Prior no-show history
Baseline readmission risk may be in the 10–15% range, with more modest benefit from intensive early follow-up.
Low Risk
- Preventive visits
- Minor acute issues
- Stable labs and vitals
Readmission risk typically <5%. Intensive follow-up adds little measurable clinical value.
Translate Risk into Cadence
| Risk Tier | First Follow-Up | Frequency | Channel | Clinical Review |
|---|---|---|---|---|
| High | 48–72 hrs | Weekly x 4 | Phone + clinician | Mandatory |
| Moderate | 5–7 days | Biweekly | Telehealth/Phone | Conditional |
| Low | 14–30 days | Standard cycle | Automated | No |
The mistake most clinics make is applying high-intensity outreach to everyone.
That increases staffing burden without proportional clinical return.
Research does not support universal high-touch models. It supports targeted early follow-up for high-risk patients.
Treating every patient the same wastes time and resources. Use risk and evidence (not convenience) to decide follow-up frequency.
Quantify the Impact
Consider the financial implication:
If your clinic manages 1,000 high-risk patients annually with a 20% readmission rate:
- 200 readmissions
- Even a conservative 10% relative reduction = 20 prevented readmissions
- At an average cost of $12,000–$15,000 per readmission
That’s $240,000–$300,000 in avoided cost exposure, before factoring quality incentives.
Risk-stratified follow up management clearly supports cost containment and quality strategy combined.
2. Automate What Makes Sense, Humanize What Matters
Automation is necessary for scale, but it is not a clinical substitute.
Many promote automation as the silver bullet for improving appointment attendance, patient satisfaction, and adherence rates.
Automation helps. It does not replace clinical oversight.
What Healthcare Automation Does Well
Studies show automated reminders can:
- Improve appointment attendance by 15–25%
- Reduce no-show rates by 20–30%
- Improve medication adherence modestly when combined with education
Automation is particularly effective for:
- Appointment reminders
- Preventive care nudges
- Routine lab follow-ups
- Educational messages
- Portal engagement prompts
When integrated into a structured follow up workflow, automation ensures consistency and reduces administrative burden.
Where Healthcare Automation Fails
Complex patients do not respond predictably.
Patients with:
- Advanced chronic disease
- Polypharmacy
- Social instability
- Cognitive decline
- Low digital literacy
Require human contact.
Research in transitional care models shows that nurse-led follow-up interventions are associated with larger reductions in readmissions compared to reminder-only interventions.
The difference?
Clinical judgment.
Design an Escalation Framework
| Trigger | Escalation Action |
|---|---|
| Worsening shortness of breath | Same-day nurse review |
| Weight gain in HF patient | Provider notified |
| No response (high-risk) | Direct phone outreach |
| Abnormal lab result | Manual clinical review |
| Repeated missed reminders | Social risk screening |
The Balanced Model
High-performing clinics apply a hybrid model:
- Automation handles volume and standardization
- Humans manage instability and uncertainty
This model improves:
- Adherence rates
- Patient reported outcomes
- Early intervention timing
- Overall clinical benefits
And critically….it improves trust.
It is important make patients feel supported rather than automated.
Over-automation in follow-up creates false confidence.
If your dashboard says “messages sent” but your readmission rate is unchanged, you don’t have effective follow-up.
You have automated activity.
True follow up management requires:
- Risk alignment
- Human escalation
- Outcome tracking
- Continuous optimization
Automation scales operations, whereas human oversight protects outcomes. The clinics that balance both will outperform those chasing efficiency alone.
3. Integrate Workflow with Outcome Tracking (Not Just Task Lists)
Here’s where most patient follow up strategies break down:
They live in task lists.
A reminder is sent.
A checkbox is marked.
No one connects it to outcomes.
If follow-up does not connect to measurable outcomes in your EHR, it will drift into inconsistency.
Real-Time Visibility Is Non-Negotiable
Your EHR and dashboards should display, in real time:
- Follow-up status (scheduled, completed, missed)
- Risk tier assignment
- Readmission flags
- Patient-reported symptom responses
- Escalation triggers
- Time-to-intervention metrics
If your team must manually search for follow-up status, you have fragmentation.
High-performing clinics use embedded workflows where follow-up is automatically triggered at visit closure or discharge documentation.
Embed Follow-Up Into Clinical Templates
The simplest way to ensure consistency?
Make follow-up unavoidable.
When a provider completes a visit note, the template should require:
- Risk tier confirmation
- Follow-up timing selection (auto-suggested by protocol)
- Escalation pathway designation
This removes variability.
Research in care standardization repeatedly shows that structured templates reduce care variation and improve adherence to quality measures.
If follow-up lives outside the clinical template, it becomes optional.
Optional processes produce uneven outcomes.
Define Role Clarity to Prevent Leakage
Every step in your follow up workflow must have an owner and SLA (service-level agreement).
| Task | Role | Timeframe |
|---|---|---|
| Initial outreach | Care coordinator | 48–72 hrs (high-risk) |
| Symptom review | RN | Same day |
| Medication reconciliation | Nurse/Pharmacist | 48 hrs |
| Escalation decision | Provider | 24 hrs |
| Documentation | Assigned staff | Immediate |
Ambiguity increases delay, and delay increases risk.
Studies in transitional care models show that structured, nurse-led follow-up programs with defined accountability reduce readmissions more effectively than unstructured outreach models.
Clear ownership improves both efficiency and safety.
Close the Loop With Outcome Tracking
A complete outcome tracking loop looks like this:
The gist here is closed-loop.
If the system ends at “message sent,” measurement of effectiveness is not in place.
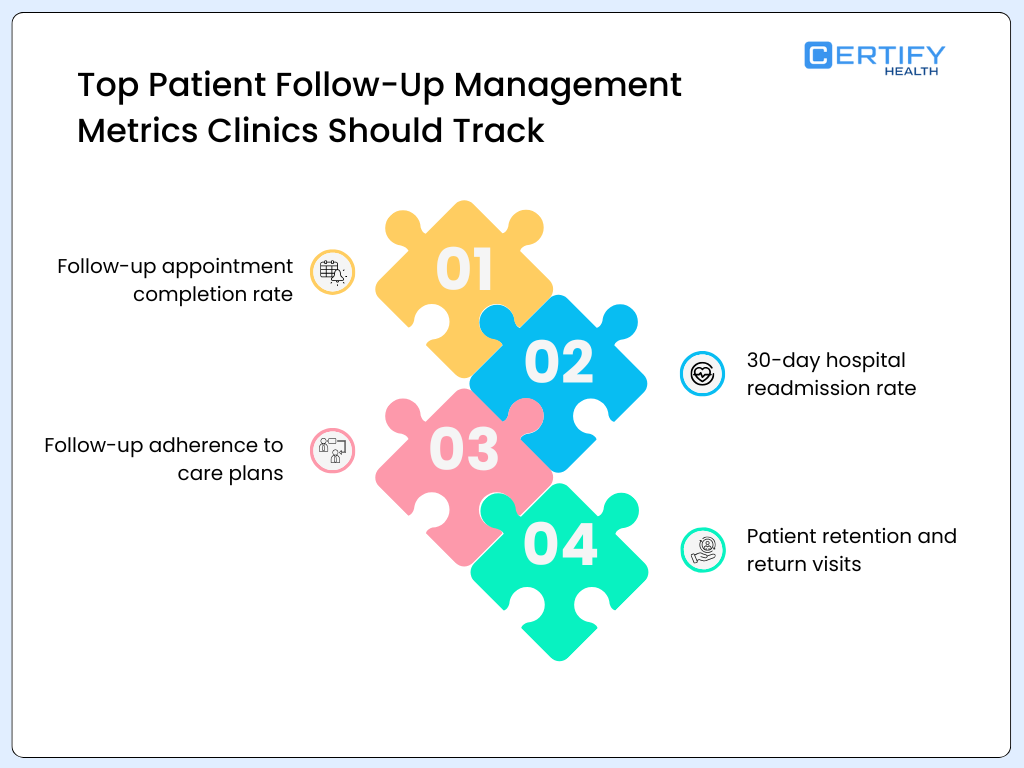
4. Measure What Matters (Beyond Appointment Attendance)
Attendance is a process metric.
Many clinics proudly report improved appointment attendance after implementing reminder systems.
That is useful but insufficient.
Meta-analyses evaluating transitional care and follow-up interventions consistently use endpoints such as:
- 30-day readmissions
- Mortality rates
- Emergency department revisits
Not “messages sent.” Not “calls completed.”
If your measurement framework doesn’t align with evidence-based endpoints, it lacks credibility.
Core Metrics That Drive Clinical and Financial Impact
| Metric | Why It Matters |
|---|---|
| Follow-up adherence rates | Indicates continuity strength |
| 7-day readmission rate | Early instability marker |
| 14-day readmission rate | Medium-term stabilization |
| 30-day readmission rate | CMS benchmark |
| Patient reported outcomes (PROs) | Functional improvement |
| Time to intervention | Responsiveness measure |
| Patient satisfaction | Retention & reimbursement predictor |
For example:
- Baseline heart failure readmissions often range from 20–25% within 30 days.
- Even a 5–10% relative reduction through structured follow-up translates into significant cost avoidance and quality score improvement.
Additionally, research shows improved medication adherence correlates with lower hospitalization rates and improved chronic disease control.
Follow-up must influence adherence.
If it doesn’t, it’s underperforming.
Time-to-Intervention Is the Hidden Metric
One overlooked KPI is time between:
- Patient-reported symptom
- Clinical review
- Intervention
Delays increase complication risk.
Faster response improves outcomes.
Measure it.
If your high-risk patient reports worsening symptoms and intervention happens 72 hours later, the system failed (even if the reminder was sent on time.)
Attendance isn’t the goal; clinical improvement is. Measure what moves health, not what moves calendars.
5. Empower Patients with Education and Shared Decision-Making
The most overlooked dimension of follow up management is patient psychology.
Patients who understand why follow-up matters engage differently than those who see it as an obligation.
Explain the “Why” Behind Follow-Up
Instead of saying:
“We’ll see you in a week.”
Say:
“Early follow-up reduces complications and helps us catch problems before they require hospitalization.”
Framing changes behavior.
Research shows that patients who understand the rationale behind care plans demonstrate higher adherence rates and improved engagement.
Provide Access, Not Just Instructions
To truly empower patients, enable:
- Portal access to labs
- Visit summaries
- Medication lists
- Educational materials
- Structured self-management resources
Patients managing chronic disease benefit from:
- Clear symptom thresholds
- Weight monitoring instructions (HF)
- Glucose tracking (diabetes)
- Action plans
Access builds accountability.
Make Follow-Up Part of a Personal Care Plan
High-performing clinics convert follow-up into a shared contract:
| Component | Example |
|---|---|
| Clear expectations | “We’ll check in within 72 hours.” |
| Symptom triggers | “Call us if weight increases by 2 lbs in 24 hrs.” |
| Monitoring plan | “Track BP daily for 14 days.” |
| Next milestone | “Reassess labs in 30 days.” |
This shifts follow-up from passive reminder to active engagement.
Many clinics send reminders.
Few integrate:
- Risk stratification
- Workflow integration
- Outcome tracking
- Patient education
- Shared decision-making
That integration improves:
- Patient satisfaction
- Long-term patient retention
- Documented clinical benefits
- Overall quality performance
Follow-up should feel like a partnership.
And partnership is what sustains outcomes over time.
Structure it deliberately. Measure it rigorously. Humanize it intelligently.
That’s how follow-up becomes your clinic’s real ROI engine.
Implementation Playbook: Turning Follow-Up Strategy Into Operational Discipline
Strategy without execution is noise.
If your clinic is serious about improving patient follow up, reducing readmissions, increasing patient retention, and improving patient satisfaction, you need operational assets.
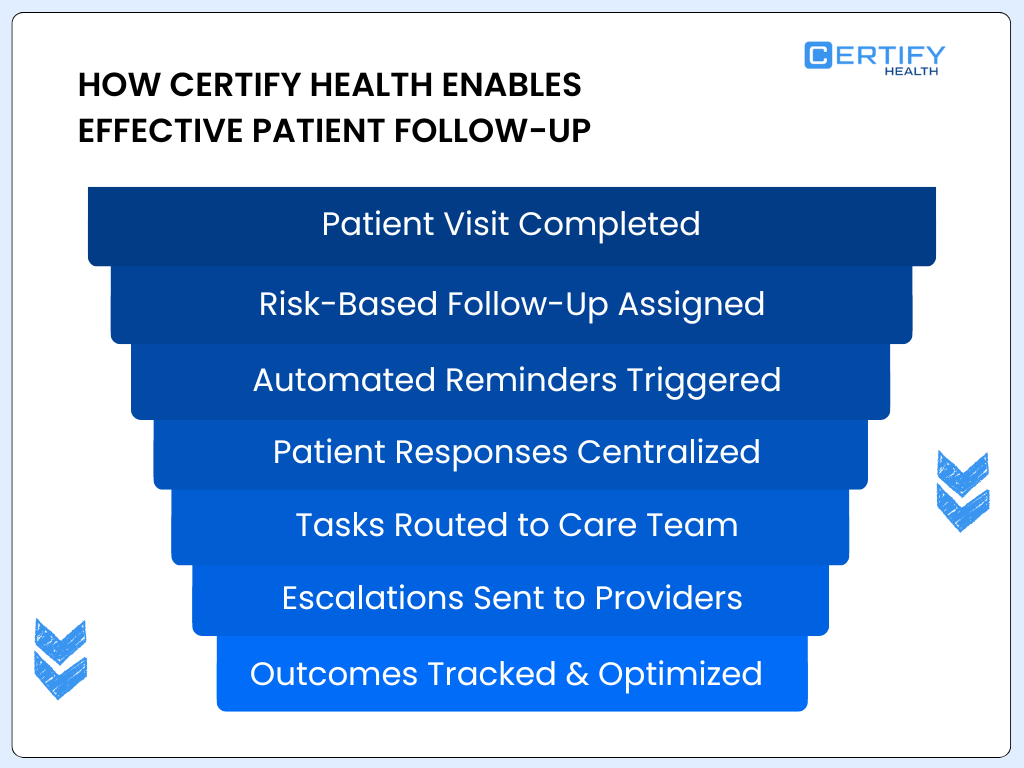
Below is a structured implementation playbook you can deploy immediately, and where relevant, how a unified platform like www.certifyhealth.com enables this system at scale.
1. Follow-Up Timing Matrix (Risk-Based Template)
Your follow up protocol must be codified.
Here is a structured timing matrix you can adapt:
| Condition | Risk Tier | First Contact | Follow-Up Frequency | Channel | Owner |
|---|---|---|---|---|---|
| Heart Failure | High | 48 hrs | Weekly x 4 | Phone + clinician | RN + Provider |
| COPD | High | 72 hrs | Weekly x 2 | Phone | RN |
| Diabetes (unstable) | Moderate | 5–7 days | Biweekly | Telehealth | Care Manager |
| Post-ED visit | Moderate | 5 days | 1–2 touchpoints | Phone | Care Coordinator |
| Preventive Visit | Low | 14–30 days | Standard | Automated | Admin |
Operational Rule:
Risk tier must auto-populate in the EHR at visit completion.
With a platform like Certify Health’s unified workflow system, risk triggers can automatically generate:
- Follow-up tasks
- Reminder schedules
- Escalation flags
- Role assignments
No spreadsheets.
No manual reminders.
No lost patients.
2. Sample Follow-Up Script Templates (High-Risk)
Standardization improves quality and protects consistency.
Below is a structured high-risk patient script.
High-Risk Phone Script (48–72 Hour Post-Discharge)
Step 1: Identity Confirmation
- “Hi [Name], this is [Clinic Name]. I’m calling to check in after your recent visit.”
Step 2: Medication Reconciliation
- “Have you filled your prescriptions?”
- “Any difficulty taking them as instructed?”
Step 3: Symptom Assessment
- “Have you noticed worsening shortness of breath?”
- “Any new swelling, dizziness, or chest discomfort?”
Step 4: Social Barrier Screening
- “Do you have transportation for your next visit?”
- “Any difficulty affording medications?”
Step 5: Reinforce Plan
- “Your next appointment is on [date]. It’s important because…”
Step 6: Escalation
- Trigger escalation if red flags identified.
Structured documentation within an integrated system (like Certify Health’s patient engagement and intake modules) allows:
- Real-time symptom logging
- Automatic flag generation
- Provider alerts
- Documented intervention timing
This is how you improve time to intervention, not just documentation.
3. EHR Workflow Steps (Embedded)
Follow-up must be embedded into your clinical workflow.
Here’s the step-by-step architecture:
Step 1: Visit Completion Trigger
- Risk tier auto-calculated
- Follow-up timing auto-generated
Step 2: Task Creation
- Assigned to defined role
- SLA countdown begins
Step 3: Outreach Execution
- Automated reminder OR
- Manual phone call based on risk
Step 4: Response Logging
- Structured data capture (not free-text)
- Escalation logic activated
Step 5: Intervention Documentation
- Medication change
- Earlier visit scheduled
- Telehealth consult
Step 6: Outcome Update
- Readmission flag
- PRO score update
- Satisfaction survey
With Certify Health’s unified healthcare platform, these steps are integrated into one operational backbone, aligning:
- Intake
- Patient communication
- Care coordination
- Revenue cycle workflows
- Outcome tracking
This eliminates fragmented systems and manual reconciliation.
Follow-up becomes measurable.
4. Dashboard & KPI Definitions (Outcome-Driven)
Dashboards should move beyond reminders sent.
Here’s what leadership should review weekly:
| KPI | Target | Why It Matters |
|---|---|---|
| % High-Risk Contacted ≤72 hrs | ≥90% | Prevent instability |
| Follow-up adherence rates | ≥85% | Engagement strength |
| 7-Day Readmission | Decreasing trend | Early failure signal |
| 30-Day Readmission | Below baseline | CMS impact |
| Time-to-Intervention | <24 hrs | Responsiveness |
| Patient Reported Outcomes (PROs) | Improving trend | Functional gain |
| Patient Satisfaction | ≥4.5/5 | Retention driver |
Clinical meta-analyses evaluating transitional care programs consistently use:
- 30-day readmissions
- Mortality
- ED revisits
Your dashboard must mirror those endpoints. Anything else is cosmetic measurement.
Certify Health enables integrated dashboards combining:
- Follow-up status
- Financial impact
- Quality metrics
- Patient engagement metrics
One system. One source of truth.
Common Pitfalls — And How to Avoid Them
Even strong strategies fail without discipline.
Let’s break down the most common failure points.
1. Ignoring Social Barriers
You can’t improve adherence rates without addressing social determinants.
- Transportation.
- Cost.
- Caregiver limitations.
- Health literacy.
Research shows social risk factors significantly increase readmission risk, independent of medical complexity.
Solution:
- Embed social screening into follow-up scripts
- Flag transportation or affordability concerns
- Route high-risk cases to care coordination
Certify Health’s intake and communication modules can capture structured social risk inputs. This allows proactive intervention instead of reactive crisis management.
2. Over-Automation Without Human Fallbacks
Automation improves appointment attendance by 15–25%.
But it does not manage clinical instability.
If a high-risk patient doesn’t respond to reminders and no human reviews that non-response, your system failed.
Solution:
- Hard-coded escalation triggers
- Non-response alerts for high-risk tiers
- Mandatory nurse review for flagged symptoms
Automation scales operations.
Human oversight protects outcomes.
3. Poor Role Clarity
Ambiguity destroys workflow.
If follow-up responsibility is shared loosely between front desk, MA, and nurse, gaps emerge.
Solution:
- Assign role + SLA
- Audit weekly
- Tie accountability to dashboard review
Integrated workflow platforms eliminate ambiguity by auto-assigning tasks and tracking completion status visibly.
4. Measuring Vanity Metrics
Tracking “messages sent” or “calls attempted” is not meaningful.
The only metrics that matter:
- Reduced readmission
- Improved PRO scores
- Increased patient satisfaction
- Stabilized chronic disease indicators
If your follow-up does not change outcomes, it is operational noise.
Conclusion: Follow-Up Is Clinical Quality Management
Let’s be clear:
Patient follow-up is not administrative.
It is:
- Risk mitigation
- Outcome optimization
- Revenue protection
- Patient loyalty infrastructure
- Clinical quality management
When engineered properly, structured follow up management:
- Reduces 30-day readmissions
- Improves patient reported outcomes
- Strengthens adherence rates
- Increases patient retention
- Enhances CMS quality performance
When treated casually, it increases variability, cost, and reputational risk.
The difference lies in:
- Risk stratification
- Workflow integration
- Intelligent automation
- Real-time outcome tracking
- Patient empowerment
A unified system like CERTIFY Health enables clinics to connect patient engagement, care coordination, and quality analytics in one operational backbone, thereby eliminating silos and converting follow-up into measurable impact.
In modern outpatient care, continuity is not a courtesy.
It is strategy.
Build it deliberately.
Measure it rigorously.
Optimize it continuously.
That’s how follow-up becomes your clinic’s true ROI engine.