Table of Contents
Introduction
We still see SOAP notes as routine paperwork. That framing misses the point.
Clinical documentation is not a passive record. It is an operational control surface that shapes reimbursement, audit risk, clinician workload, and patient trust.
CMS reports improper payments across Medicare and Medicaid reached $47.9 billion in FY 2022. Poor documentation was a primary driver.
SOAP notes sit squarely at the center of this risk.
They can either convert clinical intent into billable, defensible data or quietly undermine revenue, compliance, and experience across the system.
The problem is not that clinicians write SOAP notes poorly.
The problem is that we treat them as clerical artifacts instead of infrastructure.
What Are SOAP Notes
- The SOAP note is a structured clinical documentation framework used to record the essential medical elements of a patient encounter.
- It captures what the patient reports, what the clinician observes, how findings are interpreted, and what actions are taken.
- Its primary purpose is to make medical necessity clear, visible, and defensible within the medical record.
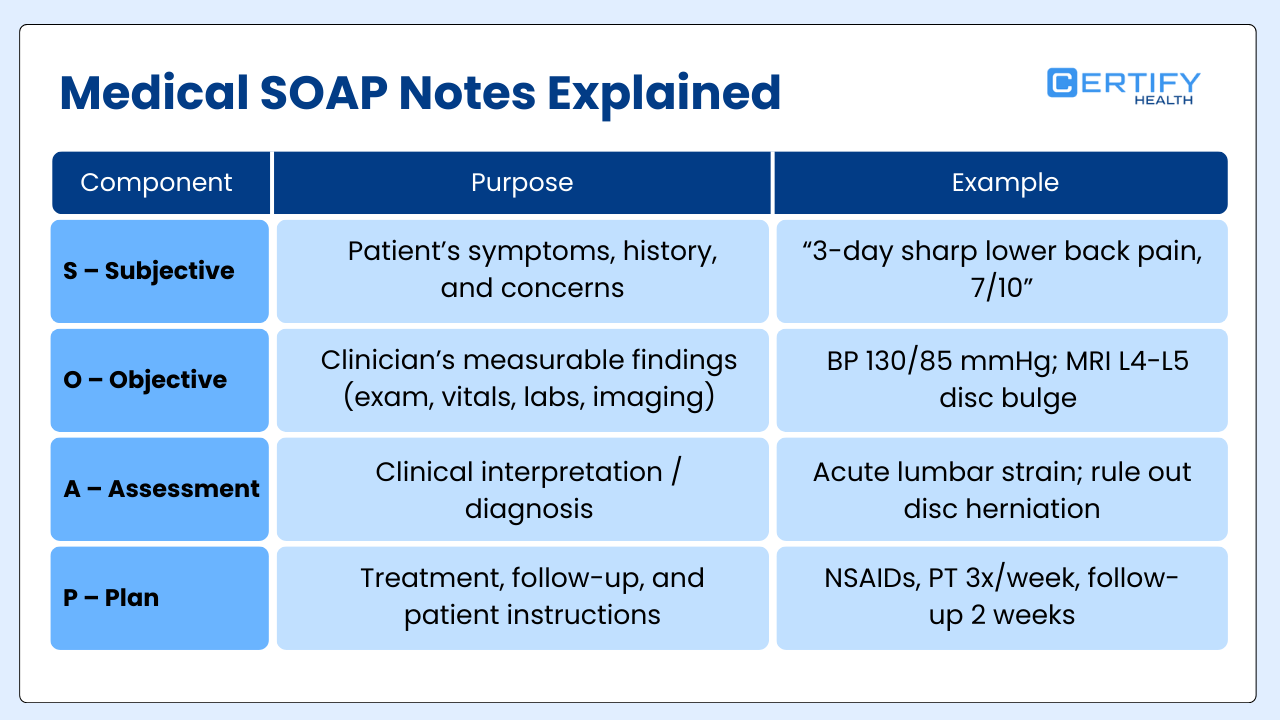
SOAP notes structure patient encounters in four sections: Subjective, Objective, Assessment, and Plan.
That’s correct….but incomplete.
The real purpose of SOAP notes is to preserve clinical reasoning.
Diagnostic errors affect about 5% of U.S. adults each year, nearly 12 million people. Poor documentation makes it harder to understand, review, and correct those errors over time.
When notes degrade into long, free-form narratives, they stop functioning as reasoning records. They become liabilities.
SOAP Framework Evolution Flowchart
The Origin (Late 1960s)
Developed by: Dr. Lawrence Weed
Goal: Move away from narrative documentation and intuition-based medicine.
The Shift: Organized Process
- Transition from “gut feeling” to a data-driven clinical process.
- Implementation of an organized structure for every patient encounter.
The Core Mechanism: Categorization
- Separation of Subjective and Objective observations.
- Separation of Assessment (diagnosis/logic) from Plan (action).
End Result: Clinical Excellence
- Explicit Reasoning: Makes the doctor’s thoughts clear to others.
- Reproducibility: Ensures consistent care across different providers.
SOAP Notes as a Strategic Data Asset
Hospitals still treat documentation as administrative overhead. That is a structural flaw.
SOAP notes generate the data that powers coding, utilization review, risk adjustment, quality reporting, and audit defense.
Yet clinicians are expected to produce this data manually in EHRs not optimized for cognitive work.
A peer-reviewed study in Annals of Internal Medicine found physicians spend 1.77 hours on EHR and desk work for every hour of patient care. This ratio is unsustainable. It treats high-value clinical cognition as low-value clerical output.
SOAP notes themselves are not the problem. The problem is asking humans to manufacture structured data manually at scale.
Shift From Narrative Documentation to Communicative Precision
Narrative notes feel flexible. They feel safe. Operationally, they are fragile.
Unstructured documentation buries medical necessity, obscures intent, and forces coders and auditors to infer reasoning after the encounter.
ONC reports that unstructured data reduces interoperability and secondary use, increasing rework and error risk.
SOAP notes impose discipline. They separate observation from interpretation and interpretation from action.
That separation improves diagnostic clarity. AHRQ estimates diagnostic errors cost the U.S. up to $100 billion annually when downstream testing, complications, and utilization are included.
Precision is not about writing more. It is about making decisions legible to humans and systems.
Why SOAP Notes Matter Beyond Documentation
Four enterprise outcomes hinge on SOAP notes:
- Revenue Cycle Management: Clear assessments and plans justify medical necessity under CMS guidelines.
- Compliance: Relevance under HIPAA Minimum Necessary rules protects patient privacy.
- Clinician Burnout: Documentation burden drives nights and weekend work.
- Patient Experience: Clarity, continuity, and trust depend on legible notes.
These are not separate domains. They share a single dependency: documentation quality.
Hospitals that treat SOAP notes as paperwork inherit downstream damage. Hospitals that treat them as infrastructure gain leverage.
The Invisible Cost of Clinical Documentation Burden
1. EHR Documentation vs Patient Care
Clinicians now spend more time on EHRs than on patients.
One ambulatory study found physicians spend an average of 16 minutes per patient encounter just documenting. ONC data shows an additional 1–2 hours daily outside scheduled hours, often called pajama time.
What is Pajama Time?
Pajama time is a healthcare informatics term that refers to the hours physicians spend working in the EHR outside of scheduled clinic hours, typically at night, early morning, or on weekends, often from home.
This time is unpaid, untracked, and corrosive. It is not a personal failure. It is a predictable outcome of systems that treat SOAP notes as clerical output.
2. Impact on Diagnostic Accuracy
Cognitive fatigue degrades judgment. Fatigue translates to increased diagnostic error, particularly in complex cases with multimorbidity.
Late, rushed, or copied-forward notes reduce rigor and clarity. Errors persist across encounters.
Documentation burden is a patient safety issue.
3. Impact on Billing and Revenue
Billing accuracy depends on documentation.
In 2024, the Centers for Medicare and Medicaid Services Medicare Fee-for-Service Improper Payments Report found that 7.66% of total Medicare FFS payments, approximately $31.7 billion, were classified as improper.
In the majority of cases, auditors could not determine whether the care provided met payment requirements because the clinical documentation was missing, unclear, or insufficient.
The care may have been delivered appropriately, but the record failed to make the clinical reasoning and necessity visible.
SOAP notes that lack precision create revenue risk before a claim is submitted.
4. Impact on Patient Leakage
Patient leakage is often attributed to scheduling or access. The root cause is often documentation.
Incomplete plans, vague follow up, and poorly documented referrals drive missed appointments and broken continuity.
Incomplete follow up increases downstream utilization and cost. Leakage is documented into existence.
5. HIPAA Minimum Necessary Principle
HIPAA requires only the minimum necessary information. Note bloat violates this principle.
Excess copying, templated text, and irrelevant data increase compliance risk without improving care.
HHS reported approximately 135 million individuals affected by healthcare breaches in 2023, with unnecessary data exposure a contributing factor.
SOAP discipline enforces relevance, not volume.
Note Bloat as Risk
- Compliance: Excessive documentation weakens audit defense. OIG audits flag volume without clarity.
- Clinical: Critical signals are buried. EHR research links overload to higher rates of medication and diagnostic errors.
- Revenue: Defensible documentation drives revenue. Note bloat obscures medical necessity and increases the likelihood of downcoding or denial.

Anatomy of a High-Impact SOAP Note
Creating a SOAP note that works for patients, clinicians, and hospital leadership requires more than filling four fields. Each section serves a distinct purpose in clinical reasoning, compliance, and revenue optimization.
1. Subjective (Capturing the Patient Narrative)
The Subjective section is where the patient speaks. Capturing this information accurately sets the foundation for everything downstream.
Purpose:
- Understand patient symptoms and concerns
- Provide context for diagnostic reasoning
- Document medical necessity for reimbursement
Frameworks That Help:
The OLDCARTS mnemonic ensures a structured narrative:
| Component | What It Captures |
|---|---|
| O – Onset | When symptoms started |
| L – Location | Where symptoms are felt |
| D – Duration | How long symptoms last |
| C – Character | Nature of the symptom (sharp, dull, etc.) |
| A – Aggravating/Alleviating | Factors that worsen or relieve |
| R – Radiation | Spread of symptoms |
| T – Timing | Frequency or pattern |
| S – Severity | Pain or symptom intensity |
Best Practices:
- Avoid verbatim transcripts. Summarize the narrative while preserving meaning.
- Capture actionable details, not every word spoken.
- Highlight patient priorities and concerns to guide planning.
Here’s how the flow looks like:
2. Objective (Data Without Duplication)
The Objective section is where clinical facts live. Vital signs, labs, imaging, and physical exam findings all belong here.
Best Practices:
- Reference flowsheets or prior documentation instead of re-entering the same values.
- Reduce clutter to avoid errors from overload.
- Ensure objective data supports assessments and medical necessity.
| Data Type | Example | Documentation Tip |
|---|---|---|
| Vitals | BP 138/86, HR 92 | Pull from EHR flowsheet |
| Labs | CBC, CMP | Reference latest lab result date |
| Imaging | Chest X-ray | Include report summary, not full text |
| Exam | Lung sounds, joint mobility | Structured, bulleted, not narrative prose |
Visual Flow:
3. Assessment (The Revenue-Critical Section)
The Assessment is the heart of clinical reasoning and revenue justification. It is where synthesis happens.
Key Elements:
- Clinical Synthesis: Combine subjective and objective data to create a coherent interpretation.
- Differential Diagnosis: List possible causes, reasoning for inclusion/exclusion.
- Medical Necessity Justification: Document why the encounter and interventions are justified.
Assessment vs Diagnosis Listing
| Approach | Risk/Benefit |
|---|---|
| Clinical Synthesis | Reduces ambiguity, supports coding and audits |
| Simple Diagnosis Listing | May trigger denials or downcoding |
Flow Concept:
4. Plan – Preventing Patient Leakage
The Plan is where follow-through meets revenue protection. Clear instructions prevent miscommunication, missed visits, and claim denials.
Core Components:
| Component | Example | Impact |
|---|---|---|
| Follow-ups | 2-week post-op check | Reduces missed appointments |
| Referrals | Cardiology consult | Ensures continuity of care |
| Patient Education | Medication instructions | Improves adherence and outcomes |
| Documentation Compliance | CMS E/M requirements | Reduces risk of claim denial |
Best Practices:
- Document specific timelines and responsible parties.
- Link plan to assessment to show medical necessity.
- Avoid vague instructions that could trigger leakage or downstream utilization.
Visual Flow:
Key Takeaways
- Each SOAP section has a distinct strategic purpose beyond record-keeping.
- Subjective captures patient narrative without unnecessary detail.
- Objective organizes data efficiently, avoiding duplication.
- Assessment synthesizes reasoning and justifies medical necessity.
- Plan closes the loop, prevents leakage, and protects revenue.
When hospitals treat SOAP notes as infrastructure rather than paperwork, these sections become levers for improved care, compliance, and financial performance.
APSO vs SOAP Notes: Why Modern Health Systems Are Reordering Documentation
The structure of clinical documentation is changing. Not because clinicians forgot how to write SOAP notes, but because EHRs exposed where the cognitive friction lives.
Many health systems are now reordering documentation from SOAP to APSO.
This is not a cosmetic change. It reflects how clinicians think, read, and act during care.
What Is the APSO Format
APSO reorganizes the same four elements but changes the sequence:
The content does not change. The workflow does.
Clinicians typically open a note looking for two things:
What is going on, and what are we doing about it. APSO puts those answers first.
Instead of scrolling through history and vitals to find intent, the clinical synthesis and action plan are immediately visible.
Why CIOs Prefer APSO in EHRs
From an IT and operations perspective, APSO aligns documentation with how EHRs are actually used.
CIOs care about three things documentation directly affects:
- Time in the EHR
- Data clarity for downstream systems
- Clinician adoption and satisfaction
APSO improves all three by reducing cognitive load and scroll depth. When assessment and plan appear first, reviewers, consultants, coders, and care team members find what they need faster.
This matters at scale. Small inefficiencies multiplied across thousands of notes become enterprise-level waste.
Reduced Scroll Fatigue for Care Teams
Scroll fatigue is not a usability nuisance. It is a safety and efficiency issue.
SOAP forces readers to move through narrative and data before reaching decisions. APSO surfaces decisions first, then allows users to dive deeper only if needed.
This mirrors how clinicians scan charts during handoffs, rounds, and urgent consults. Less scrolling means less missed information and fewer interruptions in cognitive flow.
Clinician Satisfaction and Efficiency Outcomes
Clinicians consistently report frustration when documentation feels disconnected from how they practice medicine.
APSO reduces that disconnect. By prioritizing reasoning and action, it:
- Shortens time to clinical understanding
- Improves handoff clarity
- Reduces after-hours documentation burden
Satisfaction improves not because APSO writes the note for the clinician, but because it respects how clinicians think.
SOAP vs APSO at a Glance
| Dimension | SOAP Format | APSO Format |
|---|---|---|
| Information Order | Data first, decisions later | Decisions first, data follows |
| Cognitive Load | Higher due to scrolling | Lower with early synthesis |
| EHR Navigation | Narrative-heavy upfront | Action-oriented upfront |
| Care Team Review | Slower to find intent | Faster clinical understanding |
| CIO Perspective | Legacy-compatible | Workflow-optimized |
| Clinician Experience | Functional but fatiguing | More intuitive and efficient |
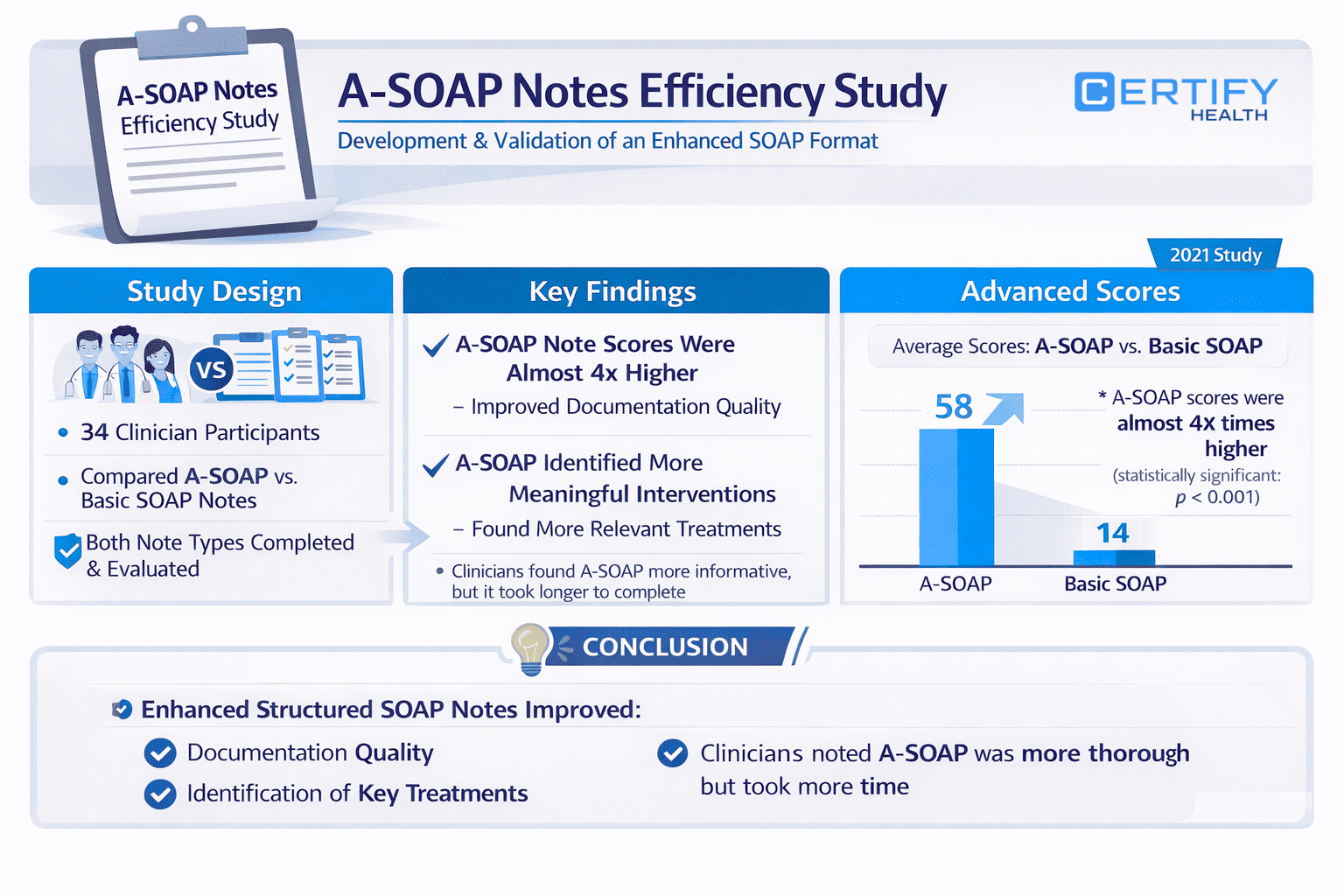
Evidence from Clinical Documentation Research
Real-world research underscores how thoughtful documentation design improves outcomes beyond theory.
A prospective study published in the Journal of Applied Pharmaceutical Science evaluated a redesigned advanced SOAP (A-SOAP) note against a more basic SOAP template among pharmacy students.
In the study, 34 postgraduate Pharm D students completed case scenarios using both formats.
Scores for documentation quality were significantly higher with A-SOAP (mean ~57.9) compared with the basic SOAP note (mean ~14.5), with strong statistical significance (p < 0.001).
This suggests that a more structured and thoughtfully framed template enhances the efficiency of problem identification and clarity of documentation.
- Participants also reported that A-SOAP helped them identify clinical interventions more specifically and improved their ability to frame plans.
While the advanced note took more time to complete on average, the increased specificity and clarity mirror what many health systems seek when evaluating documentation for care continuity, billing support, and interprofessional communication.
In other words, how clinicians are asked to organize information matters.
Structured innovation in note formats—whether A-SOAP for education or APSO in clinical workflows—can improve understanding, reduce variability, and align documentation with cognitive and operational needs.
Open Notes and the Bias Problem in Clinical Documentation
Clinical documentation was once written for clinicians alone. That is no longer true.
With Open Notes, patients are now readers of SOAP notes.
This shift has exposed a long-standing issue in healthcare documentation: bias, tone, and language that were never designed to be seen by the people they describe.
What is The 21st Century Cures Act
The 21st Century Cures Act mandates that patients have timely, electronic access to their clinical notes, including progress notes, consult notes, and SOAP documentation.
This policy did not change how clinicians think. It changed who can see the thinking.
What was once internal shorthand is now part of the patient experience. That has consequences.
Patient Access to Medical SOAP Notes
Today, patients routinely read their notes through patient portals. They see:
- How their symptoms are characterized
- How their behavior is interpreted
- How their concerns are prioritized or dismissed
For many patients, this is their first unfiltered view into clinical reasoning. Documentation tone now directly influences trust, engagement, and continuity.
SOAP notes are no longer just clinical artifacts. They are patient-facing documents.
Stigmatizing Language in Clinical Notes
Research consistently shows that stigmatizing language appears in clinical documentation, often unintentionally. Words that signal judgment rather than observation can change how patients perceive their care and how future clinicians interpret the record.
Examples of Language Shift in Healthcare Communication
| Problematic Language | Neutral, Clinical Alternative |
|---|---|
| “Non-compliant patient” | “Patient reports difficulty adhering to regimen” |
| “Drug-seeking behavior” | “Patient reports ongoing pain despite treatment” |
| “Poor historian” | “History limited due to recall difficulty” |
| “Refuses treatment” | “Patient declined after discussion of risks and benefits” |
Impact on Patient Trust
Patients who read notes that feel dismissive or judgmental are less likely to trust clinicians and the health system. Trust is fragile. Documentation can either reinforce it or quietly erode it.
Open Notes research has shown that respectful, transparent documentation improves patient understanding and engagement. Biased language does the opposite.
Trust is built line by line.
Impact on HCAHPS Scores
Patient perception of communication strongly influences HCAHPS performance. While HCAHPS does not measure documentation directly, documentation shapes the conversations patients remember.
When notes reflect listening, clarity, and respect, patients feel heard. When notes reflect bias or dismissal, that sentiment carries into survey responses.
Documentation tone has downstream financial implications.
Impact on Continuity of Care
SOAP notes are read not only by patients, but by future clinicians. Biased language can anchor impressions, influence decision-making, and perpetuate inequities across encounters.
Clear, neutral, and precise documentation improves handoffs, reduces misinterpretation, and supports safer continuity of care.
Bias does not stay in one visit. It propagates through the record.
Strategic Takeaway
Open Notes changed the audience for SOAP documentation. That change exposed a bias problem that was always there.
High-quality SOAP notes now require more than clinical accuracy. They require linguistic discipline. Neutral language protects patient trust, improves experience metrics, and preserves continuity of care.
In the Open Notes era, how clinicians write matters as much as what they write.
Future of SOAP Notes: Ambient AI and Real-Time Documentation
Clinical documentation is entering a transition phase. Not away from SOAP, but away from manual transcription.
The future of SOAP notes is not about typing faster. It is about capturing clinical intent as care happens, with minimal interruption to the human interaction at the center of medicine.
What Is Ambient Clinical Intelligence
Ambient Clinical Intelligence, often abbreviated as ACI, refers to systems that passively capture clinical conversations and signals during an encounter and convert them into structured documentation.
Instead of clinicians acting as scribes, ambient systems listen, contextualize, and organize information in real time. The clinician reviews and validates. The system handles the mechanical work.
This approach preserves the SOAP structure while reducing the cognitive and physical burden of documentation.
Real-Time SOAP Note Generation
In an ambient model, SOAP notes are drafted during the encounter, not reconstructed afterward.
- Subjective elements are captured from patient dialogue
- Objective data is pulled directly from devices and EHR feeds
- Assessment reflects clinician synthesis, not post-visit recall
- Plan is documented while decisions are made
This matters because documentation quality declines when notes are completed hours later, often under fatigue and time pressure.
Real-time generation aligns documentation with clinical reasoning, not memory.
Reduced Documentation Time per Provider
Federal and peer-reviewed research consistently shows that documentation consumes a disproportionate share of clinician time. Ambient and real-time approaches aim to reverse that ratio.
Early studies of ambient documentation tools show meaningful reductions in after-hours charting and so-called pajama time. The value is not just time saved, but cognitive energy preserved.
When SOAP notes are generated concurrently with care, clinicians spend less time reconstructing encounters and more time practicing medicine.
Patient Experience and the Return of Eye Contact
One of the most underappreciated effects of documentation burden is its impact on presence.
When clinicians are focused on screens, patients notice. When clinicians maintain eye contact, listen, and respond without interruption, trust improves.
Ambient documentation enables this shift by removing the need for constant typing. SOAP notes still exist, but they recede into the background.
Patient experience improves not because technology is visible, but because it is not.
Where Workflow Automation Fits In
Ambient AI does not operate in isolation. It depends on clean upstream and downstream workflows.
Tools that streamline patient intake, eligibility verification, consent capture, and structured data collection reduce the noise ambient systems must interpret. Platforms like CERTIFY Health, which focus on automating front-end patient access and intake workflows, help standardize the data entering the clinical encounter.
This matters because ambient documentation works best when the clinician is not compensating for missing or inconsistent administrative information. Clean inputs support cleaner notes.
SOAP Notes as a Strategic Asset for RCM and Patient Experience
Every SOAP note quietly connects three enterprise priorities that health systems usually manage separately: revenue integrity, clinician retention, and patient trust.
When documentation breaks down, all three erode together.
Documentation and Revenue Integrity
Revenue cycle performance starts with clinical documentation.
Clear assessments and defensible plans are what justify medical necessity under CMS evaluation and management guidelines. When SOAP notes lack synthesis, claims become vulnerable to denials, downcoding, and post-payment audits.
This is why documentation quality is now viewed as a revenue protection strategy, not a compliance afterthought.
Front-end workflows matter here. Incomplete intake data, missing histories, or unclear visit intent force clinicians to compensate inside the note.
Platforms like Certify Health, which focus on structured patient intake, eligibility verification, and pre-visit readiness, help ensure that clinicians start encounters with cleaner inputs. Cleaner inputs reduce ambiguity in SOAP notes, which directly supports downstream revenue integrity.
Documentation does not fix broken workflows. It reflects them.
Did You Know?
Documentation deficiencies are one of the most frequently cited reasons for claim denials in federal audits. The issue is rarely incorrect coding. It is unclear clinical justification upstream.
Documentation and Clinician Retention
Burnout is often framed as a workforce issue. It is also a documentation design issue.
Clinicians consistently report that documentation burden is a major driver of dissatisfaction and after-hours work. SOAP notes written late at night or reconstructed from memory are not just inefficient. They are demoralizing.
When intake, consent, and administrative data are collected before the visit, clinicians spend less time filling gaps and more time practicing medicine. Workflow tools like Certify Health do not replace SOAP notes. They reduce the administrative noise that makes SOAP notes harder to complete well.
Retention improves when documentation feels clinically meaningful rather than bureaucratic.
Did You Know?
Studies on so-called “pajama time” show that clinicians spend significant portions of their evenings completing notes. Reducing pre-visit administrative burden is one of the most effective ways to shrink that time.
Documentation and Patient Trust
In the Open Notes era, SOAP notes are no longer invisible to patients.
Patients read how their concerns are described, how decisions are explained, and whether plans are clear. Documentation tone now influences trust as directly as bedside communication.
When SOAP notes are precise, respectful, and consistent across visits, patients experience continuity. When notes are rushed, templated, or vague, patients feel dismissed or confused.
Trust is reinforced when the documentation matches the care experience.
Structured intake and clear pre-visit communication also play a role. When patients know what to expect before the visit and see their concerns reflected accurately afterward, confidence in the system grows.
Fascinating Facts About SOAP Notes
- SOAP notes are read by more people than they are written for, including coders, auditors, care teams, and patients.
- Documentation quality affects revenue outcomes before a claim is ever created.
- Poor documentation increases clinician workload downstream, not just at the point of care.
- Patients who understand their notes are more likely to follow care plans and maintain continuity.
Conclusion: SOAP Notes as Enterprise Infrastructure
SOAP notes were never just about documentation. Health systems treated them that way anyway, and the cost has been measurable.
In modern healthcare, SOAP notes function as enterprise infrastructure. They connect clinical reasoning to revenue integrity. They shape clinician workload and burnout. They increasingly influence how patients experience care through Open Notes and digital access.
The future is not about abandoning SOAP. It is about redesigning how SOAP fits into real clinical workflows.
Hospitals that recognize this shift move documentation upstream, reduce noise, and protect what matters most: clinical judgment, trust, and sustainability.
Key Takeaways
APSO Adoption
Reordering documentation to APSO reflects how clinicians read and think. Assessment and Plan first reduces scroll fatigue, improves handoffs, and aligns documentation with real-world use inside EHRs.
Bias-Aware Documentation
With Open Notes, language matters. Neutral, precise documentation improves patient trust, continuity of care, and experience metrics while reducing downstream misinterpretation.
AI-Assisted Workflows
Ambient and real-time documentation tools reduce after-hours charting and cognitive fatigue. When paired with clean intake and access workflows, SOAP notes become clearer and more defensible, not longer.
SOAP notes do not fail on their own. They fail when the systems around them do.
Frequently Asked Questions
Are SOAP notes still required in modern EHRs?
Yes. SOAP remains the dominant documentation structure across care settings. What is changing is how notes are organized, generated, and supported by upstream workflows.
Is APSO replacing SOAP?
Do better SOAP notes really affect revenue?
Yes. Documentation quality directly influences medical necessity justification, audit outcomes, and claim defensibility. Revenue risk often originates in the note, not the code.
How do Open Notes change documentation expectations
Patients now read clinical notes. This makes tone, clarity, and bias awareness essential for trust, continuity, and experience.
Will AI replace clinicians in documentation?
No. AI assists with capture and structure. Clinical judgment, assessment, and final validation remain human responsibilities.
Where CERTIFY Health Fits in Modern Documentation Workflows
High-quality SOAP or APSO notes do not begin at the point of typing. They begin with data readiness.
CERTIFY Health’s patient management software is designed to manage the full patient record across the encounter lifecycle, reducing fragmentation between intake, documentation, coordination, and follow-up.
This matters because documentation quality is constrained by what the system makes available, visible, and usable at the moment of clinical decision-making.
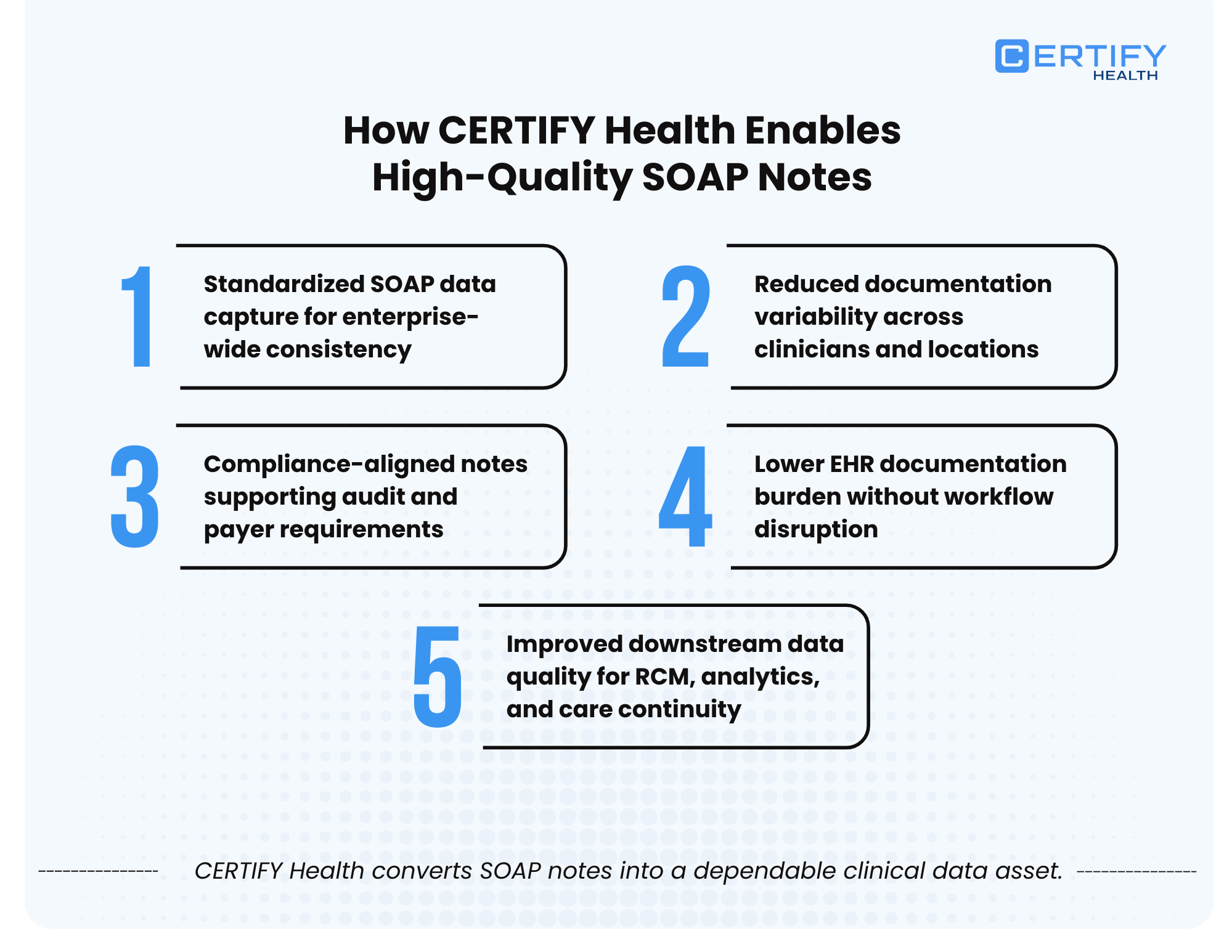
Effective documentation depends on context over time.
CERTIFY Health provides a longitudinal patient chart that surfaces vitals, clinical flags, history, and medications in a unified timeline. This reduces the need for clinicians to reconstruct history manually or search across multiple views.
When prior data is immediately accessible, assessments become more coherent and less repetitive.
SOAP note quality improves when clinicians are not re-entering facts.
CERTIFY Health supports encounter-level tools including vitals (manual or device-fed), allergies, and problem lists. These elements can be referenced rather than retyped, helping Objective sections remain factual and concise without duplication.
Reducing manual re-documentation directly lowers clutter-induced error risk.
CERTIFY Health supports SOAP notes, progress notes, diagnosis logging, attachments, and discharge summaries within the same patient record.
This allows documentation to evolve naturally across the encounter, rather than being fragmented across disconnected modules. Clinicians can preserve clinical reasoning while maintaining continuity between assessment, plan, and downstream documentation.
The result is less copy-forward behavior and clearer intent across visits.
AI-Powered Documentation as Assistive Infrastructure
CERTIFY Health includes AI-powered documentation tools such as real-time transcription, summaries, and assistive notes.
Used appropriately, these tools support clinicians by reducing manual typing and cognitive load, while keeping the clinician responsible for review and final judgment. This aligns with emerging best practices for ambient documentation, where AI assists but does not replace clinical reasoning.
When integrated into structured workflows, AI reduces time spent documenting without degrading note quality.
Care Coordination Embedded in Documentation
Documentation does not end at the note.
CERTIFY Health includes care coordination capabilities such as tasking, handoffs, and treatment plan workflows. This ensures that plans documented in SOAP or APSO notes are operationalized, not lost in free text.
Clear linkage between documentation and coordination reduces patient leakage and improves follow-through.
Orders, Results, and Document Management
CERTIFY Health supports lab and imaging orders with results linking, along with document repositories and attachments.
This allows Objective data to be referenced accurately within notes without re-documenting results, supporting both clinical clarity and audit defensibility.
Reporting, Insights, and Clinical Oversight
Documentation quality is measurable.
CERTIFY Health provides clinical dashboards and reporting, enabling organizations to monitor documentation patterns, completeness, and trends over time. These insights support continuous improvement efforts rather than one-time template changes.
CERTIFY Health supports HL7 and FHIR integration with a clinical audit trail.
This ensures that documentation workflows remain interoperable across systems and defensible during audits. Structured documentation, combined with auditability, strengthens compliance without increasing documentation volume.
Why This Matters
SOAP and APSO notes do not exist in isolation. They are the output of systems that manage patient data, clinician attention, and workflow design.
CERTIFY Health’s patient management platform supports documentation by ensuring that clinicians start encounters with complete, accurate, and structured information, and finish them with notes that are clearer, shorter, and more defensible.
Documentation quality improves when the system is designed to support clinical reasoning, not fight it.
CERTIFY Health supports pre-visit readiness: structured intake, eligibility verification, and patient-submitted context. When subjective and administrative inputs are clean before the encounter, APSO notes become shorter, clearer, and clinically sharper.
To learn more about optimizing your practice with a unified healthcare management system, please connect with the CERTIFY Health team. Book a demo.