Submit Claims Faster. Catch Rejections Before They Cost You.
Healthcare billing shouldn’t depend on manual data entry, late submissions, or surprise denials. CERTIFY Health streamlines the billing and claims process with claim submission automation and real-time rejection flags—so practices improve clean claim rates, shorten reimbursement cycles, and reduce denials.

Clean Claims Drive Cash Flow
In healthcare, billing delays and denied claims directly hit your revenue. Every missed submission or payer rejection slows reimbursements and increases bad debt. Practice administrators and billing managers often ask:
“How do we automate claim submission so staff aren’t re-keying data?”
“How do we spot claim rejections the moment they happen?”
“How do we stay compliant with payer rules and cut down on denials?”
Submit Clean Claims the First Time
Take the manual work out of billing with automation that adapts to payer requirements.
- Auto-generate claims from clinical and encounter data.
- Apply payer-specific rules to prevent common errors.
- Submit in batches or individually to fit your workflow.
- Increase first-pass acceptance rates and reduce days in A/R.
Outcome:
predictable reimbursements, less staff burden, stronger revenue cycle.
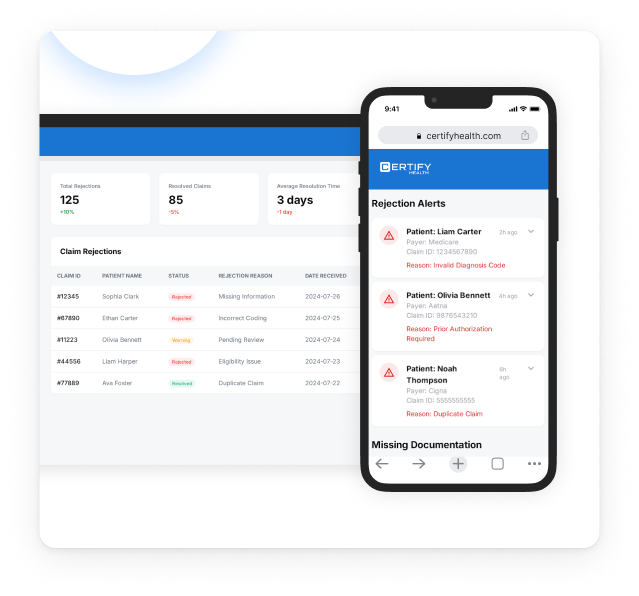
Spot and Fix Errors Before They Stall Revenue
Rejected claims shouldn’t be a surprise weeks later. CERTIFY Health flags them instantly so staff can act.
- Real-time alerts for payer rejections and missing documentation.
- Configurable workflows to escalate urgent issues.
- Built-in correction and resubmission tools.
- Rejection trend reporting for smarter prevention.
Outcome:
fewer denials written off, faster resubmissions, and more consistent revenue.
Why CERTIFY Health
for Patient Charts?
Unified platform
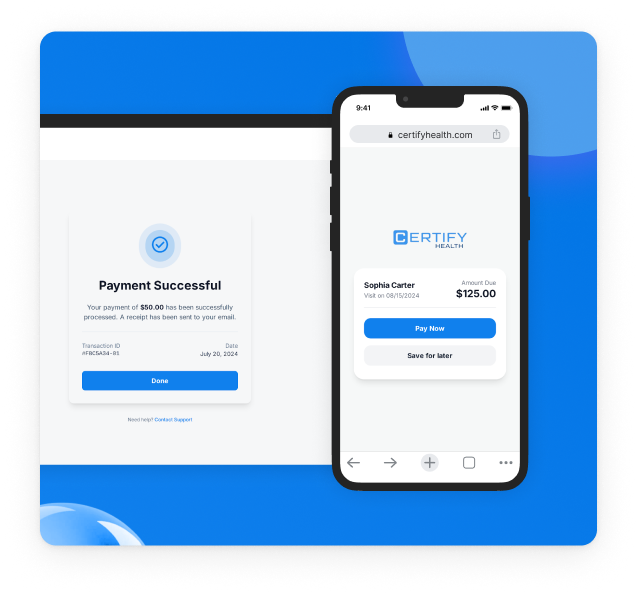
submissions, rejections, payments, and reporting in one system.
Provider-first design
built around the workflows of busy billing teams.
Compliance-ready
HIPAA, HITRUST r2, SOC 2, PCI DSS, and GDPR.
Scalable
from small clinics to multi-site enterprises.
Interoperable
works with major EHRs, clearinghouses, and payer systems.







