Table of Contents
Introduction to Patient Education
Patient education is a structured, continuous process through which healthcare providers help patients understand their condition, their choices, and their role in managing health over time.
At its core, patient education answers three questions every patient carries but rarely asks out loud:
- What is happening to my body?
- What decisions do I need to make?
- What actions actually change outcomes?
In modern healthcare delivery, patient education includes:
- Clear explanation of diagnoses using plain language.
- Teaching self-management skills for chronic conditions.
- Aligning treatment plans with patient literacy, culture, and readiness.
- Reinforcement across touchpoints such as visits, portals, follow-ups, and care plans.
The goal to facilitate behavioral activation.
A cohort study of hospitalized heart failure patients found that low health literacy independently increased the risk of 30-day unplanned healthcare use (hospital readmission or ED visits) after discharge.
That statistic matters because it reframes from patient education as a clinical intervention.
From an operational standpoint, patient education sits at the intersection of:
- Clinical decision-making.
- Patient engagement strategies.
- Value-based care and quality metrics.
- Long-term cost containment.
Any healthcare system treating it as optional is already behind.
Why Patient Education Matters for Engagement and Outcomes
Engagement starts with comprehension.
Patients fail care plans because they are confused, overwhelmed, or misinformed. Education reduces friction between intent and action.
A clinical trial based on improving use and adherence of effective coronary heart disease prevention strategies found that patients receiving the intervention had self-reported adherence about 25 percentage points higher than usual care at 3-month follow-up.
That improvement cascades into measurable outcomes:
- Higher medication adherence.
- Better chronic disease control.
- Fewer preventable emergency visits.
- Improved patient-reported quality of life scores.
Strong patient education also changes the dynamic of care. Patients shift from passive recipients to informed participants. Questions become more precise. Decisions become shared. Trust improves.
From an engagement perspective, educated patients are more likely to:
- Use patient portals consistently.
- Complete follow-up instructions.
- Participate in preventive care.
- Stay within a health system over time.
This is why patient education is now central to population health management, patient engagement programs, and outcomes-driven healthcare models.
If engagement is the engine of modern care, patient education is the ignition.
Challenges and Barriers to Effective Patient Education
Patient education fails for predictable reasons. These are not patient shortcomings. They are system design failures. Research has documented the same barriers for decades, yet many organizations still treat them as unavoidable.
Limited Health Literacy and Cognitive Barriers
According to the National Assessment of Adult Literacy, only 12% of U.S. adults have proficient health literacy, meaning the majority struggle to understand routine medical information. This directly affects comprehension, adherence, and self-care.
Cognitive load compounds the problem. New diagnoses, stress, pain, and medication changes reduce retention even among highly educated patients.
Common failure points include:
- Overly technical language.
- Long explanations without prioritization.
- No confirmation of understanding.
Effective education systems simplify, sequence, and reinforce. Without that, instructions become noise.
Technology and Access Gaps
Digital education only works if patients can access it.
Federal research shows persistent gaps in broadband access, smartphone ownership, and digital literacy across age and income groups in the U.S. When education is delivered only through digital channels, vulnerable populations are excluded by default.
Key access challenges include:
- Limited internet connectivity.
- Shared or outdated devices.
- Low confidence using digital tools.
High-performing systems offer multiple education pathways, not a single digital gate.
Cultural, Language, and Socioeconomic Factors
Language barriers and cultural misalignment reduce engagement and trust, leading to worse outcomes. Socioeconomic pressures further complicate adherence when instructions conflict with daily realities.
Barriers often appear as:
- Mistrust of healthcare systems.
- Cultural beliefs about illness and treatment.
- Inability to follow plans due to cost or work constraints.
Education must acknowledge these realities to be effective.
Provider Training and Time Constraints
Clinicians are rarely trained to teach.
Medical education emphasizes diagnosis and treatment, not communication science. Combined with time pressure, this leads to rushed explanations and missed opportunities for understanding.
Clinicians who receive structured communication training deliver more effective patient education without extending visit length.
The takeaway is clear. The barrier is not time. It is training and system support.
Patient education challenges are well known. The organizations that succeed are the ones that design around them instead of blaming patients for predictable failures.
How Patient Portals and Personalized Education Drive Better Patient Engagement
Effectiveness of Patient Education via Patient Portals
Patient portals have moved from a convenience feature to a primary delivery channel for patient education. The evidence is no longer theoretical.
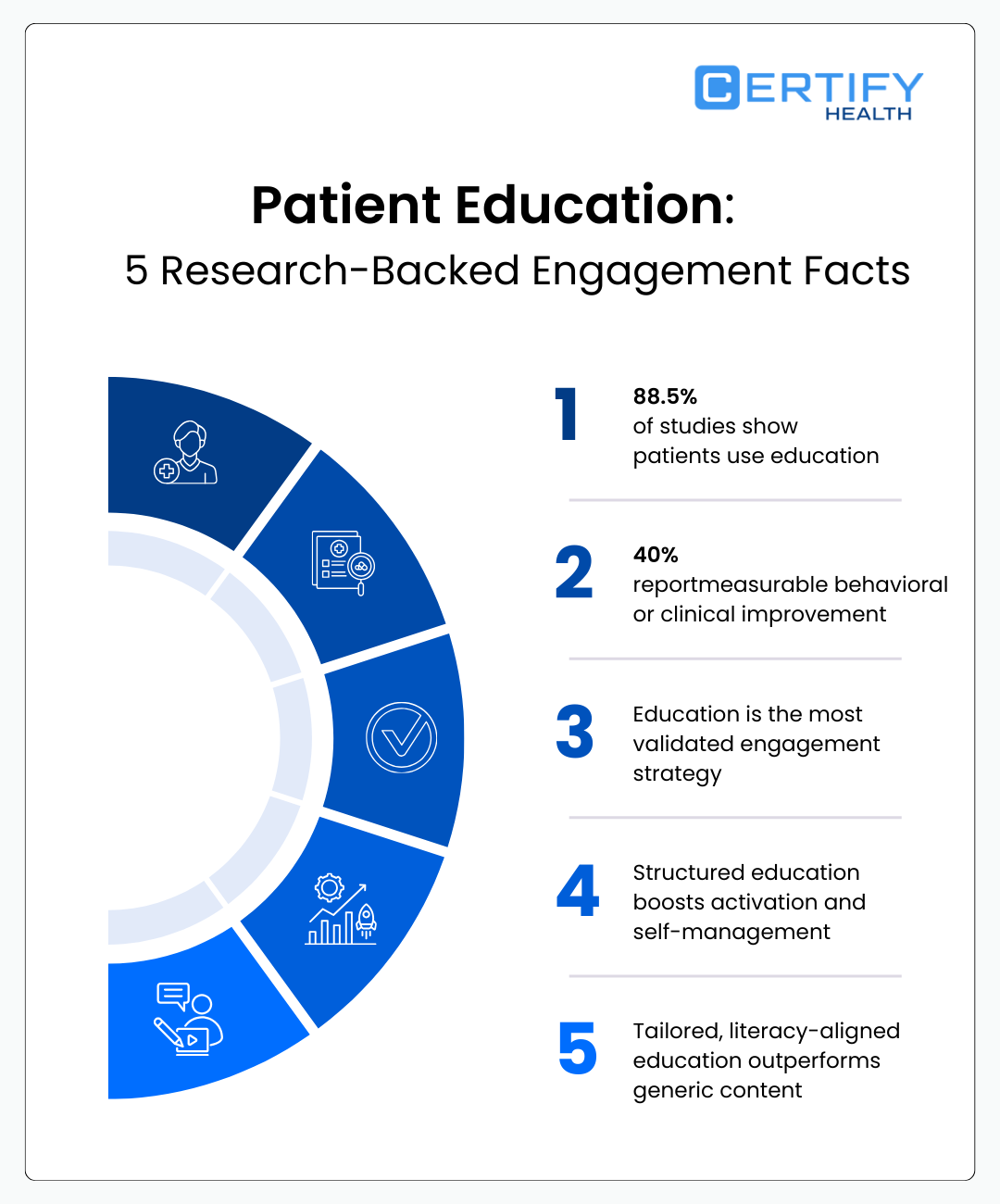
A systematic review evaluated patient education delivered through patient portals across clinical settings.
It found that 88.5% of the included studies reported active patient use of educational content delivered via portals, and 40% demonstrated statistically significant improvements in clinical or behavioral outcomes, including medication adherence, disease self-management, and follow-up compliance.
This matters for one simple reason. Portals remove the single biggest barrier to patient education: timing.
Education delivered during a clinical visit competes with anxiety, time pressure, and cognitive overload. Portal-based education meets patients:
- After the diagnosis has settled in.
- At the moment decisions are being made.
- Repeatedly, not once.
High-performing portals do not just host PDFs. They structure education around:
- Condition-specific pathways.
- Actionable next steps.
- Reinforcement through reminders and follow-ups.
From an engagement standpoint, portal education changes usage patterns. Patients are not logging in only to view lab results but are also returning to understand what those results mean and what to do next.
This is why patient education via portals correlates strongly with:
- Higher longitudinal engagement.
- Reduced care plan abandonment.
- Improved patient-reported confidence in self-care.
Healthcare organizations that underutilize portals for education are wasting one of the few channels patients already trust and repeatedly use.
Narrative Evidence for Tailored and Multi-Level Approaches
If patient education fails, it is rarely because the information is wrong. It fails because it is not designed for the person receiving it.
Narrative reviews and evidence syntheses from U.S. academic medical centers consistently show that tailored patient education outperforms generic education across literacy levels, ages, and disease categories.
Education is most effective when it is adapted to:
- Health literacy and numeracy.
- Language and cultural context.
- Disease severity and stage.
- Patient readiness and cognitive load.
One review found that multi-level education strategies, combining verbal instruction, written materials, and digital reinforcement, were associated with meaningful improvements in self-management behaviors, while single-format education showed limited durability over time.
The implication is clear. One-size-fits-all education is clinically inadequate.
High-impact patient education operates on multiple levels:
- Individual level: personalized explanations and goals.
- System level: consistent messaging across visits and platforms.
- Temporal level: reinforcement over weeks and months, not minutes.
Strong systems design education the way clinicians practice medicine. Context-aware, adaptive, and continuous.
Patient education is not about telling patients more. It is about telling them what matters, in a way they can act on, and doing it consistently.
Healthcare systems that invest in tailored, multi-level education do not just improve engagement metrics. They improve outcomes that regulators, payers, and patients all care about.
Core Principles of Effective Patient Education
1. Health Literacy–Centered Communication
- Align educational content with patient reading and comprehension levels.
- Use plain language, avoid medical jargon, and include visual aids when possible.
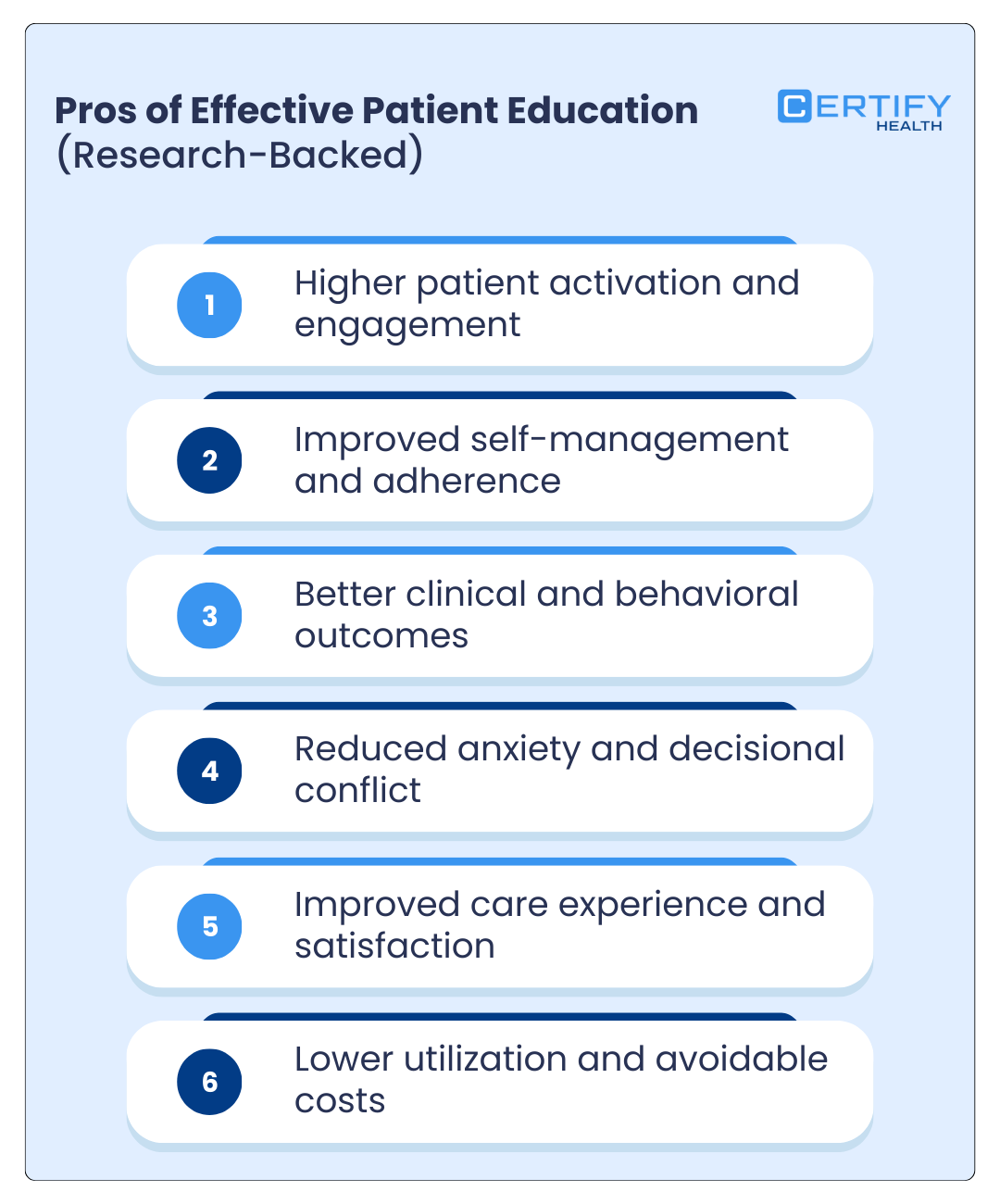
Studies show that patients with higher health literacy experience up to 30% fewer hospitalizations across chronic disease populations.
Tips for Implementation:
| Strategy | Why it Works | Example |
|---|---|---|
| Plain-language materials | Reduces confusion and improves recall | Use “high blood pressure” instead of “hypertension” |
| Visual aids | Supports patients with low literacy | Infographics of medication schedules |
| Layered content | Enables patients to explore at their own pace | Step-by-step guides with expandable sections |
2. Teach-Back and Comprehension Checks
- Ask patients to repeat instructions in their own words to confirm understanding.
- Recommended by major U.S. health authorities including CDC and AHRQ.
Teach-back interventions improve comprehension and medication adherence, with studies showing ~21–25% increase in treatment adherence in outpatient settings.
Implementation Examples:
- After explaining a new medication regimen, ask: “Can you show me how you would take this medication at home?”
- Use standardized checklists to document patient comprehension.
3. Shared Decision-Making Tools and Decision Aids
- Decision aids help patients weigh options, understand risks/benefits, and align care with personal values.
- Improves engagement and satisfaction, particularly for chronic disease management.
The systematic review of patient portal–based education mentioned earlier showed:
- 88.5% of studies reported active patient use of educational content
- 40% demonstrated statistically significant improvements in clinical or behavioral outcomes, including medication adherence, disease self-management, and follow-up compliance
Example Tools:
- Online interactive symptom checkers with tailored treatment options.
- Printable decision aids for procedures such as colonoscopy, diabetes care, or hypertension management.
- Integrated portal reminders prompting patients to review educational content before appointments.
Pro Tip:
Integrating health literacy–friendly materials, teach-back checks, and decision aids into patient education programs not only improves adherence and engagement but is backed by robust U.S. Federal research.
Proven Methods Healthcare Providers Use
1. In-Visit Education Techniques
Personalized Verbal Counseling
The most powerful patient education tool is still the clinician’s voice, when used deliberately. Personalized verbal counseling means adapting explanations to the patient’s condition, literacy level, and emotional state in real time.
A recent randomized trial that patients who received individualized verbal education during visits demonstrated a rough 19% higher adherence to treatment plans compared to those receiving standardized instructions alone.
Effective verbal education focuses on:
- One diagnosis at a time.
- One decision at a time.
- One clear action the patient can repeat back.
If the patient cannot explain it in their own words, the education failed.
Visual Aids, Print Materials, Multimedia
Humans remember images better than instructions. Multimodal education works because it reduces cognitive load.
A study conducted within U.S. primary care clinics showed that combining verbal counseling with visual aids and printed summaries led to a 35% improvement in information recall and significantly higher patient satisfaction scores.
High-value materials include:
- Simple diagrams of anatomy or disease progression.
- One-page summaries, not dense brochures.
- Short videos used during or immediately after the visit.
Education should clarify, not impress.
Patient-Centered Questioning and Dialogue
Open-ended questioning, such as “What concerns you most about this plan?”, consistently improves engagement.
Research shows patient-centered communication is associated with higher shared decision-making scores and better self-management behaviors across U.S. outpatient populations.
When patients feel heard, they engage.
2. Digital & Remote Education Strategies
Patient Portal Content and Reminders
Patient portals are now a primary education channel. National reports show high perceived usefulness and consistent engagement with portal-delivered educational content, especially when paired with reminders.
Effective portal education includes:
- Condition-specific explanations tied to test results.
- Clear next steps.
- Timed reminders aligned with care plans.
Static content underperforms. Contextual content works.
Mobile Apps and mHealth Tools
Smartphone-based education improves learning because it travels with the patient.
Patients using educational mobile apps show significantly higher comprehension and medication adherence compared to control groups receiving usual care.
Short lessons, reminders, and progress tracking matter more than feature density.
Emerging Technologies such as Mixed Reality
For complex procedures, immersive education shows promise. Mixed reality tools used in preoperative education have led to improved patient understanding and reduced anxiety before surgery.
This is about clarity when stakes are high.
3. Reinforcement and Follow-Up
Automated Summaries and Follow-Up Messaging
Patients forget most of what they hear within hours. Automated visit summaries and follow-up messages reinforce learning at the right time. Post-visit reinforcement is linked to better retention and follow-through on care instructions.
Coaching and Tele-support
Patient Education Across the Care Continuum
Pre-Visit Preparation & Expectations
- Patients receive education before the appointment
- Sets the agenda for the visit
- Patients arrive informed and prepared
- Improves visit efficiency and satisfaction
In-Visit Shared Understanding
- Education becomes action during the encounter
- Clinician and patient align on goals
- Questions are clarified in real time
- Shared understanding turns plans into commitments
Post-Visit Reinforcement & Retention
- Learning continues after checkout
- Follow-up materials reinforce key messages
- Supports recall and adherence
- Determines real-world outcomes
Outcome: Effective Patient Education
Education succeeds when it is:
- Continuous — before, during, and after care
- Personalized — tailored to the individual
- Human-centered — designed for real behavior, not ideal compliance
Which Healthcare Specialties Benefit Most From Patient Education?
Patient education does not deliver equal returns across all specialties. It delivers outsized impact where care depends on behavior outside the clinic. The evidence is clear across U.S. healthcare settings.
High-Impact Specialties and Why Education Works
| Specialty | Where Education Has the Most Impact | Evidence-Based Outcome Metric |
|---|---|---|
| Primary and General Medicine | Chronic disease self-management and preventive care | Structured education reduces avoidable hospitalizations in chronic disease populations by up to 30% |
| Cardiology | Medication adherence and lifestyle modification | Patient education improves cardiovascular medication adherence by 17 to 23% |
| Mental and Behavioral Health | Treatment engagement and coping strategies | U.S. trials show psychoeducation increases therapy adherence by approximately 20% |
| Orthopedics and Rehabilitation | Postoperative recovery and exercise compliance | Education-driven programs improve exercise adherence by over 25% |
| Pediatrics and Women’s Health | Caregiver understanding and lifecycle care | Studies link caregiver education to higher preventive visit adherence and vaccination uptake |
| Urgent and Transitional Care | Discharge comprehension and self-care | Improved discharge education reduces 30-day readmissions by around 15% |
Primary and General Medicine
Primary care carries the heaviest education burden. Chronic conditions like diabetes, hypertension, and asthma are managed almost entirely outside the exam room. Patient education directly influences daily decisions.
Without education, care plans collapse. With it, patients become reliable partners in prevention and long-term management.
Cardiology
Cardiology outcomes hinge on adherence. Medications only work if taken correctly. Lifestyle changes only matter if sustained.
Cardiovascular studies consistently show education improves medication persistence, diet compliance, and symptom monitoring. In heart disease, education is risk reduction.
Mental and Behavioral Health
In behavioral health, education is engagement. Explaining the nature of illness, expected timelines, and coping strategies reduces stigma and drop-off.
Psychoeducation programs in U.S. outpatient settings demonstrate measurable gains in therapy attendance and treatment continuity. Patients who understand their condition are more likely to stay in care.
Orthopedics and Rehabilitation
Recovery fails quietly. Patients stop exercises at home long before clinicians notice.
Education that explains why movements matter, what pain is normal, and how recovery progresses leads to better functional outcomes. Evidence from U.S. rehab programs shows education-driven adherence improves recovery timelines.
Pediatrics and Women’s Health
Education often targets caregivers, not just patients. From prenatal care to adolescent health, understanding timelines, warning signs, and preventive milestones matters.
CDC-backed research consistently links caregiver education to improved preventive care utilization and early intervention.
Urgent and Transitional Care
Discharge is the most dangerous moment in healthcare. Confusion leads to readmissions.
Structured discharge education significantly improves self-care behaviors and reduces unnecessary return visits.
Across specialties, the pattern is consistent. Where behavior drives outcomes, patient education delivers the greatest clinical return.
How CERTIFY Health’s Patient Education Benefits Healthcare Providers
Patient education fails when systems rely on memory, paper, or one-time explanations. It works when education is embedded into workflows, reinforced over time, and accessible when patients actually need it.
This is where CERTIFY Health aligns closely with what research shows works in real clinical settings.
→ Automated Care Instructions and Follow-Up Messaging
Education that is not reinforced is forgotten.
Patients forget up to 80% of medical instructions within hours of a visit, especially when managing new diagnoses or medications. Reinforcement is not optional. It is evidence-based.
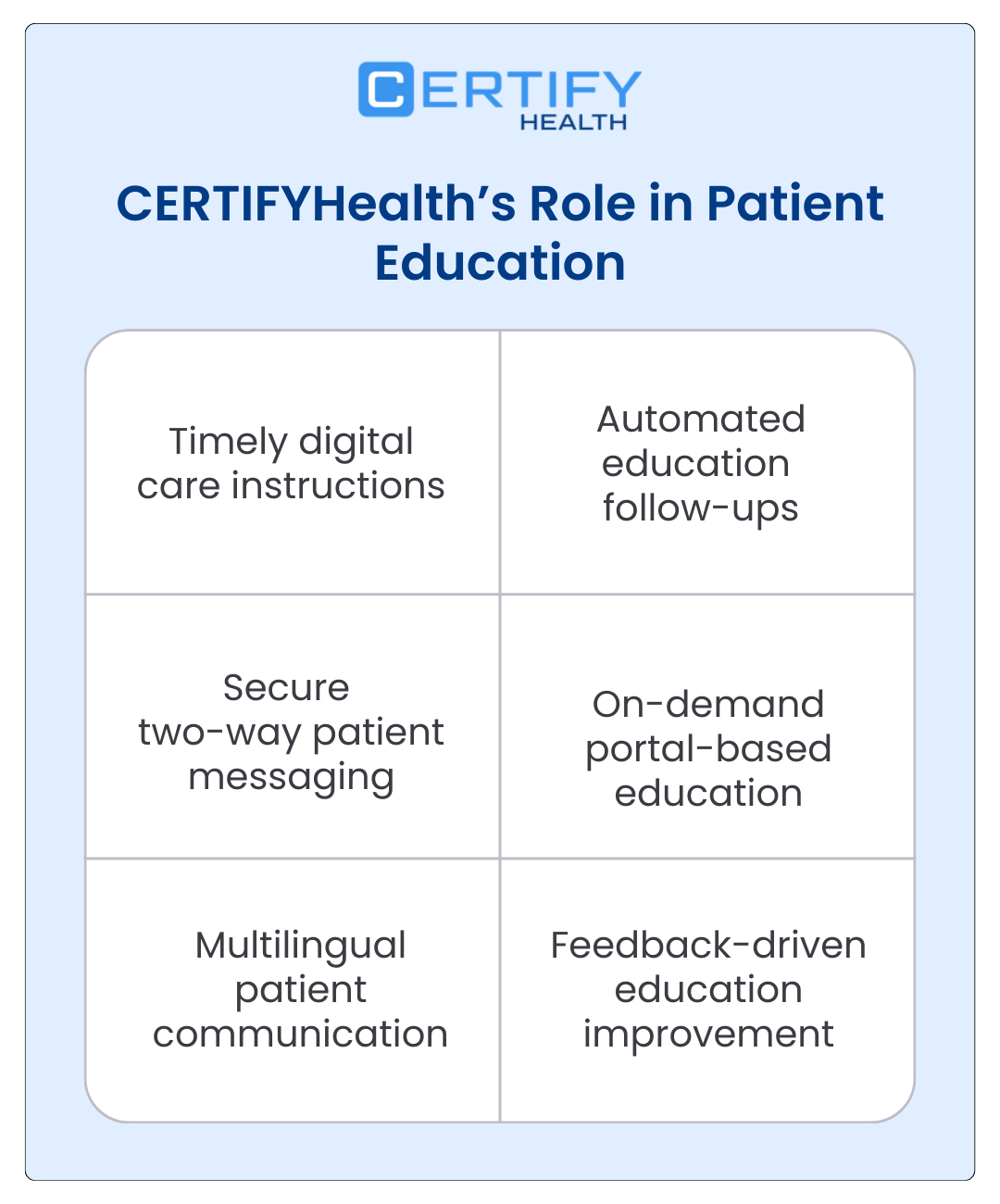
CERTIFY Health supports automated care instructions and follow-up messaging that:
- Reiterate next steps after visits.
- Reinforce medication and self-care instructions.
- Deliver reminders at clinically relevant intervals.
This directly supports retention, adherence, and continuity, which are consistently linked to better outcomes.
Secure Two-Way Patient Communication
Confusion is the enemy of engagement.
NIH-supported communication studies show that patients with access to follow-up clarification experience significantly fewer misunderstandings and higher satisfaction with care plans compared to one-way instruction models.
CERTIFY Health enables secure two-way communication so patients can:
- Ask questions after the visit.
- Clarify instructions before problems escalate.
- Resolve uncertainty without unnecessary visits.
Strong education systems allow dialogue, not silence.
On-Demand Patient Portal Access to Educational Content
Timing matters more than volume.
Patients who access educational content through portals demonstrate higher self-management confidence and engagement than those relying on in-visit education alone.
CERTIFY Health makes education available on demand through the patient portal, aligned to:
- Diagnoses.
- Care plans.
- Follow-up actions.
This mirrors research-backed models where patients learn best after the visit, not during cognitive overload.
Multilingual Support and Accessibility
Education that cannot be understood is not education.
Limited health literacy worsens outcomes and lowers engagement. Addressing language and accessibility gaps is not a compliance feature. It is a clinical necessity.
CERTIFY Health supports multilingual and accessible communication to:
- Reduce comprehension barriers.
- Improve equity in engagement.
- Reach patients across literacy levels.
Systems that ignore this gap quietly lose patients. Book a demo to learn more.
Feedback Collection to Tailor Education
Generic education underperforms. Tailored education works.
Feedback-driven personalization improves engagement and self-management behaviors across chronic and preventive care populations.
CERTIFY Health incorporates surveys and feedback loops to:
- Understand what patients did or did not understand.
- Adapt future education.
- Continuously refine messaging.
This closes the loop between education delivery and real-world impact.
The strongest patient education systems are not louder. They are smarter, continuous, and designed around how patients actually learn. CERTIFY Health reflects that evidence-driven reality.
How to Measure Patient Engagement and Education Success
Healthcare systems that take education seriously track whether patients understood, engaged, and acted. The metrics below are not vanity indicators. They are behavioral signals tied directly to outcomes.
Knowledge Retention and Teach-Back Performance
Understanding is the first gate.
Teach-back, where patients explain instructions in their own words, is one of the most validated education measures in U.S. care settings.
In a U.S. randomized controlled study of emergency department discharge instructions, nearly 90% of patients in the teach-back group had complete comprehension of follow-up instructions compared with about 50% in the standard instruction group, translating to roughly a 40 percentage point reduction in comprehension errors for key post-care guidance when teach-back was used.
High-performing organizations measure:
- Teach-back success rates.
- Common misunderstanding patterns.
- Topics requiring repeated clarification.
If patients cannot teach it back, they will not carry it out.
Portal Usage and Digital Engagement
Engagement leaves a digital trail.
Many observational studies using electronic health record data show that patients who actively engage with portals, defined as repeated logins and content views, demonstrate higher self-management confidence and follow-through compared to non-users.
Useful engagement metrics include:
- Educational content views per patient.
- Return visits to condition-specific resources.
- Completion of post-visit tasks.
Portal usage is not about clicks. It is about whether patients are returning to understand and act.
Adherence and Behavioral Change
Education-driven interventions are associated with measurable improvements in medication adherence, often in the range of 15 to 25% depending on condition and delivery method.
Behavioral metrics that matter:
- Medication refill consistency.
- Completion of recommended follow-ups.
- Self-reported lifestyle changes tied to care plans.
This is where education becomes a clinical lever.
Satisfaction and Experience Outcomes
Experience is a proxy for trust.
Patients who report clear explanations and understanding of care plans score significantly higher on satisfaction measures and are more likely to remain within the same health system.
Key indicators include:
- “Understood instructions” survey responses.
- Confidence in managing health after visits.
- Likelihood to recommend the provider or practice.
Satisfied patients are not just happier. They are more engaged, more adherent, and more likely to achieve better outcomes.
Patient education success is visible when understanding improves, engagement deepens, behavior changes, and trust grows.
Anything less is noise.
Frequently Asked Questions (FAQ): Patient Education
Does patient education improve health outcomes?
Yes. When it is done correctly, patient education produces measurable clinical impact.
Structured patient education is associated with significant improvements in medication adherence, self-management behaviors, and reduced avoidable hospitalizations, particularly in chronic disease populations.
What types of education materials are most effective?
The most effective materials are clear, multimodal, and actionable.
Combining verbal explanation with written or visual reinforcement improves recall and satisfaction compared to single-format education. Materials that work best share common traits:
- Plain language at a sixth-grade reading level or lower.
- Visual aids that explain processes, not just labels.
- Short summaries that emphasize what to do next.
Education should prioritize clarity over completeness.
How do I implement teach-back in practice?
Teach-back is simple and efficient when embedded into workflow.
AHRQ guidance recommends asking patients to explain instructions in their own words using non-judgmental prompts such as, “I want to be sure I explained this well. Can you walk me through what you will do when you get home?”
U.S. studies show teach-back improves comprehension without increasing visit time when used selectively for high-risk instructions.
Teach-back is not a test. It is a safety check.
What digital tools enhance patient education?
Digital tools work when they align with patient behavior.
Patient portals, automated follow-up messages, and mobile education tools improve engagement and self-management when content is contextual and reinforced.
High-impact tools include:
- Patient portals that link education to diagnoses and test results.
- Automated summaries delivered after visits.
- Secure messaging for clarification.
Technology does not replace education. It extends it beyond the visit.
The common thread across all effective patient education strategies is respect for how patients learn, forget, and act in the real world.
Conclusion and Evidence-Backed Best Practices
Patient education is no longer a soft skill or an optional add-on. The evidence from U.S. research is consistent and difficult to ignore. When patients understand their condition, their choices, and their role in care, outcomes improve. When they do not, even the best clinical decisions fail outside the exam room.
Core Takeaways
The strongest conclusions from the evidence are clear:
- Patient education is a clinical intervention, not a communication courtesy.
- Multimodal, reinforced education outperforms one-time explanations.
- Teach-back is one of the most reliable indicators of comprehension.
- Digital tools extend education, but do not replace human dialogue.
- Tailored education improves engagement, adherence, and trust.
AHRQ and NIH-supported studies repeatedly show that education linked to behavior change delivers measurable improvements in adherence, self-management, and preventable utilization.
Practical Steps for Clinics
Clinics that want results should focus on execution, not volume.
Evidence-backed actions include:
- Standardize teach-back for high-risk instructions.
- Pair in-visit education with post-visit summaries and reminders.
- Use patient portals to deliver condition-specific education.
- Offer materials in multiple languages and accessible formats.
- Measure education success through comprehension, engagement, and behavior, not distribution counts.
The most effective systems treat education as a continuous process across the care journey.
Direction for Future Research and Technology
Emerging research in the U.S. points toward:
- Adaptive education systems that adjust content based on patient feedback.
- Greater integration of education into clinical workflows and EHRs.
- Use of immersive technologies for complex decision-making.
- More rigorous measurement linking education directly to outcomes and equity.
Technology will continue to evolve, but the principle remains unchanged. Patients act on what they understand.
Healthcare organizations that align patient education with evidence, workflow, and patient reality will not only improve engagement. They will improve care itself.