Collect Upfront. Reduce Denials. Improve Patient Trust.


Why It Matters
Patients are taking on more financial responsibility than ever, but without transparent tools, front desks struggle and practices lose revenue. Denials rise when eligibility isn’t confirmed. Balances balloon when co-pays aren’t collected upfront. Confusion frustrates staff and erodes patient satisfaction.
What CERTIFY Health’s Patient Revenue Platform Delivers

Real-Time Eligibility Checks
Verify coverage instantly—no manual calls or delayed portals. Patients and staff see accurate eligibility, benefits, and cost responsibilities at the point of intake.

Automated Payment Reminders
Send HIPAA-compliant SMS/email nudges for co-pays, balances, and upcoming bills. Patients stay informed, and your staff doesn’t waste hours chasing payments.
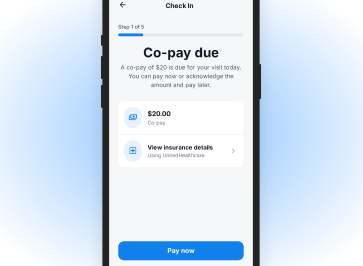
Co-Pay Prompts at Check-In
Collect what’s due before the visit begins. Integrated prompts at mobile, kiosk, and staff-assisted check-in ensure transparency, speed, and fewer outstanding balances.
Why Practices Choose CERTIFY Health’s Patient Revenue Tools
Reduced Claim Denials
Coverage verified upfront, preventing downstream rejections.
Faster Collections
Payments prompted and settled before services are rendered.
Lower Admin Burden
Automation removes manual tracking and follow-ups.
Better Patient Experience
Clear, proactive communication builds trust and avoids billing surprises.
Secure, Compliant, and Connected
Every transaction is protected with HIPAA, HITRUST r2, SOC 2, and PCI DSS compliance. Eligibility and payment workflows connect seamlessly to Epic, Cerner, MEDITECH, NextGen, athenahealth, and more—without disrupting your current PMS.

Ready to Protect Every Dollar Your Practice Earns?
Patient-side revenue capture is the first step toward financial stability. CERTIFY Health’s patient revenue tools makes it simple, automated, and patient-friendly.
FAQs
How does CERTIFY Health’s patient revenue platform help prevent patient billing surprises?
CERTIFY Health ensures patients always know what they owe before their visit begins. With real-time eligibility verification and transparent co-pay prompts during check-in, your team can clearly communicate costs upfront, no post-visit confusion or unexpected statements.
What makes CERTIFY Health’s patient revenue tools different from a typical payment collection tool?
Unlike basic payment processors, CERTIFY Health’s patient revenue platform connects the entire patient revenue journey from eligibility and co-pay collection to automated reminders and reconciliation.
It’s not just about collecting payments; it’s about creating transparency, efficiency, and trust between patients and providers.
Is the system secure for handling patient payment data?
Absolutely. CERTIFY Health’s patient revenue tools meets the highest standards of security and compliance (HIPAA, HITRUST r2, SOC 2, and PCI DSS). Every patient transaction, reminder, and eligibility check is fully encrypted and auditable.
How quickly can my practice start seeing results after implementation?
Many practices begin reducing claim denials and improving point-of-service collections within the first 30–60 days. Because workflows are automated and staff training is minimal, value realization is fast and measurable.







