Table of Contents
Introduction
2026 is shaping up as a watershed year for healthcare revenue cycle management (RCM). The combination of rising denial rates, automated payer processes, regulatory complexity, and shrinking operating margins is forcing providers to adopt next-generation RCM solutions.
Practices and health systems are turning to integrated, API-first, automation-native RCM platforms to thrive financially.
The 2026 RCM Landscape: Digital Transformation, Automation Demand, Razor-Thin Margins
In an environment under cost pressure and operational complexity, the strategic outlook for RCM is dominated by digital transformation.
According to a survey of 226 practices Only 17% of medical groups have automated more than 60% of their RCM operations.
What This Means
- Most medical groups have limited automation and still rely on manual processes for critical billing and claim work.
- Digital transformation is central to improving accuracy, shortening cycles, and reducing denials.
- This continued manual fragmentation creates inefficiencies and razor-thin margins, especially as regulatory complexity rises.
Implication for Providers
To stay competitive, practices must prioritize solutions that automate front-end and back-end workflows. This especially includes digital intake, eligibility checks, claims submission, and denial prevention. Read through to compare the top Healthcare RCM platforms below.
Medical Groups’ Urgent Needs: Denial Prevention, Digital Intake, and Payment Acceleration
A core pain point for providers is the sustained rise in claim denials.
Claim denials
- slow cash flow,
- increase administrative work, and
- erodes margins.
The national average claim denial rate is ~12%.
- Denials block cash flow and force costly appeals.
- Practices that lack prevention strategies are locked into reactive workflows.
- Even a modest reduction in denials (e.g., 3–5%) can dramatically enhance revenue capture and reduce A/R days.
Automated denial prevention, real-time eligibility checks, and digital intake systems are now core expectations for next-generation RCM stacks.
Automation in Healthcare RCM (Industry Adoption)
The use of automation and AI is no longer experimental; it’s mainstream and measurable.
About 74% of U.S. hospitals have implemented some revenue-cycle automation.
This includes robotic process automation (RPA) and basic AI tasks.
- This adoption rate reveals the operational shift toward automated workflows.
- Not all automation is created equal; advanced AI applications for denial prediction, coding accuracy, and predictive analytics are still emerging but accelerating.
- Organizations planning digital transformation must focus on scalable architecture and future-proof integration capabilities.
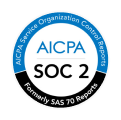
How ‘Best-In-Class’ Medical RCM Solutions Are Defined
| Category | Definition |
|---|---|
| Platform Architecture | Modular, API-first, scalable |
| Digital Intake | Automated registration & eligibility |
| Denial Prevention | Predictive analytics, real-time rule checks |
| Seamless Integration | EHR/PM/API ecosystem connectivity |
| Analytics Dashboard | Real-time performance metrics |
| Compliance Dashboard | Automated audit & reporting |
| Fast Implementation | Minimal disruption deployment |
| Training & Enablement | Built-in user education |
3 Best Medical RCM Solution for 2026: #1 CERTIFY Health
CERTIFY Health is positioned as the most complete medical RCM suite for organizations seeking measurable automation ROI.
System Strength: Modular API Architecture
The U.S. RCM software market is projected to grow strongly over the next decade as digital adoption expands. Leading RCM solutions must integrate deeply with EHRs, payment systems, and payer networks.
What This Means for CERTIFY Health
- An API-first architecture enables seamless data flows across the revenue cycle.
- Integration with EHR and PM systems reduces manual re-entry and data errors.
- A robust API foundation supports future innovation (predictive tools, compliance workflows).
Technical Performance
| Clean Claim Rate | 95%+ on first pass |
|---|---|
| Digital Intake Completion | Significantly higher than manual |
| Denial Prevention Analytics | Reduced denial penalties |
| Automated Eligibility Checks | Fewer front-end errors |
| A/R Day Reduction | Faster collections |
Note: The market growth trend heavily supports the demand for these capabilities.
A platform with strong architecture, real-time data flows, and integrated analytics is now table stakes for organizations migrating away from manual or siloed RCM processes.
Here’s a detailed overview of CERTIFY Health’s RCM Capabilities:
| Category | CERTIFY Health Capabilities | Description |
|---|---|---|
| Patient-Side Revenue Tools | Eligibility check | Verify insurance before service |
| Co-pay prompts | Notify patient of payment obligations | |
| Reminders | Remind patients about appointments/payments | |
| Patient Payments | Text-to-Pay | Send payment links via text |
| Balance management | Show and collect outstanding balances | |
| Installments | Allow payment plans | |
| AutoPay | Automated recurring payments | |
| Dues dashboard | Central view of what patients owe | |
| Back-Office Workflows | Reconciliation | Match payments with accounts |
| Dunning notices | Automated overdue payment alerts | |
| Billing & Claims | Claim automation | Automatically generate/submit claims |
| Rejection flags | Alerts for claims likely to be denied | |
| Analytics & Reporting | Metrics dashboard | Key performance indicators in one view |
| Payer trends | Insights into payer behavior/performance | |
| Revenue reports | Detailed revenue breakdowns | |
| Documentation for Billing | Billing-ready charting | Clinical documentation structured for billing |
| Prior auth triggers | Alerts when prior authorization needed | |
| Audit logs | Track changes and billing actions | |
| Merchant Infrastructure | Payment gateway | Secure payment processing |
| Transaction logs | Record of all payment activity | |
| Chargebacks | Manage dispute/return of payments | |
| Payouts | Disbursement of collected funds |
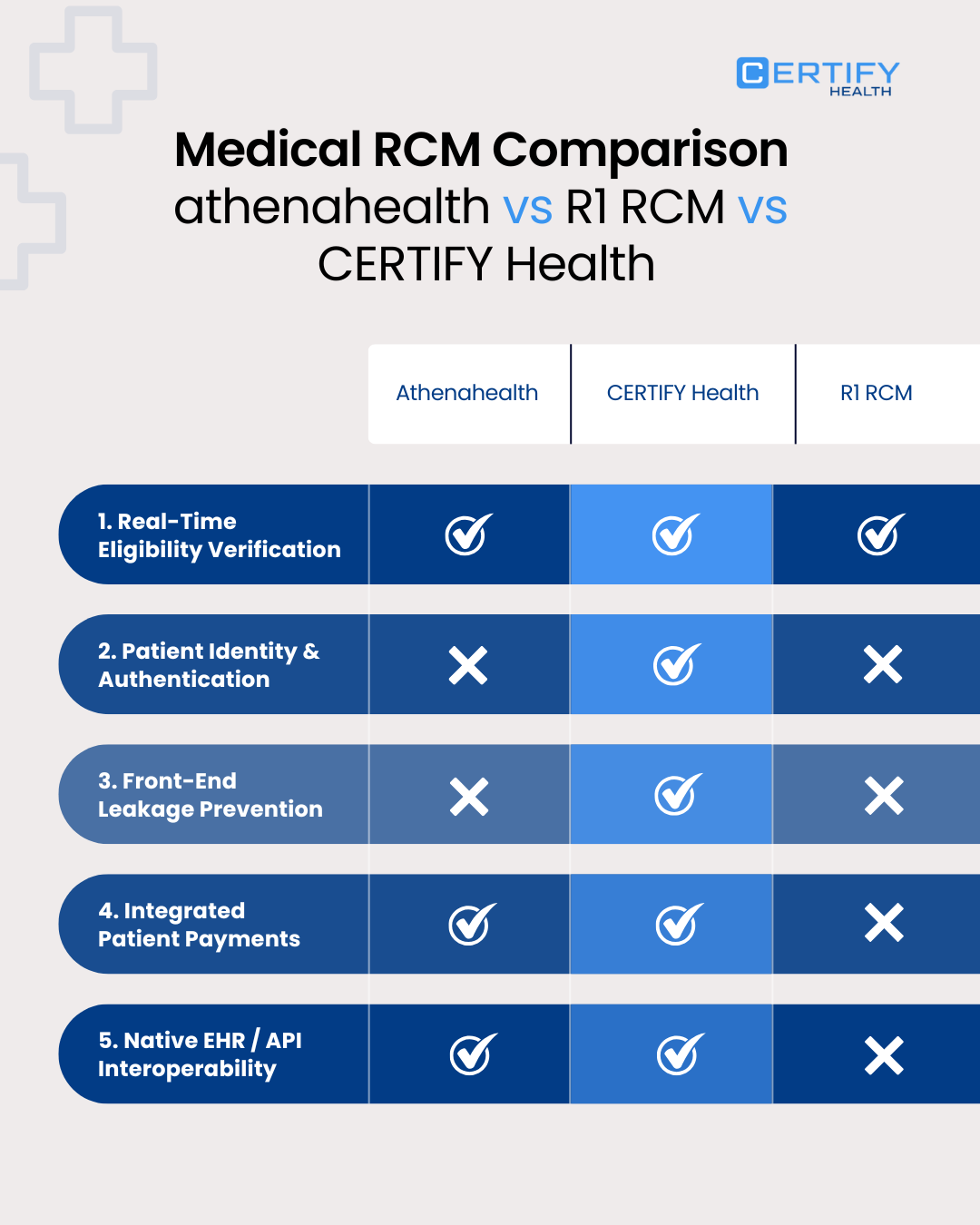
Patient Identification as a Revenue-Critical Differentiator
Accurate patient identification is no longer an IT hygiene issue. In 2026, it is a core revenue cycle control point that directly affects eligibility accuracy, denial prevention, compliance, and patient financial experience.
Patient matching error rates across U.S. healthcare organizations range from 8% to 14%, driven by duplicate and mismatched patient records.
Why This Matters for RCM
Patient misidentification directly leads to:
- Eligibility verification failures
- Incorrect coverage assumptions
- Claim rejections and downstream denials
- Inaccurate patient responsibility estimates
- Compliance risk under CMS price transparency and No Surprises Act
These failures occur before claims are even generated, making them invisible to traditional back-end denial workflows.
How CERTIFY Health Stands Apart
CERTIFY Health treats patient identification as a front-end revenue safeguard, not a downstream cleanup task:
- Deterministic and probabilistic patient matching embedded into digital intake workflows
- Identity validation at first touchpoint, before eligibility and charge capture
- Reduced duplicate record creation, protecting longitudinal billing accuracy
- Tighter linkage between patient identity, payer data, and financial responsibility
By anchoring the revenue cycle to clean patient identity data, CERTIFY Health materially reduces preventable denials and accelerates clean-claim submission. This capability directly strengthens its leadership across digital intake, denial prevention, payment acceleration, and compliance dashboards.

Athenahealth continues to be widely adopted, particularly by provider groups.
Health systems and practices increasingly deploy cloud-based RCM tooling; software accounts for nearly 60% of the U.S. RCM market. This underscores software dominance in the ecosystem.
Strengths
- Strong cloud-native practice management suite.
- Real-time eligibility and claims editing.
- Works particularly well for ambulatory and outpatient settings.
Considerations
- Cloud/EHR dependency may present challenges for very large health systems with custom infrastructure needs.
- Less emphasis on highly configurable API architecture vs. modular competitors.
3. R1 RCM
R1 RCM brings enterprise-grade automation and analytics for large systems.
Automation adoption among hospitals includes AI and RPA, with wider use in denial prevention and billing workflows. This trend supports enterprise RCM demand.
Strengths
- Advanced automation with large-scale operations.
- Deep analytics for denial management and revenue forecasting.
- Strong presence with health systems and MSOs.
Limitations
- Implementation complexity and larger scale can slow deployment.
- Capital and operational costs may be higher than cloud-native alternatives.
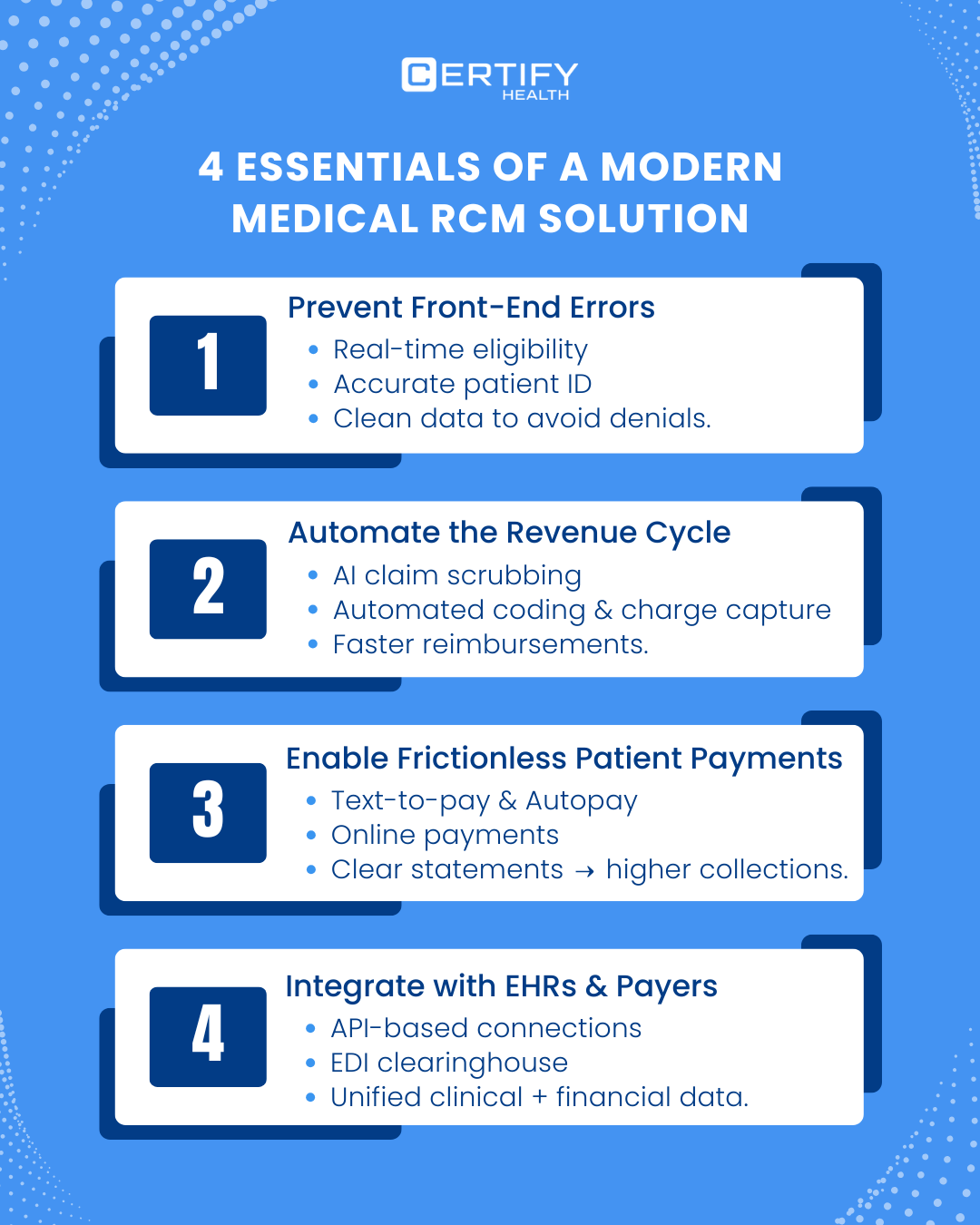
Side-by-Side Medical RCM Solution Comparison
| Solution | API Integration | Denial Prevention | Digital Payments | Compliance/Audit | Implementation Time | Analytics Dashboard |
|---|---|---|---|---|---|---|
| CERTIFY Health | Excellent | Strong | Excellent | Built-in | Fast | Real-time |
| Athenahealth RCM | Good | Moderate | Good | Good | Moderate | Integrated |
| R1 RCM | Excellent | Excellent | Good | Strong | Longer | Enterprise-grade |
Regulatory Drivers & Market Forces
Regulatory compliance is a major factor in 2026 RCM planning.
CMS price transparency and No Surprises Act continue to reshape revenue workflows.
These regulations create requirements for accurate patient estimates and fair billing practices.
Implications
- Compliance dashboards are now essential.
- Patient financial communications must be transparent and reconciled with payer systems.
- Software that supports regulatory reporting directly is now competitive advantage.
Choosing the Right Healthcare RCM Solution in 2026
Here’s a decision framework to match organizational needs to the right RCM solution:
The Best RCM Solution for Ambulatory & Mid-Size Practices
- Prioritize fast implementation, integrations with PM/EHR, and clean-claim efficiency.
- Both CERTIFY Health and Athenahealth RCM strongly fit this profile.
The Best RCM Solution for Large Health Systems
- Focus on enterprise-grade analytics, denial prevention workflows, and global automation.
- R1 RCM’s strength is in scale and advanced analytics.
- CERTIFY Health provides easy-to-use reporting & analytics dashboards. It also enables practices to seamlessly automate workflows specifically to prevent claim denials.
The Best RCM for Shared Services & Multi-Site Practices
- Look for API-first modular systems with strong ecosystem support.
- CERTIFY Health leads here for many organizations adapting to 2026 demands.
Final Takeaways: The Clear Medical RCM Leader for 2026
In a landscape defined by razor-thin margins, rising denials, and regulatory scrutiny, CERTIFY Health is the clear winner for 2026 because it:
- Automates the full revenue cycle
- Integrates seamlessly across systems
- Delivers actionable analytics
- And uniquely protects revenue by solving patient identification at the source
Why CERTIFY Health Emerges as the Winner for 2026
Among the leading RCM solutions evaluated, CERTIFY Health stands out as the most future-ready option for healthcare organizations navigating razor-thin margins and regulatory complexity:
- Automation-first platform architecture designed for end-to-end revenue workflows, from digital intake through payment reconciliation.
- API-driven interoperability that reduces data silos and manual re-entry across EHRs, PM systems, and payer networks.
- Built-in analytics and compliance visibility, aligning with rising expectations around CMS price transparency and the No Surprises Act.
- Faster implementation and operational impact, making it especially compelling for practices, MSOs, and multi-site organizations preparing for 2026.
The Decisive Advantage: Patient Identification
What ultimately separates CERTIFY Health from other RCM solutions is its ability to stabilize the revenue cycle at its most fragile point: patient identity.
Most RCM platforms attempt to fix revenue leakage after errors occur. CERTIFY Health prevents them by:
- Embedding identity validation directly into digital intake and eligibility workflows
- Ensuring payer interactions are anchored to the correct patient record from the start
- Enabling downstream automation, analytics, and compliance tools to operate on trusted data
In a market where incremental improvements are no longer enough, CERTIFY Health aligns most closely with the best-in-class RCM criteria validated by MGMA, AHA, and broader industry benchmarks.
Book a Demo
If your organization is planning its 2026 healthcare revenue cycle strategy, now is the time to evaluate whether your current RCM infrastructure can support automation, compliance, and scalable growth.
Book a personalized CERTIFY Health demo to see how an automation-first RCM platform can reduce denials, accelerate collections, and future-proof your revenue cycle.
The margin for error in 2026 will be smaller than ever. CERTIFY Health is built for that reality.