Table of Contents
Introduction
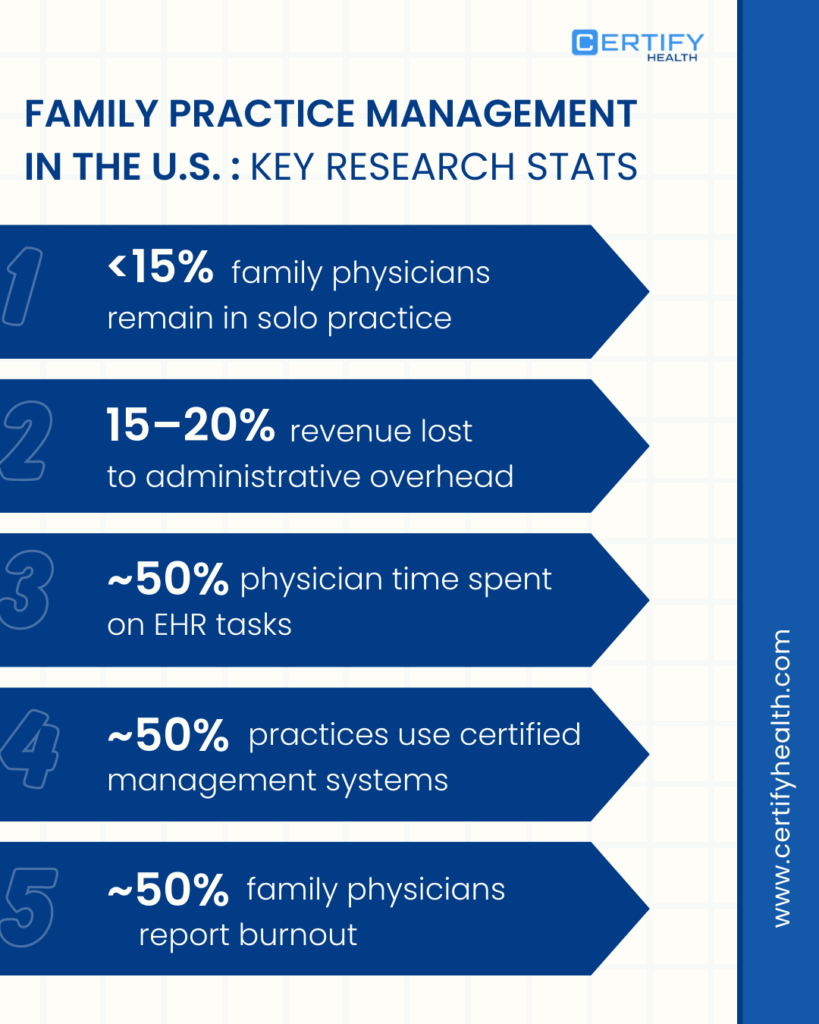
Family practice management has transitioned from an administrative necessity to a rigorous exercise in operational engineering.
As independent clinics and health systems grapple with unprecedented margin compression, the delta between a thriving practice and an insolvent one lies in the technical execution of workflow management, EHR optimization, and the shift toward value-based care (VBC).
The following guide provides a deep-dive, technical analysis of primary care operations designed for clinic owners, medical directors, and healthcare executives aiming for management excellence.
What Is Family Practice Management?
Family practice management is the systematic orchestration of clinical, financial, and administrative resources to deliver comprehensive, longitudinal care.
Unlike the narrow scope of specialty practices, family medicine requires a “whole-person” infrastructure. This involves managing pediatric, obstetric, adult, and geriatric populations within a single clinical operations framework.
In 2025, the U.S. Census Bureau and the Bureau of Labor Statistics (BLS) identified that healthcare management roles are projected to grow 28% through 2032, significantly faster than the average for all occupations, driven by the complexity of primary care coordination.
Family Practice vs. Specialty Practice Management
The management of a family practice is characterized by high-volume, low-acuity interactions that demand extreme efficiency.
| Feature | Family Practice Management | Specialty Practice (e.g., Surgery) |
|---|---|---|
| Patient Volume | High-frequency, recurring visits | Lower-frequency, episodic |
| Workflow Focus | Preventive care & chronic disease | Diagnostic & procedural efficiency |
| Revenue Model | Shift from FFS to Value-Based Care | Predominantly Fee-for-Service (FFS) |
| Data Requirements | Longitudinal & population health | Incident-specific & post-op |
Why Management Excellence Is Critical for Sustainability
Management excellence is an absolute necessity. With reimbursement pressure increasing, practices must leverage Health IT infrastructure to automate what was once manual.
Without a technical approach to operating margins, the overhead of traditional primary care will exceed revenue by late 2026 for most mid-sized clinics.
Core Components of Effective Family Practice Management
1. Clinical Operations and Workflow Management
According to MGMA, primary care practices with stronger operating margins employ non-physician providers at 41% or higher of physician staffing levels, versus 20% or lower in underperforming clinics, representing about 2X difference in team-based staffing intensity tied to financial performance.
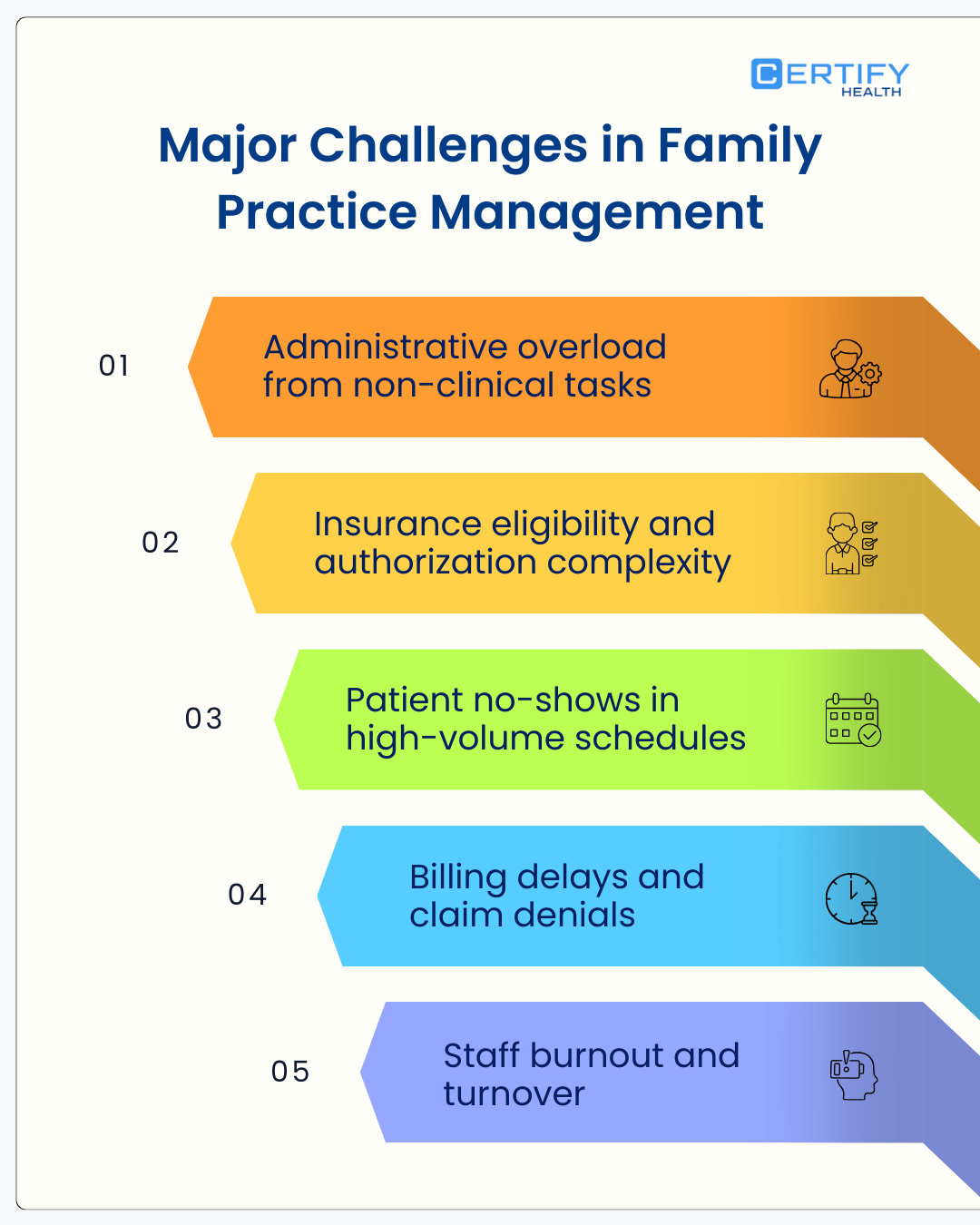
- Appointment Scheduling and Patient Flow: A broken appointment scheduling system is the primary driver of patient leakage.
Use “wave scheduling” or “modified wave scheduling” to ensure the provider is never waiting for a patient, and vice versa.
- Staffing Models: The 2026 trend is toward team-based care.
This includes “top-of-license” nursing where MAs handle all intake, immunization registries, and preventive care screenings, leaving only complex decision-making to the physician.
- Reducing Administrative Burden: The “pajama time” phenomenon (physicians charting late at night) is a management failure.
Implementing AI ambient scribes can reduce documentation time by up to 50%.
2. Financial and Revenue Cycle Management (RCM)
The Centers for Medicare & Medicaid Services (CMS) reported that for the 2025-2026 cycle, the Medicare Physician Fee Schedule (MPFS) conversion factor decreased by about 2.8%, forcing practices to find efficiency in claims accuracy to survive.
- Claims Accuracy: To maintain operating margins, a practice must achieve a 98% first-pass clean claim rate.
This requires “front-end” RCM: verifying insurance eligibility through a digital front door before the patient even arrives.
- Controlling Overhead: Overhead in family medicine typically hovers between 60% and 70%. Management excellence involves rigorous vendor management and the use of Group Purchasing Organizations (GPOs).
3. Technology and Health IT Infrastructure
- EHR Optimization: Most EHRs are “out-of-the-box” nightmares. Optimization involves creating specialty-specific templates and macros that automate continuity of care documentation.
- Interoperability: Your system must talk to local labs, imaging centers, and hospitals via HL7 or FHIR standards to prevent duplicate testing.
Patient Experience and Engagement in Family Medicine
Research shows that primary care practices with strong patient engagement and care coordination (such as PCMH models) are associated with a 5–8% reduction in emergency department visits among patients with chronic disease, demonstrating how proactive engagement strategies can lower acute care utilization
The Strategy of Patient Education
In a family practice, the patient is the most underutilized member of the care team.
Patient education is a management strategy that uses digital portals to deliver targeted content based on the patient’s diagnosis code.
Measuring Patient Satisfaction vs. Experience
- Satisfaction: A retrospective look at how the patient felt.
- Experience: A technical audit of the touchpoints: Was the appointment scheduling easy? Was the patient flow through the office logical?
- Tools: Use automated NPS (Net Promoter Score) triggers immediately following a visit.
Care Delivery Models: Transitioning to Value-Based Care
The Health Care Payment Learning & Action Network (LAN) reports that 45% of healthcare payments are now tied to some form of value-based care or alternative payment model as of late 2025.
Fee-For-Service (FFS) vs. Value-Based Care (VBC)
The traditional FFS model rewards volume, which leads to provider burnout. VBC rewards quality and preventive care measures.
- FFS: You get paid for the 15-minute visit.
- VBC: You get paid a PMPM (Per Member Per Month) fee to keep the patient healthy.
Patient-Centered Medical Home (PCMH)
The Patient-Centered Medical Home model is the operational gold standard. It requires:
- Care Coordination: Tracking patients through transitions of care (hospital to home).
- Access: Providing 24/7 access to clinical advice, often through telehealth.
Managing Chronic Disease and Population Health
The CDC’s National Center for Health Statistics notes that about 70% of U.S. adults have at least one chronic condition, making population health management the primary revenue driver for primary care.
Data-Driven Risk Stratification
Management involves using analytics to identify the “Rising Risk” patients. These patients are those who are not yet sick but whose data (rising A1c, missed appointments) suggests an impending crisis.
Technical Workflow: Risk Management
- Capture: Aggregate EHR, claims, and social determinants of health (SDOH) data.
- Analyze: Apply AI models to predict high-utilization events.
- Intervene: Assign a care coordinator for immediate outreach.
Operational Challenges: Burnout and Workforce Shortages
Operational strain has become one of the most underestimated barriers to effective patient follow-up management.
Clinics are being asked to do more follow-up, coordination, and documentation with fewer clinical resources. This gap is widening.
A 2025 study by the Association of American Medical Colleges (AAMC) projects a shortage of up to 40,000 primary care physicians by 2036, emphasizing the need for role optimization of mid-level providers.
This shortage makes one reality unavoidable: follow-up management cannot be physician-centric. Clinics must redesign workflows to better leverage mid-level providers and support staff while protecting physician time for high-value clinical decisions.
Addressing Provider Burnout Through Workflow Design
Provider burnout is rarely caused by patient care itself. More often than not, it is the result of administrative friction: excessive inbox messages, redundant documentation, and poorly defined task ownership.
Evidence-backed operational strategies include:
- Standardizing the Medical Assistant–to–Provider Ratio
Consistent MA-to-provider ratios reduce variability in workload distribution and prevent follow-up tasks from defaulting to physicians.
Clinics with clearly defined support staffing models see improved throughput and lower cognitive load on providers.
- Implementing Structured Inbox Management Protocols
A best-practice model routes approximately 80% of patient portal messages to trained nurses or care coordinators for triage, education, and resolution before escalation.
Physicians engage only when clinical decision-making is required, thereby preserving focus and reducing burnout risk.
Change Management in Technology Adoption
Even the best follow-up technology fails without structured adoption.
Clinics often underestimate the operational disruption caused by new Health IT tools, leading to partial usage, shadow workflows, and staff frustration.
A proven approach is the “Train-the-Trainer” change management model:
- Designate one clinical champion (e.g., physician or NP) to ensure workflows align with care delivery
- Designate one administrative champion to oversee scheduling, documentation, and staff adoption
- Empower both champions to lead training, collect feedback, and refine workflows during rollout.
This model accelerates adoption, builds internal accountability, and reduces resistance by anchoring change within trusted peer leadership rather than top-down mandates.
Without addressing burnout, staffing shortages, and adoption friction, follow-up programs fail at scale. Sustainable patient follow-up depends as much on operational architecture as on technology or intent.
Best Practices for Performance Improvement
To improve operating margins, practices must move from reactive to proactive management.
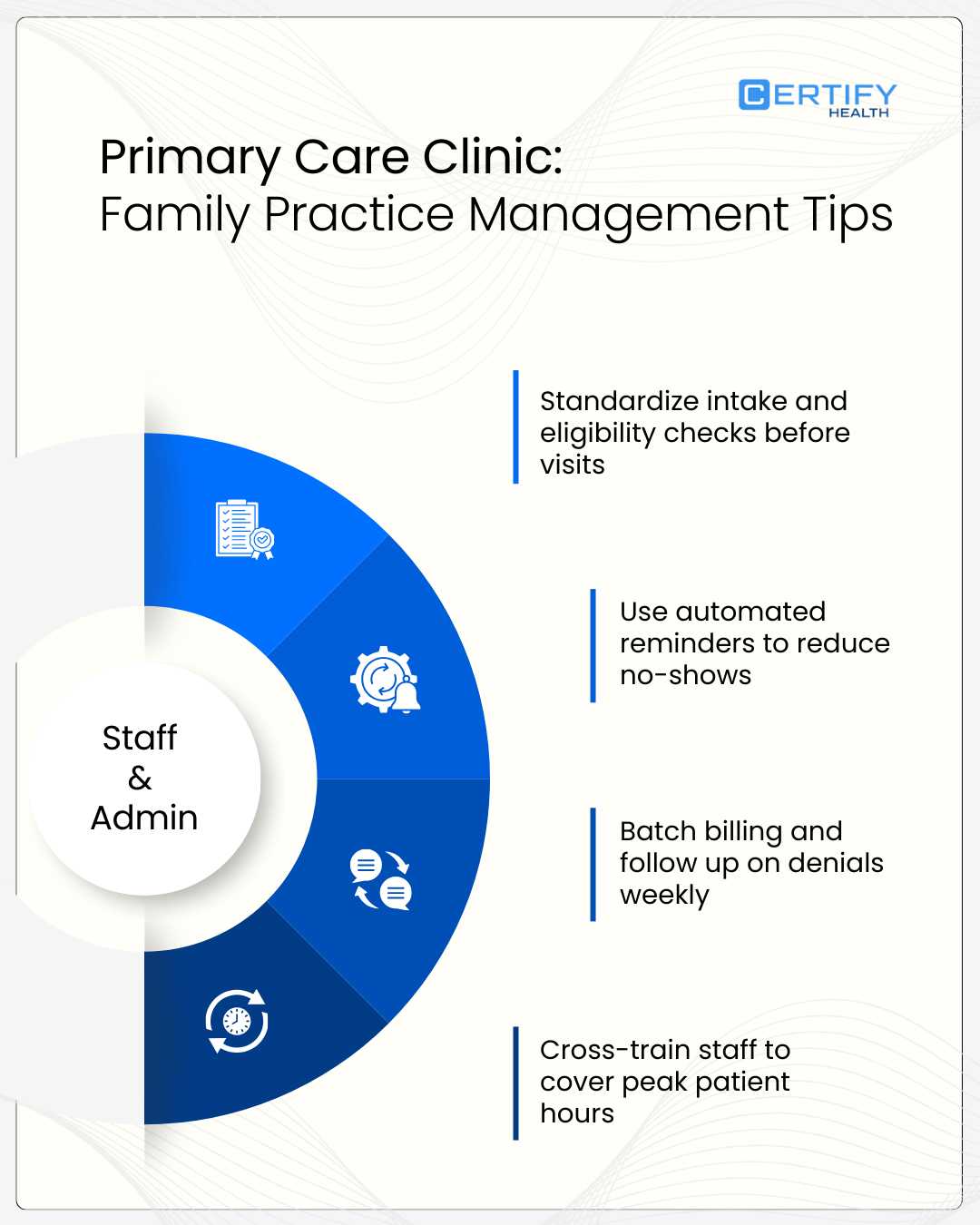
Standardizing Clinical and Administrative Workflows
- The Rooming Process: Use a 5-minute standard for vitals and intake.
- The Discharge Process: Ensure every patient leaves with a printed or digital “After Visit Summary” (AVS) and their next appointment scheduled.
Leveraging Automation
- Automated Recall: Use SMS bots to fill gaps in the schedule by targeting patients due for preventive care.
- Self-Service Intake: Allow patients to scan their IDs and pay co-pays via a kiosk or mobile app.
Key Metrics for Family Practice Management Success
| Metric Category | Key Performance Indicator (KPI) | Benchmark |
|---|---|---|
| Utilization | Third Next Available Appointment | < 48 Hours |
| Financial | Net Collection Ratio | > 96% |
| Clinical | Hypertension Control Rate (Blood Pressure <140/90) | > 75% |
| Operational | Staff Turnover Rate | < 15% |
How Technology Enables Scalable Management
Scalability in family practice is impossible without a robust digital backbone.
- Digital Front Door: This includes online scheduling, digital registration, and automated check-ins. It reduces the need for front-desk staff during workforce shortages.
- Data Analytics: Use dashboards to monitor utilization metrics in real-time. If “no-show” rates spike on Tuesdays, the data will tell you why.
- Remote Patient Support and Hybrid Care: Remote patient management should be integrated into the workflow management system, not treated as a separate silo.
How CERTIFY Health Supports Family Practice Management
CERTIFY Health acts as the operational catalyst for high-performing primary care clinics, serving as a technical orchestration layer that integrates directly with existing Health IT infrastructure.
In an era of increasing margin compression, CERTIFY Health converts manual administrative bottlenecks into automated, high-fidelity data streams that protect a practice’s financial and operational health.
According to the CERTIFY Health Outpatient Pressure Index 2025™, clinics implementing digital intake platforms saw an average 60% reduction in check-in times and cut post-visit call volumes by 80% through secure messaging.
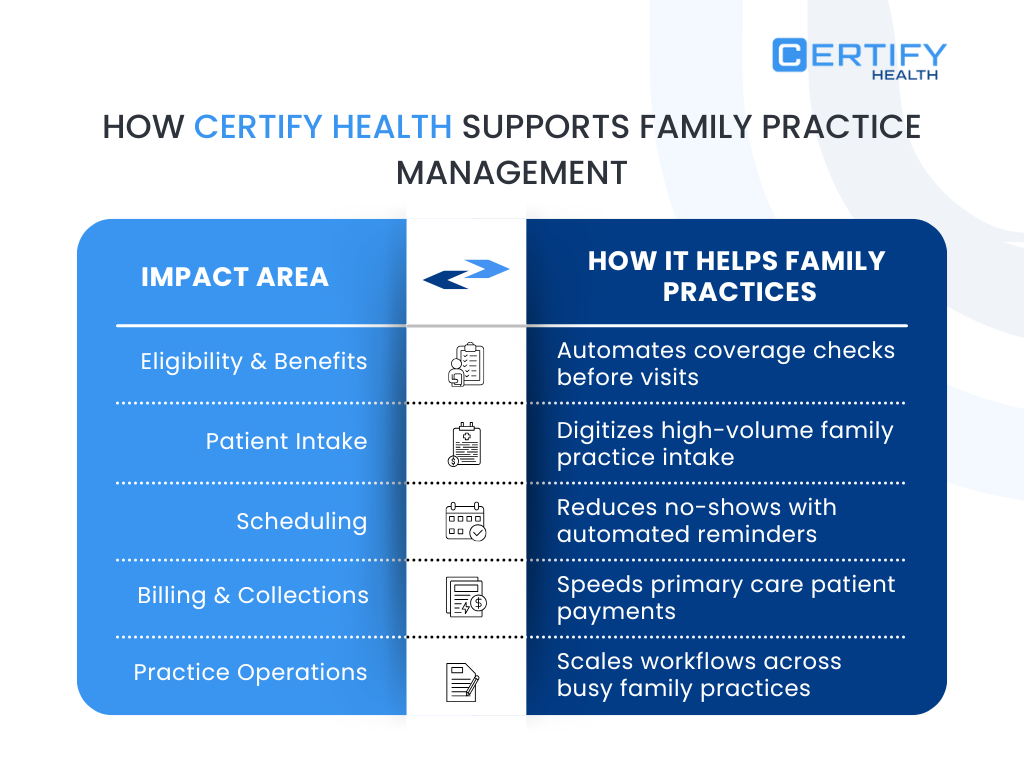
1. Re-engineering Patient Intake and Claims Accuracy
The “clipboard and paper” model is the primary driver of claim denials. Manual entry errors in patient demographics or insurance IDs lead to significant reimbursement pressure.
- Biometric Identity Verification: Utilizing FaceCheck biometric authentication, CERTIFY ensures 1:1 patient matching.
This eliminates duplicate records in the EHR and prevents medical identity theft, which is a critical component of management excellence.
- Real-Time Eligibility (RTE): CERTIFY automates insurance verification in under 60 seconds, compared to the 8–24 minutes required for manual checks.
By identifying coverage issues before the clinician encounter, practices drastically improve claims accuracy and protect operating margins.
- Digital eConsent and Forms: Patients complete all necessary documentation via mobile or kiosk before reaching the front desk, allowing for total role optimization of administrative staff.
2. Strategic Communication and Reducing Clinician Burnout
Fragmented communication is a leading cause of provider burnout. CERTIFY Health’s communication suite replaces traditional “phone tag” with structured, HIPAA-secure digital touchpoints.
- Automated Nudges and Reminders: Beyond simple appointment reminders, the platform uses AI-driven “check-in nudges” and “payment reminders,” which have been shown to reduce no-show rates by up to 38%.
- ASAP List & Waitlist Automation: When a cancellation occurs, CERTIFY Health’s ASAP List automatically reaches out to patients on the waitlist, ensuring high utilization metrics without manual staff intervention.
- Two-Way Secure Messaging: This allows for seamless continuity of care, enabling patients to ask follow-up questions or receive lab results without clogging the practice’s phone lines.
3. Data-Driven Practice Improvement
CERTIFY provides the granular data necessary for high-level clinical operations oversight.
- Real-Time Sentiment Analysis: By capturing patient experience metrics immediately post-visit, managers can identify and rectify operational friction (such as excessive wait times) before they impact the practice’s public reputation.
- Operational Benchmarking: Detailed reports on patient flow (from “check-in” to “roomed” to “discharged”) allow leadership to apply precise change management strategies to underperforming workflows.
- Bidirectional EHR Integration: CERTIFY Health’s “Plug & Play” connectivity ensures that all data (from insurance cards to clinical intake forms), syncs instantly with the EHR, maintaining a high-fidelity Health IT infrastructure.
Frequently Asked Questions (FAQ)
What does family practice management include?
It involves the integration of clinical care, human resources, financial oversight, and technological infrastructure specifically tailored for primary care.
How is family medicine different from internal medicine management?
Family medicine requires specialized workflows for pediatrics and immunizations, whereas internal medicine is often more focused on adult sub-specialty coordination.
How can small primary care clinics improve efficiency?
Focus on EHR optimization and role optimization. Every task done by a physician that a medical assistant could do is a loss of revenue.
Conclusion: Building Resilient, High-Performing Practices
The family practices that survive the next decade will be those that embrace management excellence as a technical discipline.
By focusing on preventive care, optimizing clinical operations, and leveraging advanced Health IT infrastructure, clinic leaders can ensure both financial viability and high-quality continuity of care.
The transition to value-based care is not a hurdle; it is an opportunity for those with the right data and workflows in place.