Table of Contents
Zero-wait digital check-in is not a feature. It is an operational outcome.
In OB/GYN, where visits are frequent, time-sensitive, and emotionally loaded, waiting is not a nuisance. It is a system failure. Research consistently shows that wait time is one of the most controllable drivers of patient experience, staff workload, and downstream operational efficiency.
This blog explains how OB/GYN practices can achieve zero-wait digital check-in and zero-contact patient check-in using a five-step framework.
Why Zero Waiting Time Matters More in OB/GYN Than Any Other Specialty
OB/GYN Visit Complexity Creates Structural Check-In Bottlenecks
OB/GYN practices manage repeated visits per patient across pregnancy, postpartum, annual exams, imaging, and procedures. That creates higher intake density per patient than most outpatient specialties.
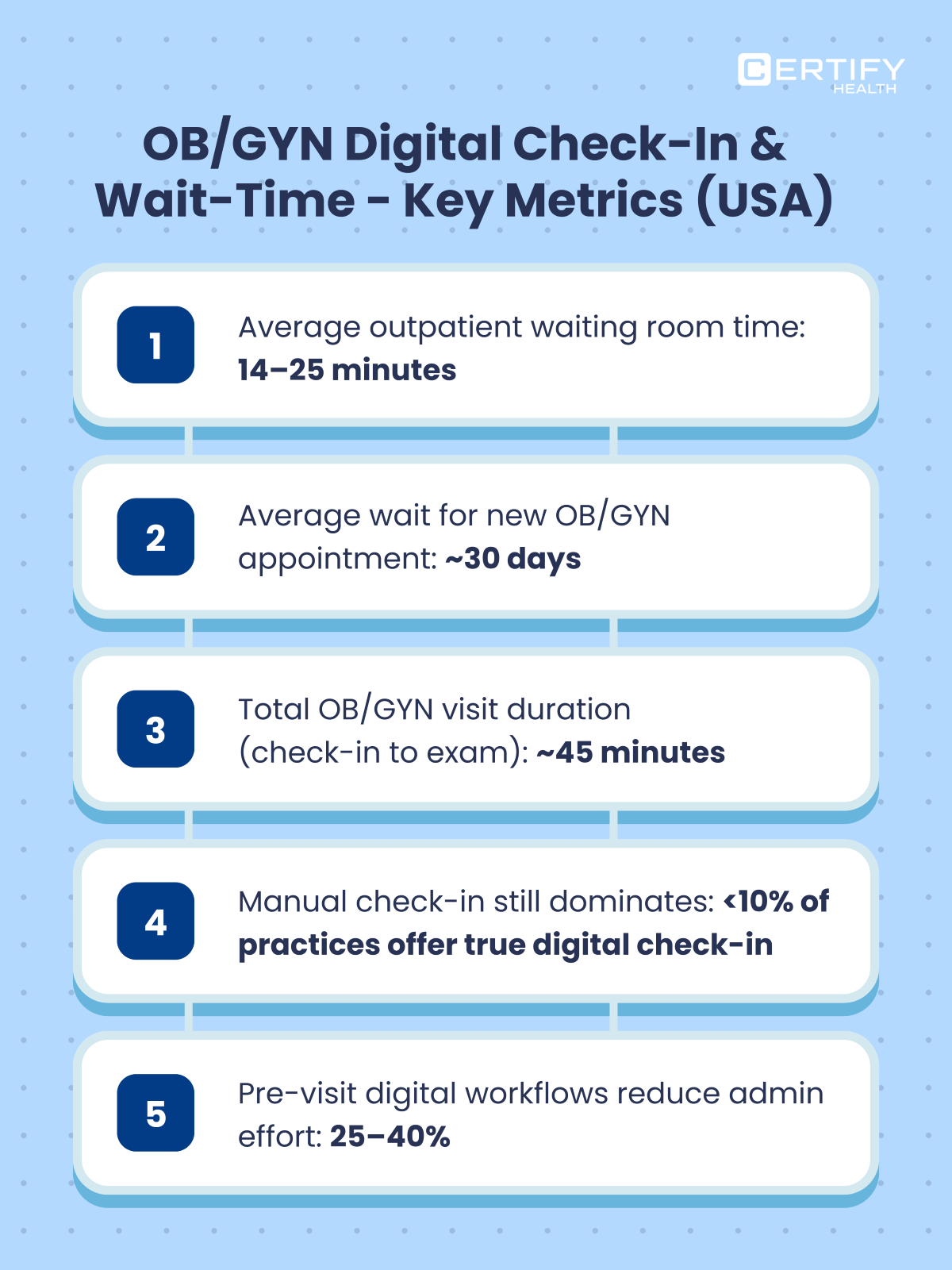
Outpatient data analyzing 21.4 million U.S. visits found that while the median wait time after the scheduled appointment was 4.1 minutes, 17 percent of patients waited more than 20 minutes and 10 percent waited more than 30 minutes before being seen.
Those delays are not random. They correlate with intake complexity and front-loaded administrative tasks.
In OB/GYN, intake is not simple demographics. It includes reproductive history, medication changes, insurance shifts, and visit-specific clinical data. When that work happens at arrival, waiting is inevitable.
The Hidden Cost of Waiting in OB/GYN Practices
Waiting time is not just a patient experience issue. It is an operational cost.
Inefficient front-end processes increase downstream congestion, causing provider schedule drift and staff overtime.
The Institute of Medicine explicitly defines timeliness as a core quality dimension of care and identifies waiting as a form of waste that health systems must design out, not manage around.
Zero-wait is not about speed. It is about removing waste before it shows up at the front desk.
What Zero-Wait Digital Check-In Actually Means
Zero-Wait Is an Operational Outcome, Not a Feature
Zero-wait does not mean no OBGYN waiting room. It means no administrative delay between arrival and clinical flow.
Operationally, zero-wait digital check-in requires:
- Intake completed before arrival
- No front-desk data re-entry
- No insurance correction at check-in
- No manual reconciliation between systems
Process redesign, not staffing increases, is the most effective way to reduce wait times.
Why Tablets in the OBGYN Waiting Room Do Not Eliminate Wait Times
Digitizing paper at arrival does not change arrival congestion. Moving work earlier in the care pathway produces materially better outcomes than speeding it up at the point of service.
If intake starts when the patient walks in, the bottleneck already exists.
Zero-wait starts upstream.
Common Reasons OB/GYN Digital Check-In Still Fails
Fragmented Systems Create Data Silos and Duplicate Work
- Healthcare interoperability failures are a documented contributor to inefficiency.
- Lack of system integration increases redundant data entry, which increases staff workload and delays patient flow.
- In OB/GYN practices using disconnected scheduling, intake, and billing systems, staff repeatedly touch the same data. Every touch adds time.
Static Forms Create Redundant and Irrelevant Questions
- Perceived waiting time increases when patients are asked unnecessary or repetitive questions, even if actual clock time does not change.
- Redundant questions increase patient frustration and reduce intake completion rates. That pushes work back to the front desk.
No Real-Time Eligibility or Demographic Validation
- Administrative complexity at intake increases arrival-to-service delays and contributes to downstream billing friction.
- Eligibility surprises are not billing problems. They are intake timing problems.
The 5-Step Framework to Achieve Zero-Wait Digital Check-In for OB/GYN
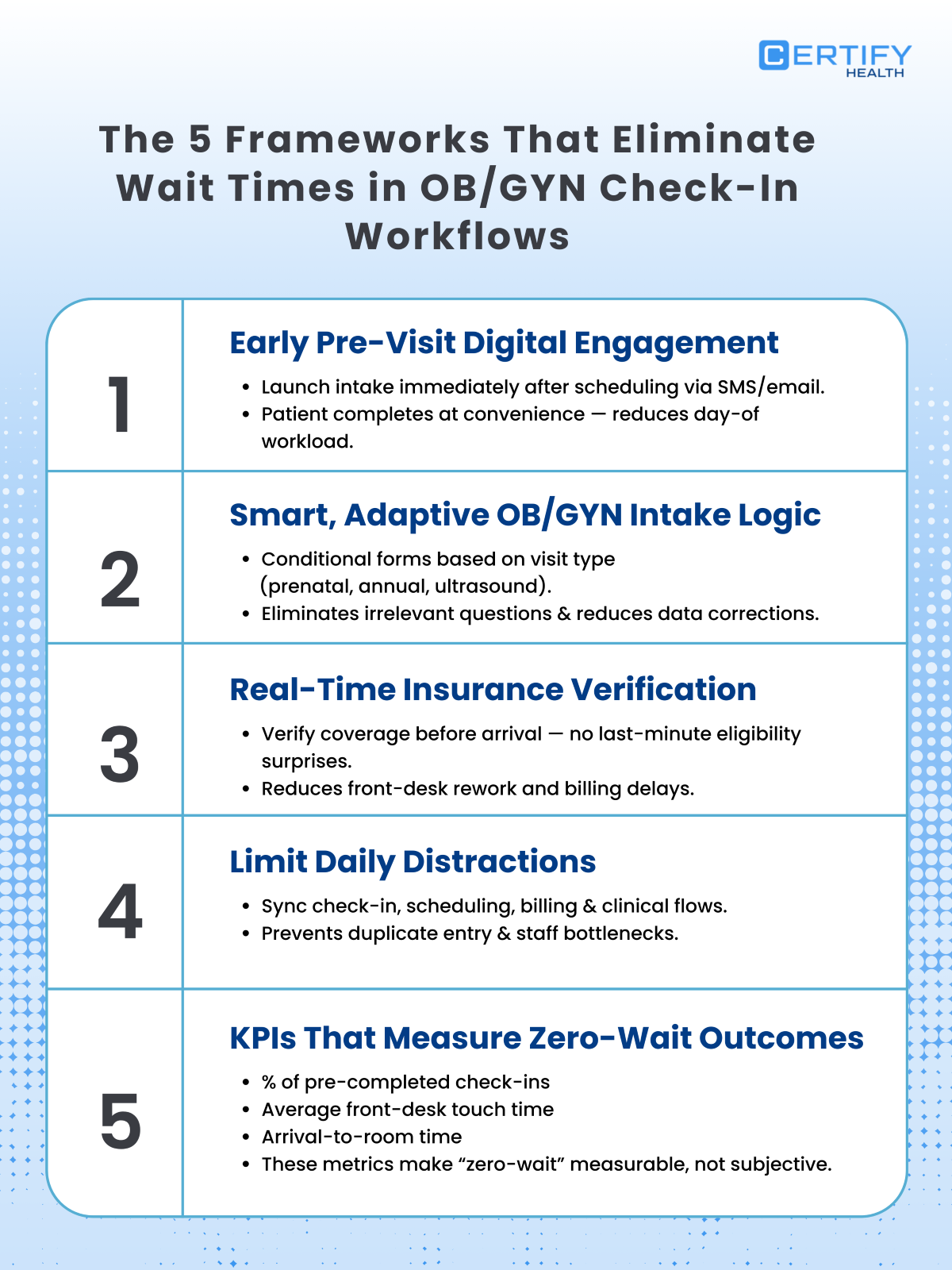
1. Start Digital Check-In at Scheduling, Not Arrival
Why Scheduling Is the True Beginning of Check-In
Early patient engagement reduces operational congestion later in the visit cycle.
A study found that advanced access scheduling reduced time-to-appointment availability by up to 32 days in outpatient settings.
The same principle applies to intake. If check-in starts at scheduling, arrival becomes a confirmation step, not a data-collection event.
Why Early Check-In Reduces Same-Day Chaos
Shifting even small amounts of work earlier in the patient journey produces disproportionate reductions in waiting.
A study found that saving 2.5 minutes per patient reduced average waiting time by 26 percent, while saving 5 minutes reduced waiting by nearly 55%.
Zero-wait is not about eliminating minutes. It is about relocating them.
2. Use OB/GYN-Specific, Smart Intake Flows
Adaptive Intake Is a Requirement, Not an Enhancement
OB/GYN visits vary significantly by type. Intake relevance directly affects completion rates and satisfaction, which in turn affects arrival readiness.
Static forms force patients through irrelevant questions. Adaptive forms respect visit context.
Eliminating Redundant Questions Improves Data Quality
Reducing duplicate data capture improves accuracy and reduces reconciliation effort, which directly impacts staff workload.
Cleaner data before arrival means no correction at arrival.
That is zero-wait.
3. Validate Insurance and Demographics in Real Time
Why Same-Day Eligibility Checks Create Waiting
Administrative burden research funded by AHRQ shows that unresolved administrative issues delay care delivery and increase staff task switching, a known driver of inefficiency.
Real-time eligibility verification before arrival eliminates this friction entirely.
Pre-Visit Validation Is the Foundation of Zero-Wait
A systematic review of federally indexed studies found that digital pre-visit workflows reduced average wait times by a weighted mean of 25.4 days across outpatient services.
The mechanism is simple. Problems resolved before arrival do not create lines.
4. Sync Check-In Data Across EHR, Billing, and Operations
Data Silos Create Duplicate Entry and Staff Burnout
The Agency for Healthcare Research and Quality identifies lack of interoperability as a root cause of redundant work and staff fatigue in outpatient settings.
Duplicate entry is not just inefficient. It is demoralizing. Staff burnout increases when clerical tasks crowd out meaningful work.
Why EHR-Agnostic Interoperability Matters in OB/GYN
Scalability and long-term adaptability are strong requirements for sustainable efficiency.
OB/GYN practices with multiple locations or evolving EHR environments cannot afford brittle integrations. Zero-wait requires durable interoperability.
5. Measure Zero-Wait as an Operational KPI
Zero-Wait Must Be Measured, Not Assumed
Federal outpatient benchmarks provide a clear reference point.
Across U.S. outpatient visits:
- Median wait after appointment time: 4.1 minutes
- 17 percent waited over 20 minutes
- 10 percent waited over 30 minutes
Zero-wait OB/GYN practices should measure:
- Percentage of check-ins completed pre-visit
- Arrival-to-room time
- Front-desk touch time per patient
What gets measured gets eliminated.
What Zero-Wait Digital Check-In Looks Like in Practice
| Before Zero-Wait | After Zero-Wait |
|---|---|
|
|
Final Takeaway: Zero-Wait Is Achievable with System Design
Federal research is clear.
Waiting is not inevitable.
It is designed in.
OB/GYN practices that achieve zero-wait do not work harder. They move work earlier, remove duplication, and measure what matters.
Zero-wait digital check-in is not a technology decision. It is an operational one.
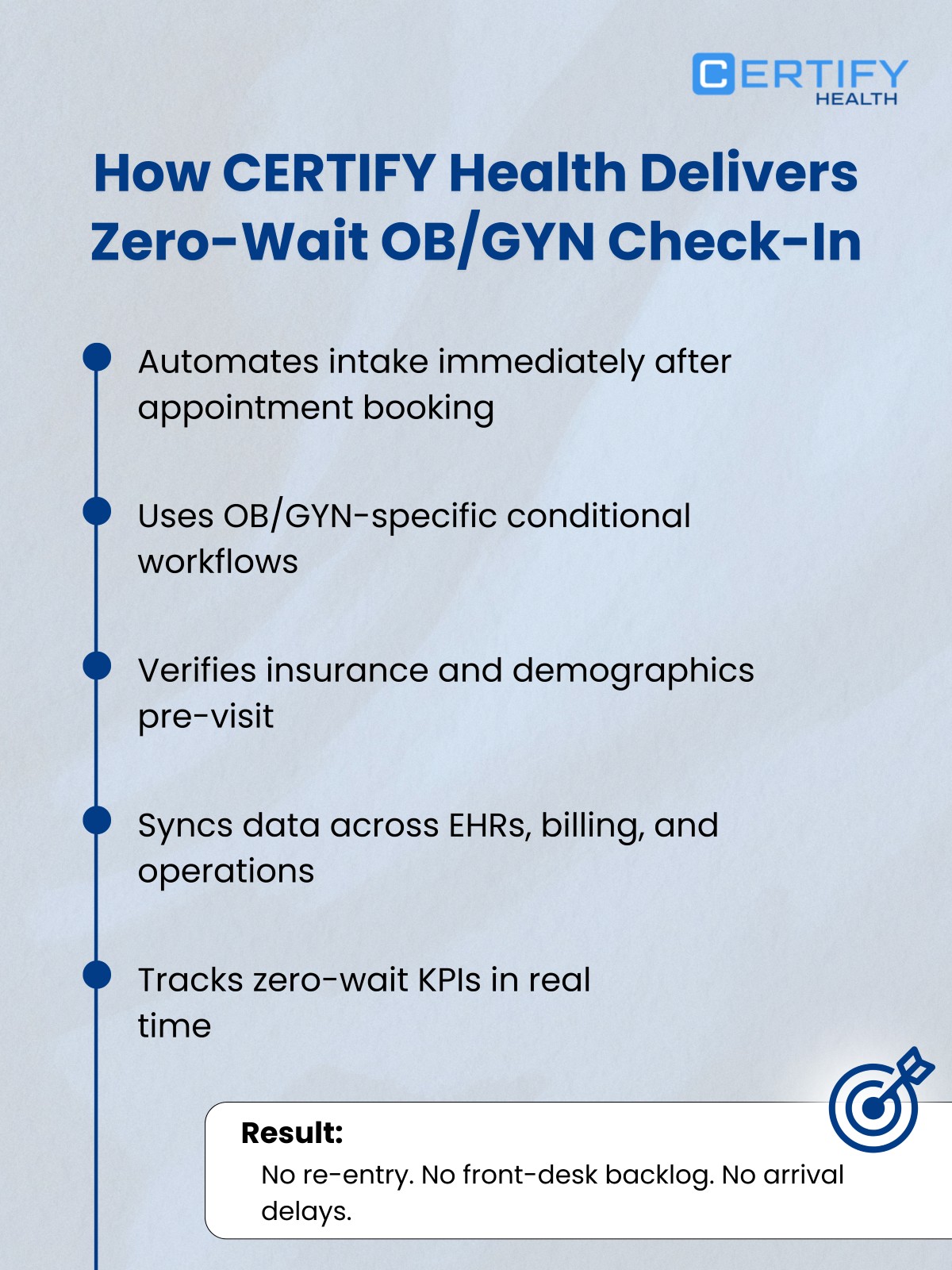
How CERTIFY Health Supports Zero-Wait Digital Check-In for OB/GYN
Zero-wait is achieved by starting work earlier, removing duplication, and integrating systems. Federal research consistently shows these are the levers that reduce waiting.
CERTIFY Health aligns to those principles:
- Check-in starts at scheduling, not arrival, reducing front-desk congestion
- OB/GYN-aware intake flows remove redundant and irrelevant questions
- Pre-visit demographic and insurance validation prevents arrival-time delays
- EHR-agnostic interoperability eliminates data silos and duplicate entry
- Operational metrics, not assumptions, define zero-wait readiness
CERTIFY Health does not promise zero-wait. It enables OB/GYN practices to achieve it through federally validated workflow design.