Table of Contents
OB-GYN practices face mounting financial pressure: burnout rates as high as 40–75%, billions lost annually to claims denials, staffing shortages in rural obstetrics, and operational drag from legacy IT silos. Administrative overload, scheduling waste, authorization delays, and documentation gaps directly impact revenue and patient access.
A structured adoption framework grounded in proven change models [Technology Acceptance Model (TAM) and Consolidated Framework for Implementation Research (CFIR)] helps decision-makers modernize without disruption.
CERTIFY Health delivers a unified platform that connects patient experience, scheduling, interoperability, and revenue workflows into one coordinated system, reducing denials, minimizing verification errors, reclaiming 15–25 staff hours weekly, improving scheduling by 20–30%, and accelerating collections within 60–90 days.
Your OB-GYN practice is already working hard. It’s time your systems did too.
Let’s map your 12-week revenue recovery plan and show you exactly where operational waste is hiding.
OB-GYN Practice's Burning Pain Points: Stats Don't Lie
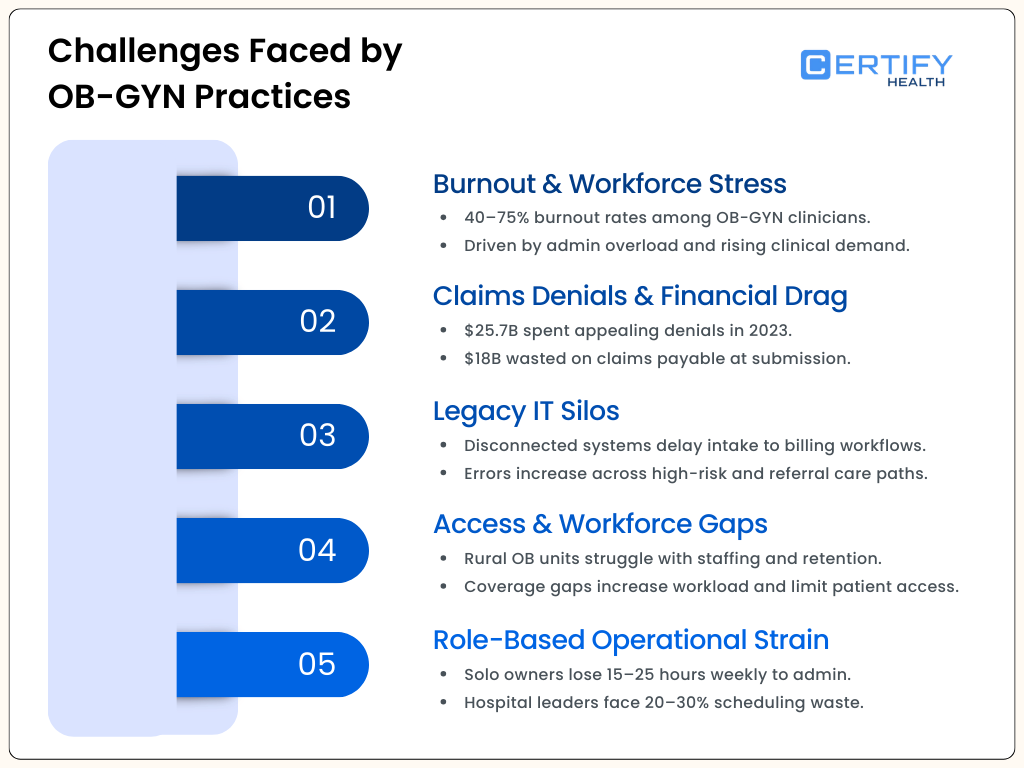
Burnout and Workforce Stress
Burnout is pervasive among OB-GYN clinicians, with specialty burnout rates reported as high as 40–75%, among the highest in medicine, driven by administrative burden and clinical demand.
Claims Denials and Financial Drag
Claims denials remain a major financial headwind for practices and health systems — providers spent an estimated $25.7 billion contesting denials in 2023, and nearly $18 billion was potentially wasted overturning claims that should have been paid at submission.
Legacy IT Silos Impair Care
Legacy IT silos slow care handoffs from intake to diagnostics and billing, exacerbating errors and delays in complex OB-GYN care pathways, from high-risk prenatal monitoring to subspecialty referrals.
Access & Workforce Distribution Gaps
Rural and low-volume hospitals face ongoing staffing challenges: nearly all surveyed rural obstetric units reported difficulty scheduling and retaining clinicians, maintaining training competencies, and covering fluctuating patient volumes. In these settings, clinician shortages can limit access and increase workload stress.
Decision-Makers Bear the Brunt Differently
In OB-GYN solo practices or menopause-focused GYN clinics, the decision maker role often falls on the physician-owner, who may lose 15–25 hours weekly to admin burdens like intake and verification errors.
Hospital CMOs or admins in large OB-GYN groups wrestle mounting financial pressures, 20-30% scheduling waste and fragmented OB-GYN Billing systems, while billing directors face $25-181 per denial rework in complex FPMRS or oncology billing.
Subspecialty chiefs in REI OB-GYN clinics deal with delayed consents and high-risk tracking, all amid post-Dobbs compliance stress.
For full insights into go through our: U.S. Women’s Healthcare Market 2025: Demand Drivers, Technology Shifts & Growth Outlooks
Ready to cut through this?
Schedule a quick CERTIFY Health demo to see how unified platforms reclaim that time for OB-GYN patient care.
Tech Adoption Framework by OB-GYN Practice Size, Type, & Specialty
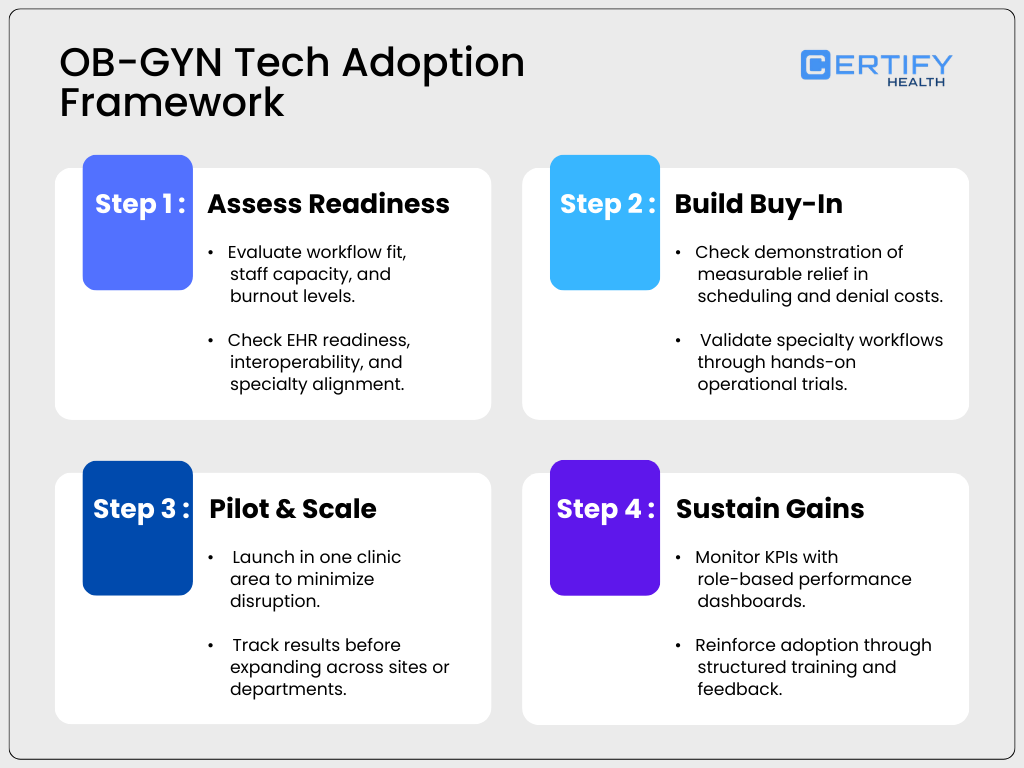
Adopting a unified platform isn’t about shiny new tools, it’s about easing perceived effort and proving real value, straight from the Technology Acceptance Model (TAM). TAM shows OB-GYN providers embrace tech when it feels useful and user-friendly, much like EHR readiness studies where positive attitudes improve adoption by 4-5 times. Layer in the Consolidated Framework for Implementation Research (CFIR), which tailors rollout by assessing inner (staff buy-in), outer (payer rules), and innovation factors (interoperability) for OB-GYN hospitals or solo setups.
This four-step guide adapts TAM and CFIR for OB-GYN decision-makers, customized by practice type.
Step 1: Assess Readiness
Start with a gut check:
Does this unified platform fit your OB-GYN clinic’s daily grind without adding screens?
- For solo/private OB-GYN practices like menopause GYN, run a quick audit on admin overload—EHR readiness hovers at 50-56% in similar settings, tied to computer access and self-efficacy.
- Large OB-GYN hospitals need full compatibility scans across L&D and OBGYN billing depts.
- REI or MFM subspecialties match against risk-tracking needs.
- Hospitalists evaluate shift gaps; if burnout’s at 65%, prioritize effort-saving tools.
Step 2: Build Buy-In
Demos shouldn’t feel like sales presentations; they should give you proof of operational impact. When evaluating solutions, OB-GYN leaders should look for measurable front-desk relief (such as 20% fewer inbound scheduling calls), revenue modeling that reduces $25+ per-claim rework costs, and real fixes for specialty workflows like REI consents or oncology documentation flags.
- For hospital-employed groups managing L&D surges, hands-on trials should demonstrate how staff handle peak volumes without added burnout.
- Solo pediatric GYN practices may prioritize simplicity and ease of adoption, while FPMRS or subspecialty chiefs will want to see complex pelvic procedure workflows mapped accurately.
Adoption happens when teams see ease of use and real workflow alignment early. Trust is built through practical validation, not promises.
Step 3: Pilot and Scale
Start small to reduce risk and scale once you see results. Pilot new intake or workflow tools in one OB-GYN clinic area before expanding systemwide.
- For solo OB-GYN practices, short, focused trials help validate ease of use without disrupting daily operations.
- Medium-sized REI groups may benefit from department-by-department rollouts, beginning with high-friction areas such as FPMRS procedures.
- In hospital-based OB-GYN programs, involve hospitalists early to evaluate shift-based tools, and gather structured feedback from locum providers to ensure workflows hold up under variable staffing models.
Early adopters play a critical role in scaling success. When teams clearly see practical value and workflow alignment, adoption accelerates.
Track measurable outcomes, such as reducing no-show rates by 25% or more, to build internal momentum and support broader rollout decisions.
Step 4: Sustain Gains
Sustained Improvement Requires Visibility
Dashboards should keep performance front and center, with mobile-friendly KPIs for solo OB-GYN leaders and more advanced, role-based reporting for larger hospital teams.
Training Should Match Organizational Complexity
Simple onboarding for small practices, structured and ongoing education for multi-site groups. Specialty-specific needs, such as pediatric GYN consent workflows, should be built into the system, not treated as afterthoughts.
Over time, automated performance tracking helps reduce administrative strain and protect against burnout by minimizing manual follow-up and reporting. Long-term success depends on continued engagement, leadership alignment, and consistent workflow reinforcement.
Before Expanding Any Initiative, Assess Readiness
Are your teams aligned? Are workflows standardized? Are metrics clearly defined? A structured evaluation process is the first step toward sustainable OB-GYN practice efficiency.
Ready to see how this framework translates into real operational gains?
Schedule a personalized CERTIFY Health demo and walk through what it looks like inside your OB-GYN practice.
CERTIFY Health’s Unified Healthcare System: Successful Tech Adoption Framework for OB-GYN
About CERTIFY Health
CERTIFY Health is a unified healthcare platform that connects intake, scheduling, patient communication, interoperability, and revenue workflows into one coordinated system for the modern OBGYN practice.
It connects seamlessly with 100+ EHRs, practice management systems, billing platforms, lab tools, and internal applications, working alongside your current technology instead of replacing it. The result? Front office, clinical, and revenue teams operate from synchronized workflows with accurate, real-time data flowing across every touchpoint.
The goal is simple: reduce operational friction, ease operational overload, lower denials and no-shows, and improve staff productivity without disrupting care delivery amid growing financial pressures.
Applying the TAM–CFIR Playbook in OB-GYN
CERTIFY Health aligns with proven adoption principles rooted in the Technology Acceptance Model and Consolidated Framework for Implementation Research: demonstrate clear usefulness early, reduce implementation burden, and scale through internal champions.
As a plug-and-play unified platform for OB-GYN settings, from solo clinics to MFM-heavy hospital programs, it supports a structured 12-week rollout designed to deliver measurable early wins for every decision maker role.
Typical focus areas include reclaiming 15–25 staff hours per week, improving scheduling performance by 20–30%, and addressing common pain points such as eligibility verification errors and OBGYN billing and oncology billing silos.
Because the platform interoperates with systems, organizations can modernize workflows without a disruptive rip-and-replace strategy.
12-Week Acceleration Plan: A Phased Rollout Tailored to OB-GYN Specialty, Practice Model, and Scale
Weeks 1–2: Initiation & Tech Setup
Foundation Layer – Patient Experience + Operational Readiness
This phase is about alignment, baseline measurement, and removing obvious friction before scaling.
Assign Your OB-GYN Core Squad
Goal: Ensure both clinical and operational voices are represented.
Who to assign:
- OB Medical Director / Department Chair
- Billing or RCM Lead
- Front-desk / Access Supervisor
- Subspecialty Champion (MFM, REI, Oncology, FPMRS, etc.)
- Hospitalist Shift Lead (for L&D programs)
Why it matters in OB-GYN:
Care extends across prenatal appointments, surgical procedures, fertility treatments, oncology services, and Labor & Delivery, making seamless coordination between teams essential from the very start.
Baseline the OB-GYN Patient Access Experience
Focus Areas (Patient Experience Layer):
- Current no-show rate (prenatal, procedures, fertility consults)
- Self-scheduling availability
- Waitlist / high-risk pregnancy access delays
- Pediatric or minor consent workflows
- Pelvic surgery paperwork friction
What You’re Doing:
- Turn on patient experience dashboards
- Run a self-scheduling baseline report
- Audit digital intake and consent gaps
- Identify surge points (e.g., L&D peak days)
Outcome:
Clear picture of where access and engagement are breaking down.
Run an OB-GYN Readiness Scan (Operational Gear Check)
This is not full implementation; its assessment.
Clinical Workflow Review
- High-risk pregnancy flags correctly tracked in EHR?
- Fertility cycle documentation aligned with billing?
- Chemotherapy authorization workflows clean?
- Post-Dobbs exclusion alerts configured?
Revenue & Billing Review
- Denial hotspots (OB bundles, infertility, oncology billing)?
- Eligibility verification errors driving downstream OBGYN billing corrections?
- Surgery authorization delays?
- Pelvic procedure documentation gaps?
Shift & Coverage Review (Hospital Programs)
- Hospitalist coverage gaps?
- L&D surge days identified?
- Locum onboarding workflow friction?
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Specialty-Specific Quick Wins (Weeks 1–2 Only)
Instead of overwhelming teams, activate 1–2 relevant tools:
- MFM: High-risk tracking validation
- REI: Fertility cycle intake + insurance verification cleanup
- Gynecologic Oncology: Chemo billing flag baseline
- FPMRS: Standardize pelvic procedure consent
- Pediatric GYN: Minor intake checklist digitization
- Menopause / Solo: Simple online self-scheduling + Text-to-Pay
Week 3: Intake Rocket Launch – Patient Experience Platform Live
Connect OCR + Digital Forms Directly to the EHR
This phase focuses on eliminating manual scanning, minimizing verification errors, duplicate data entry, and intake bottlenecks by linking structured digital forms and OCR (optical character recognition) directly into OB-GYN workflows.
Primary Goal
- Intake documents automatically scan and populate the EHR
- Digital forms sync with scheduling, billing, and documentation systems
- Reduce re-keying errors across OB-GYN access and RCM workflows
Expected Early Wins
- Up to 85% patient satisfaction from faster check-in and fewer repeat forms
- Up to 13.5% reduction in billing errors caused by incomplete or mismatched intake data
Specialty-Specific Activation
Instead of activating everything at once, each OB-GYN setting focuses on its highest-friction paperwork first.
MFM (Hospital – Large)
Focus: High-risk pregnancy intake automation
Actions:
- Activate OCR for high-risk prenatal intake packets
- Ensure system auto-flags risk indicators from scanned documents
Team Tasks:
- L&D team monitors ER and surge-based intake scans
- Validate that risk factors populate correctly in prenatal charts
REI (Private Group – Medium)
Focus: Fertility cycle documentation integration
Actions:
- Digitize fertility consultation and cycle consent forms
- Connect digital forms to PMS and billing workflows
Team Tasks:
- Physicians test fertility intake flows
- Billing confirms insurance verification fields sync correctly
Gynecologic Oncology (Academic – Large)
Focus: Chemotherapy and research packet coordination
Actions:
- OCR-scan chemotherapy consent and patient education packets
- Link oncology intake forms with research documentation workflows
Team Tasks:
- Research coordinators validate data mapping
- Billing confirms chemo authorization details auto-populate
FPMRS / Urogynecology (Private – Medium)
Focus: Pelvic surgery documentation
Actions:
- CERTIFY Health digitizes pelvic surgery intake and consent forms into secure, mobile-friendly workflows, eliminating paper and manual scanning.
- Completed pre-op documents automatically sync with the connected EHR/PMS, ensuring they’re available in the patient record without duplicate data entry.
Team Tasks:
- Surgeons test documentation uploads
- Front desk verifies intake data reaches surgical billing correctly
Complex Family Planning (Hospital – Medium)
Focus: Regulatory-sensitive intake workflows
Actions:
- Configure structured digital intake with conditional alerts to surface regulatory-sensitive cases early and ensure complete consent documentation synced to the EHR.
- Ensure complete consent documentation synced to the EHR.
Team Tasks:
- Compliance team verifies regulatory safeguards
- Physicians confirm documentation completeness
Pediatric / Adolescent GYN (Solo / Small)
Focus: Minor-specific digital intake
Actions:
- Launch child-friendly digital intake forms
- Enable guardian e-signatures
Team Tasks:
- Practice owner validates mobile-friendly workflows
- Test reminder messaging for parents/guardians
Menopause / Geriatric (Locum / Variable)
Focus: Fast documentation and intake for older patients
Actions:
- Enable quick-scan intake for medication lists and history
- Simplify geriatric-friendly digital forms
Team Tasks:
- Locum providers test rapid mobile access
- Confirm intake data flows directly into EHR without manual re-entry
What Success Looks Like by End of Week 4
- Paper intake reduced or eliminated in priority specialty
- OCR feeds structured data into the EHR
- Fewer demographic and insurance errors
- Reduced front-desk scanning workload
- Billing team reports fewer intake-related claim corrections
Week 4: Eligibility & Consent Activation – Interoperability, FaceCheck, and Patient Management Integration
Real-Time Insurance Verification + HIPAA-Compliant Digital Consents + AI Charting Introduction
This phase focuses on reducing denials, preventing authorization delays, easing OB-GYN documentation burden in the modern OBGYN practice, and relieving ongoing financial pressures.
Primary Goals
- Enable real-time eligibility and authorization checks to reduce verification errors
- Ensure HIPAA-compliant digital consent capture
- Introduce AI-assisted documentation tools to reduce charting burden
Expected Early Wins
- $25–$181 per claim saved by reducing avoidable rework, denial appeals, and downstream OBGYN billing and oncology billing corrections
- Open up 5–7 additional appointment slots per provider through faster intake and reduced documentation time
Standardizing Clinical and Administrative Workflows
MFM (Academic – Medium)
Focus: High-risk pregnancy authorizations and documentation accuracy
Actions:
- Activate real-time authorization checks for high-risk prenatal services
- Introduce structured digital documentation templates for high-risk pregnancy tracking.
Team Tasks:
- High-risk OB team pilots charting for complex cases
- Review authorization turnaround times
REI (Subspecialty – Small)
Focus: Fertility cycle insurance verification and consent compliance
Actions:
- Enable automated insurance verification for fertility cycles
- Deploy consent documentation templates
Team Tasks:
- Physicians validate consent templates for IVF/IUI cycles
- Billing monitors verification accuracy rates
Gynecologic Oncology (Hospital – Large)
Focus: Chemotherapy authorization and billing alignment
Actions:
- Activate chemo-specific billing flags, eligibility verification, and safeguards against verification errors
- Use FaceCheck to validate patient insurance accuracy
Team Tasks:
- Billing team confirms through Epic integration data flow
- Oncology leads review authorization-to-treatment timelines
FPMRS / Urogynecology (Private – Medium)
Focus: Pelvic procedure authorizations and surgical documentation
Actions:
- Automate authorization tracking for pelvic procedures
- Deploy standardized digital procedure documentation templates.
Team Tasks:
- Surgeons customize templates to match documentation standards
- Billing tracks pre-op authorization completeness
Complex Family Planning (Hospital – Medium)
Focus: Regulatory-sensitive coverage and consent workflows
Actions:
- Configure plan-based exclusion alerts during eligibility checks
- Digitize HIPAA-compliant consent workflows
Team Tasks:
- Physicians test digital consent flows
- Compliance team validates documentation completeness
Pediatric / Adolescent GYN (Small Group)
Focus: Minor consent compliance
Actions:
- Activate guardian-specific digital consent workflows
- Verify insurance eligibility prior to appointment
Team Tasks:
- Families pilot mobile consent completion
- Front desk monitors reduction in check-in delays
Hospitalists / OB ER (Any Size)
Focus: Rapid eligibility checks + documentation efficiency
Actions:
- Activate real-time insurance verification at OB ER registration to reduce denials and prevent post-visit billing corrections.
- Implement structured digital documentation workflows to help hospitalists document triage and admissions more efficiently during shifts.
Team Tasks:
- Shift leads monitor patient flow impact
- Review documentation time reduction per provider
What Success Looks Like by End of Week 6
- Fewer authorization-related delays
- Reduced eligibility-related denials and fewer verification errors
- Digital consents replacing paper across priority services
- Providers reporting reduced documentation time
- Measurable cost savings per claim and improved OBGYN billing accuracy
Week 5: Scheduling Auto-Pilot – Practice Management Software Core
Practice Management Core Activation
This phase activates automated scheduling tools within the unified platform to reduce no-shows, fill cancellations instantly, fully synchronize provider calendars, and minimize operational overload for access teams.
Primary Goal
- Enable patient self-scheduling
- Activate ASAP waitlists to auto-fill cancellations
- Launch SMS-based confirmations and reminders
- Fully integrate calendars with EHR/PMS scheduling
Expected Fast Wins
- 25–35% reduction in no-shows
- 60–80% of cancelled appointments auto-filled
- Reduced front-desk call volume
- Faster access for high-demand OB-GYN services while easing operational overload
Specialty-Specific Activation
MFM (Hospital – Large)
Focus: Coordinating high-risk pregnancy access and Labor & Delivery coverage.
Actions:
- Activate priority waitlists for high-risk prenatal visits
- Auto-fill cancelled MFM consult slots from risk-based queues
Team Tasks:
- L&D leaders coordinate outpatient schedules with hospitalist shift planning to ensure seamless coverage.
- Monitor high-risk patient access times weekly
REI (Private Group – Medium)
Focus: Fertility cycle coordination and consult access
Actions:
- Implement shared fertility cycle calendars (retrievals, transfers, monitoring visits)
- Enable patient self-booking for consults and follow-ups
Team Tasks:
- Physicians define which visit types allow self-booking
- Staff validate cycle timing alignment with lab and procedure days
Gynecologic Oncology (Academic)
Focus: Post-treatment continuity
Actions:
- Auto-schedule post-chemotherapy follow-ups
- Activate SMS reminders for infusion and monitoring visits
Team Tasks:
- Teams configure follow-up protocols by treatment type
- Monitor missed post-chemo appointment rates
FPMRS / Urogynecology (Subspecialty – Small)
Focus: Surgical block utilization
Actions:
- Use ASAP lists to fill cancelled pelvic surgery blocks
- Enable automated reminders for pre-op and post-op visits
Team Tasks:
- Front desk trains on managing surgical waitlists
- Surgeons review unused OR (Operating room) block trends monthly
Pediatric / Adolescent GYN (Locum Model)
Focus: Family-friendly access flexibility
Actions:
- Enable 24-hour online scheduling access
- Activate family-focused SMS reminders
Team Tasks:
- Locum providers test mobile schedule access
- Staff monitor guardian confirmation rates
Menopause / Geriatric GYN (Solo Practice)
Focus: Simplicity and efficiency
Actions:
- Launch simple self-scheduling for consults and follow-ups
- Enable automated SMS reminders
Team Tasks:
- Practice owner defines appointment types available online
- Go live with minimal front-desk intervention
What Success Looks Like by End of Week 5
- Self-booking live for approved visit types
- ASAP waitlists actively filling cancelled slots
- SMS reminders reducing manual confirmation calls
- Calendar fully synchronized with EHR/PMS
- Measurable no-show reduction beginning to show
Week 6: Messaging Power-Up – Patient Experience Expansion
Patient Experience Expansion
This phase activates secure, two-way digital communication inside the unified platform, to reduce front-desk workload while increasing patient engagement and responsiveness.
Primary Goal
- Enable secure two-way patient messaging
- Launch automated replies for common questions
- Activate broadcast messaging for instructions and updates
- Reduce inbound phone traffic & alleviate operational overload
Expected Fast Wins
- Front-desk call volume drops significantly
- Faster response time for patient questions
- Higher engagement before and after visits
- Improved patient satisfaction scores
Specialty-Specific Activation
Family Planning (Hospital-Based)
Focus: Regulatory-sensitive communication and visit prep
Actions:
- Send pre-visit preparation instruction broadcasts
- Automate FAQs for common intake and documentation questions
Team Tasks:
- Physicians review and customize FAQ responses
- Admin teams schedule timed instruction messages before procedures
Pediatric & Adolescent GYN (Group – Small)
Focus: Parent/guardian engagement
Actions:
- Launch appointment “nudge” reminders for guardians
- Enable secure chats for follow-up questions
Team Tasks:
- Staff activate chat routing protocols
- Monitor guardian response and confirmation rates
Gynecologic Oncology (Large Hospital)
Focus: Post-treatment continuity
Actions:
- Send chemotherapy follow-up check-ins
- Broadcast symptom-monitoring reminders
- Enable secure post-infusion messaging
Team Tasks:
- Nursing team manages broadcast workflows
- Clinical team monitors flagged symptom responses
Hospitalists / OB ER (Any Size)
Focus: Labor & Delivery surge communication
Actions:
- Enable auto-replies for common L&D triage questions
- Activate surge-based messaging during peak admission hours
Team Tasks:
- Shift leads configure auto-reply templates
- Monitor inbound volume during high census periods
What Success Looks Like by End of Week 6
- Secure messaging live across web/SMS
- Auto-replies handling repetitive inquiries
- Broadcast messages supporting pre-op and post-care
- Front-desk phone dependency reduced, easing operational overload
- Improved patient satisfaction while protecting margins under continued financial pressures
Week 6: Messaging Power-Up – Patient Experience Expansion
Patient Experience Expansion
This phase activates secure, two-way digital communication inside the unified platform, to reduce front-desk workload while increasing patient engagement and responsiveness.
Primary Goal
- Enable secure two-way patient messaging
- Launch automated replies for common questions
- Activate broadcast messaging for instructions and updates
- Reduce inbound phone traffic & alleviate operational overload
Expected Fast Wins
- Front-desk call volume drops significantly
- Faster response time for patient questions
- Higher engagement before and after visits
- Improved patient satisfaction scores
Specialty-Specific Activation
Family Planning (Hospital-Based)
Focus: Regulatory-sensitive communication and visit prep
Actions:
- Send pre-visit preparation instruction broadcasts
- Automate FAQs for common intake and documentation questions
Team Tasks:
- Physicians review and customize FAQ responses
- Admin teams schedule timed instruction messages before procedures
Pediatric & Adolescent GYN (Group – Small)
Focus: Parent/guardian engagement
Actions:
- Launch appointment “nudge” reminders for guardians
- Enable secure chats for follow-up questions
Team Tasks:
- Staff activate chat routing protocols
- Monitor guardian response and confirmation rates
Gynecologic Oncology (Large Hospital)
Focus: Post-treatment continuity
Actions:
- Send chemotherapy follow-up check-ins
- Broadcast symptom-monitoring reminders
- Enable secure post-infusion messaging
Team Tasks:
- Nursing team manages broadcast workflows
- Clinical team monitors flagged symptom responses
Hospitalists / OB ER (Any Size)
Focus: Labor & Delivery surge communication
Actions:
- Enable auto-replies for common L&D triage questions
- Activate surge-based messaging during peak admission hours
Team Tasks:
- Shift leads configure auto-reply templates
- Monitor inbound volume during high census periods
What Success Looks Like by End of Week 6
- Secure messaging live across web/SMS
- Auto-replies handling repetitive inquiries
- Broadcast messages supporting pre-op and post-care
- Front-desk phone dependency reduced, easing operational overload
- Improved patient satisfaction while protecting margins under continued financial pressures
Weeks 7–8: Revenue Release Phase – RCM & Billing Optimization
Revenue Cycle & Billing Layer Activation
This phase activates digital payment collection, automated billing workflows, and tighter claim submission loops inside the unified platform to accelerate cash flow and reduce A/R lag.
Primary Goal
- Launch Text-to-Pay and secure digital payment links
- Enable stored payment methods (wallets) and AutoPay
- Tighten claim submission and follow-up workflows
- Reduce manual billing outreach
Expected Fast Wins
- 40–60% faster patient collections
- Significant reduction in aging A/R, improved OB-GYN billing velocity
- Increased point-of-service collections
- $200K+ revenue acceleration potential for a $2M practice
- Fewer billing-related phone calls, easing administrative operational overload
Specialty-Specific Activation
REI (Private – Medium)
Focus: High-cost fertility cycles and transparent payment plans
Actions:
- Train staff on infertility billing structures (bundled vs. cycle-based)
- Enable digital wallets for staged fertility payments
- Activate Text-to-Pay for monitoring visits and add-ons
Team Tasks:
- Billing team configures stored payment options
- Financial coordinators review installment workflows
- Monitor cycle-based payment adherence
Gynecologic Oncology (Academic – Large)
Focus: Ongoing treatment copays and infusion billing
Actions:
- Send automated copay text reminders post-chemotherapy
- Enable AutoPay for recurring infusion visits
- Tighten claim submission loops for high-cost drugs
Team Tasks:
- Teams educate patients on AutoPay enrollment
- Billing reviews infusion claim turnaround times
- Monitor patient balance reduction trends
FPMRS / Urogynecology (Subspecialty)
Focus: Surgical collections and payment plans
Actions:
- Launch digital pre-surgery payment plans
- Enable card-on-file for post-op balances
- Integrate RCM workflows with surgical scheduling
Team Tasks:
- Surgeons align financial policies with RCM
- Billing team sets up structured installment plans
- Track surgical deposit capture rate
MFM (Hospital – Large)
Focus: High-risk prenatal and diagnostic copays
Actions:
- Activate automated copay capture at scheduling
- Enable Text-to-Pay for ultrasounds and follow-ups
- Integrate eligibility verification with billing triggers
Team Tasks:
- Billing integrates payment workflows with hospital systems
- Monitor point-of-service collection rate
- Track claim submission-to-payment cycle time
What Success Looks Like by End of Week 8
- Text-to-Pay live and actively used
- Wallets & AutoPay reducing unpaid balances
- Claim submission loops tightened
- A/R aging decreasing
- Measurable cash acceleration within 30–60 days
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Week 9: Denial Killer – RCM Deep Dive
Revenue Cycle Deep Dive & Protection
This phase focuses on reducing denials, strengthening first-pass claim approvals, and implementing proactive safeguards to prevent revenue loss.
Primary Goal
- Enable real-time claim tracking
- Activate denial alert dashboards
- Implement automated correction workflows
- Strengthen prior authorization controls
Expected Fast Wins
- Increased first-pass claim approval rates
- Faster resubmissions on flagged claims
- Reduced compliance-related penalties
- Lower denial-related write-offs
- Improved clean claim ratio
Specialty-Specific Activation
Gynecologic Oncology (Private Practice)
Focus: High-cost drug and infusion authorization protection
Actions:
- Activate prior authorization tracking safeguards
- Flag missing documentation before claim submission
- Enable denial screening dashboards for chemotherapy claims
Team Tasks:
- Billers review flagged claims before submission
- Staff monitor auth expiration timelines
- Track denial trends weekly
FPMRS / Urogynecology (Medium Group)
Focus: Surgical coding and medical necessity denials
Actions:
- Implement surgery-specific denial alerts
- Flag documentation gaps before submission
- Strengthen modifier and CPT validation checks
Team Tasks:
- Coders customize claim validation rules
- Surgeons align documentation with billing requirements
- Monitor surgical denial percentage monthly
Hospitalists / OB ER (Locum Model)
Focus: Flow-based claim gaps and rapid turnover documentation
Actions:
- Create denial feedback loops tied to admission workflows
- Flag incomplete encounter documentation
- Track ER-to-admit claim submission timelines
Team Tasks:
- Leads monitor claim submission cadence
- Ensure documentation completeness before billing handoff
- Review denial patterns by shift or provider
What Success Looks Like by End of Week 9
- Real-time denial dashboard active
- Prior auth gaps caught before submission
- Clean claim rate trending upward
- Faster denial resolution turnaround
- Revenue leakage visibly reduced
What Success Looks Like by End of Week 9
- Real-time denial dashboard active
- Prior auth gaps caught before submission
- Clean claim rate trending upward
- Faster denial resolution turnaround
- Revenue leakage visibly reduced
Week 10: Ops Dashboard Domination – All Layers Integrated
Full-Layer Integration & Executive Visibility
This phase integrates scheduling, messaging, billing, documentation, and RCM into centralized dashboards with real-time KPIs and mobile access.
Primary Goal
- Activate automated task routing across departments
- Launch real-time KPI dashboards
- Enable mobile access for providers and leadership
- Ensure full interoperability with EHR/PMS systems
Expected Fast Wins
- 10–15% smoother operational flow
- Faster decision-making using live data
- Reduced administrative bottlenecks
- Clear visibility into performance trends
- Leadership-level control without manual reporting
Specialty-Specific Activation
MFM (Academic Center)
Focus: High-risk pregnancy oversight + research performance
Actions:
- Launch dashboards tracking high-risk case volumes
- Monitor authorization turnaround and visit access times
- Integrate research tracking metrics (trial enrollment, protocol visits)
Team Tasks:
- Department chiefs review risk dashboards weekly
- Research coordinators monitor enrollment KPIs
- Leadership flags delays in care pathways
REI (Subspecialty Practice)
Focus: Fertility cycle performance and provider efficiency
Actions:
- Activate mobile dashboards for cycle milestones
- Track retrieval-to-transfer timelines
- Monitor cancellation fill rates and revenue per cycle
Team Tasks:
- Physicians access dashboards during clinic shifts
- Coordinators review cycle adherence trends
- Admin tracks revenue-to-visit ratio
Menopause / Hormone Practice (Solo)
Focus: Simplicity and daily operational clarity
Actions:
- Enable simplified daily performance view
- Track appointments, collections, and no-show trends
- Monitor patient communication metrics
Team Tasks:
- Practice owner reviews dashboard daily
- Adjust scheduling or messaging based on trends
- Identify revenue or access gaps early
What Success Looks Like by End of Week 10
- All operational layers connected
- Real-time KPI visibility across departments
- Automated task routing reducing manual oversight
- Mobile access for on-the-go providers
- Leadership making data-backed decisions
Week 11: Loyalty Love Bomb – Patient Mgmt + Experience Polish
Patient Management & Experience Optimization
This phase fine-tunes the patient journey using mobile surveys, experience scoring (PXI), workflow refinements, and documentation improvements to boost satisfaction and referrals.
Primary Goal
- Launch mobile post-visit satisfaction surveys
- Track PXI (Patient Experience Index) metrics
- Close feedback loops quickly
- Refine documentation templates and workflows
- Turn satisfied patients into referral drivers
Expected Fast Wins
- 85%+ patient satisfaction scores
- Increased online reviews and ratings
- Higher referral rates
- Reduced complaint escalations
- Improved provider documentation clarity
Specialty-Specific Activation
Pediatric / Adolescent GYN (Hospital-Based)
Focus: Family-centered experience refinement
Actions:
- Deploy post-visit mobile surveys to guardians
- Identify friction in reminders or check-in workflows
- Adjust timing and tone of pediatric visit nudges
Team Tasks:
- Families complete quick mobile surveys
- Staff review satisfaction trends weekly
- Operations adjust reminder flows based on feedback
Family Planning (Group Practice)
Focus: Sensitive-care communication optimization
Actions:
- Activate structured feedback loops post-consult
- Monitor satisfaction around intake and consent workflows
- Refine documentation templates for clarity and compliance
Team Tasks:
- Physicians review feedback themes
- Teams update documentation templates accordingly
- Leadership monitors referral and review growth
What Success Looks Like by End of Week 11
- Mobile survey response rates trending upward
- Patient Experience Index consistently above 85%
- Feedback loops closed within defined timelines
- Documentation workflows refined for clarity
- Noticeable growth in reviews and word-of-mouth referrals
Week 12: Victory Lap Live – Full Stack Go-Live
Full-Stack Go-Live & Enterprise Sign-Off
This phase validates the entire transformation, from intake and scheduling to messaging, RCM, denial protection, dashboards, and identity workflows (e.g., Facecheck). It ensures operational stability before scale.
Primary Goal
- Conduct end-to-end workflow testing
- Validate interoperability across systems
- Complete leadership sign-offs
- Deliver refresher training for all teams
- Establish growth KPIs post-launch
Expected Fast Wins
- Fully stabilized workflows across departments
- Confidence in patient experience and revenue systems
- Reduced risk during high-volume days
- Clear accountability ownership
- Defined growth roadmap
Specialty-Specific Activation
Hospitalists / Locums (Any Size)
Focus: High-speed operational stress testing
Actions:
- Conduct rapid admission-to-discharge workflow drills
- Test mobile documentation and eligibility workflows
- Run high-volume surge drills for L&D and OB ER.
Team Tasks:
- Points of Contact (POCs) validate full-run workflows
- Shift leads confirm documentation-to-billing handoffs
- Confirm Facecheck / eligibility tools function under peak load
MFM & Oncology (Large / Academic Systems)
Focus: Cross-departmental integration approval
Actions:
- Validate clinical documentation, authorization, scheduling, and billing handoffs
- Confirm research, infusion, and high-risk workflows are synchronized
- Review dashboard accuracy and KPI alignment
Team Tasks:
- Department heads provide final operational approval
- Revenue leadership confirms denial and claim metrics
- Executive team sets post-launch growth targets
What Success Looks Like by End of Week 12
- End-to-end workflows tested and validated
- All departments formally signed off
- Mobile and interoperability layers confirmed stable
- Growth KPIs defined for next quarter
- Team trained and confident
Overcoming Tech Adoption Barriers in OB-GYN Practice Transformation
| Adoption Barrier | Common Concern in OB-GYN | CERTIFY Health Approach (12-Week Plan) | Impact / Outcome |
|---|---|---|---|
| Provider Resistance | Burned-out OB-GYNs dread extra screens amid clinic and L&D chaos. | Weeks 1–2 workflow demos showing 20–30% call reduction; mobile-first tools; embedded into existing workflows | Technology feels like relief, not added burden |
| EHR Integration Anxiety (Epic-heavy hospitals) | Fear of workflow disruption and duplicate data entry | Seamless interoperability with major EHR/PMS systems; real-time eligibility, scheduling, and billing sync | No duplicate entry, no workflow breakage |
| Cost Hesitation (Solo/Small Practices) | Concern about affordability and ROI | Revenue acceleration via Text-to-Pay, AutoPay, denial reduction; no heavy CapEx | $200K–$400K potential capital unlock in $2M practice; ROI in 60–90 days |
| Training Overload (Subspecialties) | No time for long onboarding sessions | Bite-sized, role-based training; phased weekly rollout; mobile-accessible learning | Gradual adoption without operational disruption |
| Compliance Sensitivity (Family Planning / FPMRS) | High regulatory scrutiny; consent complexity | HIPAA-secure workflows; exclusion-flag intake alerts (Week 4); digital consent capture | Stronger compliance controls with audit trails |
| Scalability for Rural / Locum Models | Staffing gaps and unpredictable L&D surges | ASAP waitlists auto-fill 60–80% of cancellations; mobile scheduling & documentation support | Greater operational resilience during peak volume |
Ready to Reclaim Revenue & Efficiency?
Don’t wait another quarter while denials rise and schedules leak revenue.
Connect with CERTIFY Health today to build your customized 12-week OB-GYN practice transformation plan and start turning operational friction into financial momentum.