Table of Contents
The New Standard for Patient Management in Healthcare
Healthcare is under pressure like never before. Patient volumes are climbing, clinical staff are drowning in documentation, and fragmented systems create gaps that compromise safety and efficiency. From delayed lab results to mismanaged handoffs, these inefficiencies erode both patient trust and operational performance.
U.S. national health expenditures contributed to 17.6% of Gross Domestic Product (GDP) in 2023.
Clinicians face a dual burden: provide high-quality care while navigating disconnected workflows. Nurses manually track vitals, physicians juggle incomplete charts, and administrators struggle to maintain compliance. Every handoff, every delayed progress note, every misfiled document compounds the risk of inconsistent care and clinician burnout.
What Patient Management Software Really Means Today
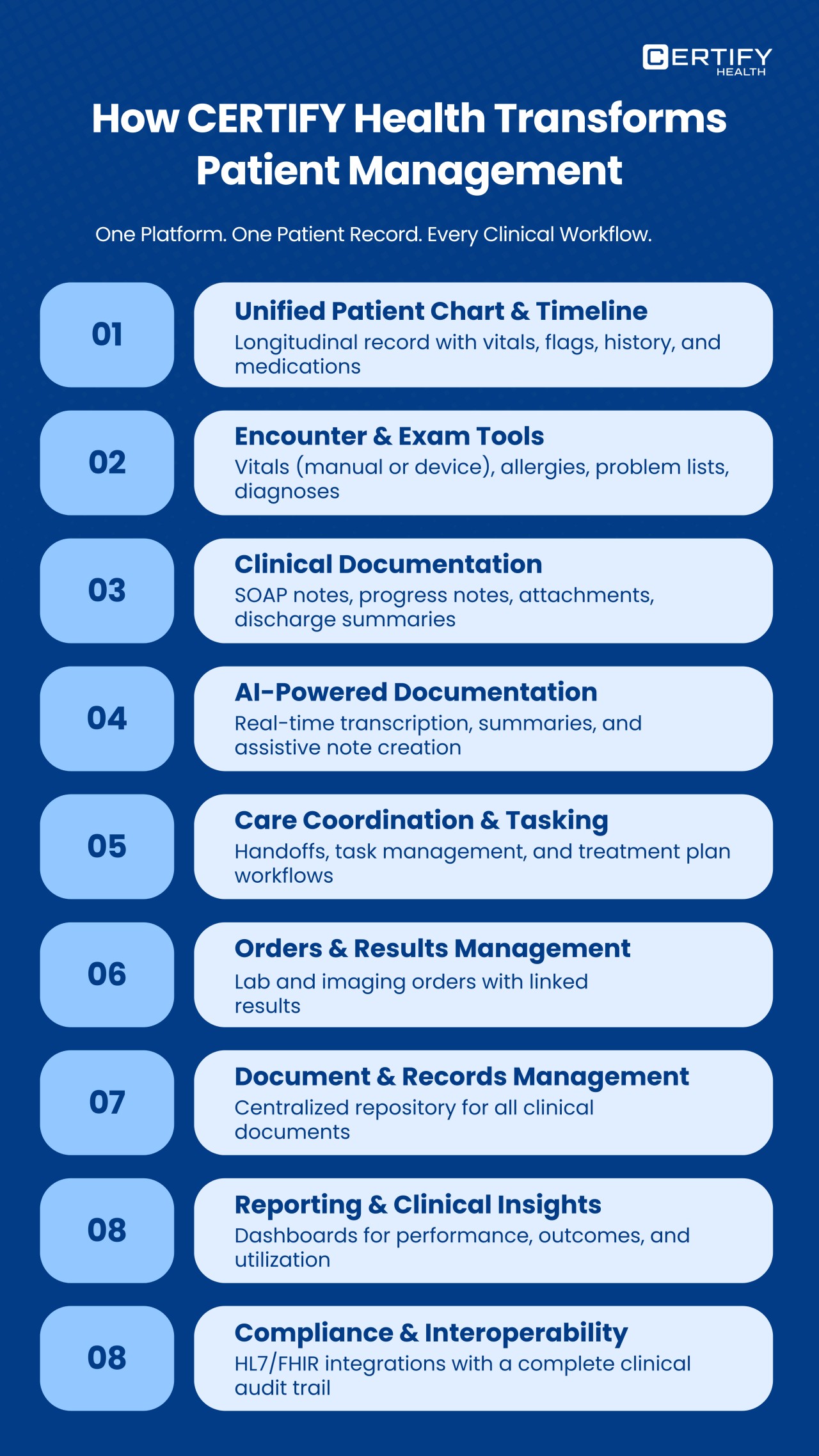
Patient management software is no longer a simple scheduling or billing tool. Modern solutions unify charting, documentation, task management, lab and imaging orders, care coordination, communication, and compliance monitoring into one intelligent platform.
With real-time visibility into longitudinal patient records and a comprehensive view of every encounter, teams can eliminate redundancies, streamline clinical workflows, and improve clinical decision support. Automated SOAP notes, progress notes, and discharge summaries reduce variability while enhancing clinical accuracy. Providers gain time back, documentation quality improves, and patients experience consistent, timely care.
Centralized patient management ensures that tasks, lab results, imaging orders, and clinical notes are always linked, traceable, and accessible. Rich text notes, AI-powered documentation, and real-time transcription elevate efficiency, providing actionable insights at the point of care.

Why Healthcare Organizations Are Redefining Patient Management
Healthcare leaders are recognizing that fragmented tools slow teams, obscure visibility, and create communication breakdowns. Practices are redefining patient management to:
- Connect care teams with unified tasking, handoffs, and care coordination workflows.
- Ensure consistent, high-quality documentation across providers.
- Enable AI-assisted clinical documentation and summary generation to reduce administrative burdens.
- Deliver real-time clinical insights to support faster, safer decision-making.
- Strengthen compliance with audit trails, HL7/FHIR integration, and standardized data exchange.
The goal is simple: eliminate friction, enhance team communication, and create a patient experience defined by clarity, timeliness, and trust.
How a Unified Platform Changes Everything
Modern platforms go beyond digitizing tasks—they transform care delivery. With longitudinal patient charts, providers see the full medical history in one place. Encounter tools ensure vitals, allergies, and problem lists are accurate and standardized. Clinical documentation templates enforce accuracy and consistency, while AI medical scribes capture notes in real time, generating summaries that reduce manual entry.
Care coordination modules route tasks, manage handoffs, and ensure nothing falls through the cracks. Orders for labs and imaging are linked directly to results, eliminating delays. Document management centralizes records, supporting images, PDFs, and external files with unified access. Dashboards and reporting deliver provider performance metrics, compliance tracking, and operational visibility.
Finally, interoperability frameworks ensure that HL7 and FHIR standards are met, enabling secure data exchange across EHRs and external systems. With all these pillars working in concert, teams operate efficiently, patients receive consistent care, and organizations realize measurable improvements in throughput and satisfaction.
The Hidden Operational Costs of Inefficient Patient Management
Administrative expenses for U.S. hospitals averaged 17% of total hospital expenses, based on analysis of 5639 hospitals. Inefficient patient management is more than a minor annoyance—it’s a hidden drain on resources, staff energy, and patient trust. Fragmented workflows, manual charting, and disconnected systems create operational bottlenecks that ripple across every part of a healthcare organization.
Documentation and Charting Inefficiencies
Physicians and nurses spend hours on manual charting, duplicating data, or piecing together fragmented records. When SOAP notes, progress notes, and discharge summaries are incomplete or inconsistent, care continuity suffers. Missing details in clinical documentation lead to coding errors, billing delays, and lost revenue.
A typical clinician can spend up to 35% of their day on documentation, cutting into patient interaction time. High administrative burden fuels provider burnout, increases the risk of mistakes, and reduces overall throughput.
Delayed or Missed Results and Follow-Ups
Without real-time visibility into lab orders, imaging results, and other critical data, follow-ups slip through the cracks. Tests are delayed, abnormal results go unnoticed, and patients wait longer for interventions. Missed follow-ups impact quality metrics, compliance, and patient satisfaction.
Fragmented workflows create a vicious cycle: delayed documentation leads to delayed results, which leads to more manual tracking and frustrated staff.
Provider Burnout Fueled by Manual Workflows
Manual workflows drain clinicians. Repetitive entry of the same patient data, scanning documents into multiple systems, or coordinating handoffs across teams consumes mental bandwidth.
Providers report feeling pulled between patient care and administrative chores. Burnout is directly linked to errors, lower retention rates, and declining care quality. A modern patient management software reduces these burdens by automating documentation and providing AI-powered clinical transcription.
Communication Breakdowns Across Teams
Communication breakdown is a leading cause of inefficiency in healthcare. When care teams rely on fragmented emails, sticky notes, or multiple disconnected platforms, tasks are overlooked, and critical information is lost.
Care coordination suffers. Nurses may miss handoff updates. Physicians may not see new lab results. Administrators struggle to track task completion. The result: inconsistent care, duplicated effort, and wasted time.
Compliance Gaps and Untraceable Data Movements
Regulatory requirements demand full auditability. Manual systems often fail to produce audit trails, leaving organizations exposed to compliance risks. Missing or inaccurate documentation can result in penalties, denied claims, or failed quality audits.
Inefficient document management—from unorganized files to inconsistent tagging—creates gaps in data security and unified access. This not only threatens compliance but slows clinical workflows and frustrates staff.
Lack of Real-Time Insights for Clinical Decision Support
Without consolidated data, providers lack clinical insights needed for evidence-based decisions. Decision-making is reactive, not proactive. Delays in seeing patterns across longitudinal patient records or cumulative provider performance metrics result in preventable errors and inconsistent care.
Patient Experience Impact
Patients feel the consequences of inefficiency. Longer waits, repeated questioning, and inconsistent care erode trust. Delays in diagnoses, incomplete documentation, or missed follow-ups make the experience frustrating and potentially unsafe.
The Solution: Integrated Patient Management
A fully integrated patient management system addresses every pain point. By combining charting, documentation, care coordination, orders, and compliance monitoring into a single platform, organizations regain control of workflows.
Clinicians access longitudinal patient records instantly. AI-powered documentation accelerates note completion. Tasking and handoffs are reliable and traceable. Lab and imaging orders are linked to results in real time. Compliance monitoring ensures audit-ready workflows.
The result is a transformed clinical environment: faster documentation, reduced errors, coordinated care, and measurable improvements in both patient outcomes and operational efficiency.
The 9 Core Pillars of Modern Patient Management (Deep-Dive)
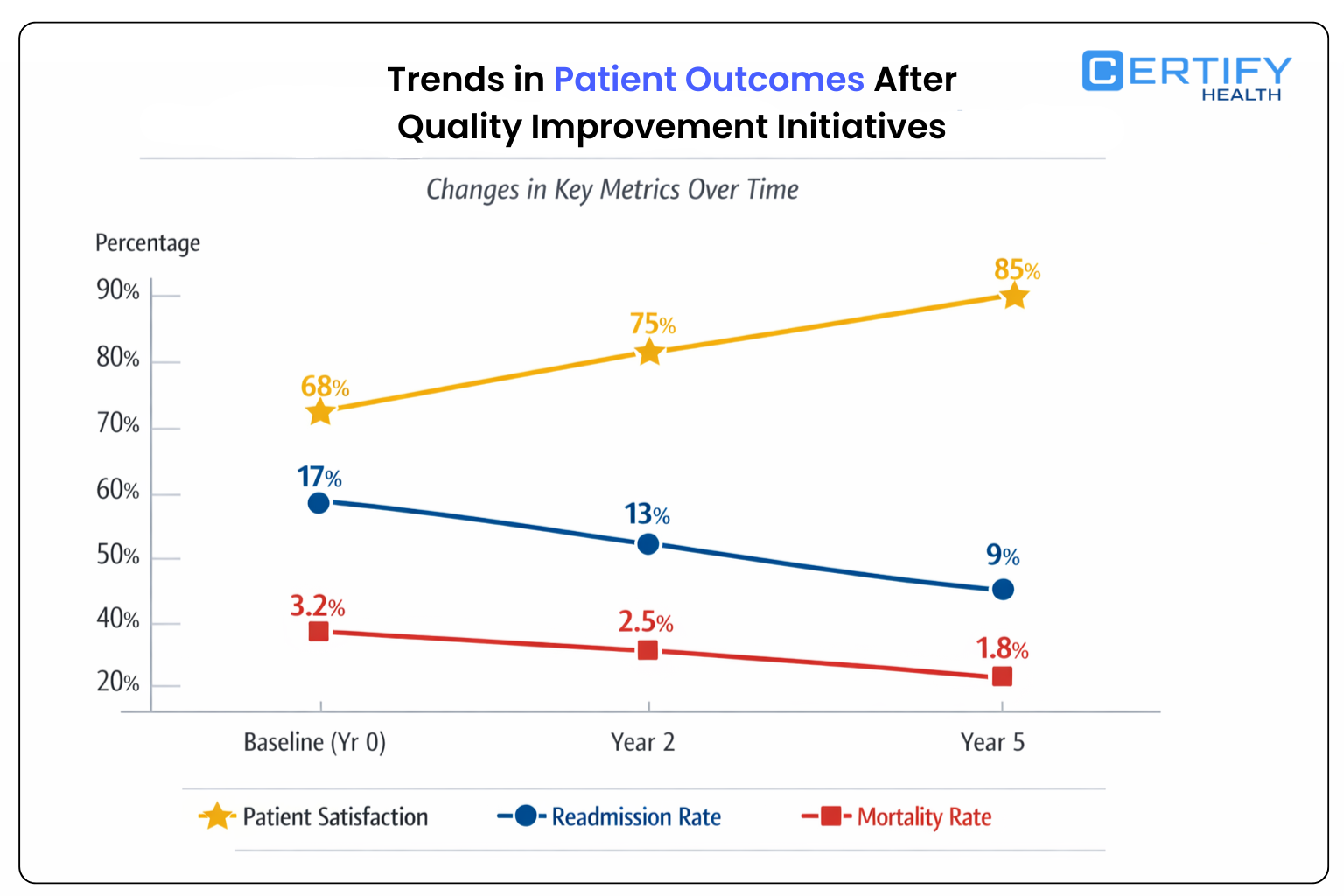
A modern patient chart and timeline is the backbone of effective clinical workflow. Fragmented charts and disconnected records create communication breakdowns, inconsistent care, and unnecessary administrative work. A unified chart gives clinicians real-time visibility into every aspect of a patient’s medical history. Quality Patient Management Software contributed to 34% improvement in specific key indicators comparing baseline to follow-up periods.
Key Features of a Longitudinal Patient Record
| Feature | Description | Benefit |
|---|---|---|
| Chronological Timeline | Conditions, medications, allergies, vitals, procedures | Provides a comprehensive view of patient history |
| Multi-Provider Access | Simultaneous access for physicians, nurses, specialists | Eliminates duplication and ensures everyone is on the same page |
| Clinical Context | Embedded notes, lab results, imaging, and visit summaries | Enables informed clinical decision support |
| Real-Time Updates | Automatic updates from lab systems, devices, and other EHRs | Ensures high-quality documentation without manual entry |
| Alerts & Notifications | Flag abnormal labs, critical medications, or follow-ups | Reduces inconsistent care and missed interventions |
Why a Unified Timeline Matters
- Eliminates Fragmentation: All data from multiple encounters is visible in one chronological sequence. No more flipping between multiple charts or systems.
- Supports Accurate Clinical Decision-Making: Physicians can see trends in vitals, lab results, and progress notes to make timely, informed decisions.
- Improves Communication Across Teams: Nurses, MAs, and providers instantly see updates, avoiding missed handoffs or duplicated tasks.
- Enhances Patient Experience: When providers have a complete view, patients experience coordinated care without repeated questioning.
Best Practices for Chart & Timeline Management
- Standardize data entry for vitals, allergies, and problem lists.
- Use rich text notes for context but embed structured data for reporting and coding.
- Enable unified access to ensure care teams see updates in real-time.
- Integrate with AI-powered documentation to reduce manual charting burden.
By centralizing patient history in a longitudinal patient record, healthcare organizations eliminate the risks associated with fragmented charts, support continuous care, and create actionable clinical insights for all providers.

Efficient encounter tools are essential for accurate patient management. Manual entry, inconsistent problem lists, and disconnected vitals capture lead to errors, documentation delays, and communication breakdowns. Modern tools unify data entry, standardize workflows, and lay the foundation for high-quality clinical documentation.
Core Components of Encounter Tools
| Component | Description | Benefit |
|---|---|---|
| Vitals Capture | Manual entry + device integration | Accurate, consistent measurement for every encounter |
| Allergy Management | Unified entry for drug, food, and environmental allergies | Reduces adverse events and supports safe prescribing |
| Problem List Standardization | Structured problem lists across visits | Ensures clinical accuracy and continuity of care |
| Medication Reconciliation | Auto-sync with pharmacy or EHR | Minimizes errors and inconsistent care |
| Encounter Templates | Condition-specific templates for documentation | Streamlines SOAP notes, progress notes, and discharge summaries |
Core Components of Encounter Tools
- Accuracy and Consistency: Manual entry errors are minimized. Allergies, meds, and vitals are captured reliably.
- Supports High-Quality Documentation: Standardized problem lists and templates improve clinical documentation quality for billing, compliance, and decision-making.
- Saves Time for Providers: Device integration and pre-filled templates reduce clicks, allowing clinicians to focus on patient care.
- Improves Inter-Team Communication: Nurses, MAs, and physicians access the same verified data, preventing errors during handoffs.
Best Practices for Encounter Management
- Integrate vitals devices for real-time transcription of measurements.
- Maintain structured allergy and problem lists to support longitudinal patient records.
- Use templates for common conditions to reduce variability in SOAP notes and progress notes.
- Ensure unified access so the care team can see updates immediately.
- Automate reminders for missing or abnormal data to support clinical decision support.
By implementing robust encounter tools, healthcare organizations create a foundation for accurate diagnoses, complete progress notes, and efficient care coordination. This eliminates fragmented workflows, strengthens comprehensive patient views, and enables faster, safer clinical decisions.
High-quality clinical documentation is the backbone of modern patient management. Accurate SOAP notes, progress notes, diagnoses, and discharge summaries ensure continuity of care, support billing and compliance, and enable efficient clinical decision support. Fragmented or inconsistent documentation leads to errors, delayed care, and increased administrative burden.
Key Elements of Clinical Documentation
| Element | Description | Benefit |
|---|---|---|
| SOAP Notes | Structured Subjective, Objective, Assessment, Plan | Standardizes encounter documentation, improves care consistency |
| Progress Notes | Chronological updates for ongoing care | Tracks patient evolution and informs subsequent decisions |
| Diagnoses | Standardized ICD coding and clinical accuracy | Supports billing, compliance, and quality reporting |
| Discharge Summaries | Summary of encounter, instructions, and follow-ups | Ensures safe transitions and patient comprehension |
| Rich Text Notes | Embedded images, PDFs, lab reports | Provides context for complex cases and multidisciplinary teams |
Why High-Quality Clinical Documentation Matters
- Continuity of Care: With accurate progress notes and discharge summaries, every provider has a clear view of patient history.
- Clinical Accuracy: Structured templates reduce variability and errors in diagnoses, ensuring safe treatment decisions.
- Operational Efficiency: Standardized documentation decreases charting time, reduces redundant data entry, and accelerates SOAP notes completion.
- Billing and Compliance: Accurate documentation ensures correct coding, supports audits, and reduces claim denials.
- Patient Safety: Comprehensive and precise records minimize risks associated with inconsistent care or missed follow-ups.
Best Practices for Clinical Documentation
- Use templates for SOAP notes and condition-specific encounters to ensure completeness.
- Incorporate rich text notes with embedded lab results, imaging, or external reports to enhance context.
- Enable AI-powered documentation to assist with summary generation and reduce manual errors.
- Ensure real-time updates to longitudinal patient records for comprehensive view across encounters.
- Implement structured data capture for clinical insights and decision support.
Impact on Clinical Workflows
Modern documentation tools reduce friction across care teams. Providers can complete notes faster without sacrificing quality. Nurses and support staff have instant access to accurate records for handoffs. Administrators gain transparent audit trails, and leadership can track provider performance metrics in real time.
Investing in robust clinical documentation systems is not optional; it’s essential. High-quality documentation empowers teams, supports patient safety, enhances compliance, and directly impacts operational efficiency and satisfaction across the healthcare ecosystem.
4. AI-Powered Documentation
The era of manual charting is over. AI-powered documentation transforms how clinicians capture, generate, and manage clinical notes. From AI medical scribes to real-time transcription and summary generation, modern tools reduce administrative burden, improve clinical accuracy, and accelerate workflow efficiency.
Core Components of AI-Powered Documentation
| Component | Description | Benefit |
|---|---|---|
| AI Medical Scribe | Captures clinical conversations in real time | Reduces manual note-taking, ensures accuracy, frees provider time |
| Real-Time Transcription | Converts verbal dictation into structured notes | Immediate access to patient data, eliminates transcription delays |
| Summary Generation | Auto-generates visit summaries and discharge notes | Streamlines workflow, improves coding completeness, supports clinical decision support |
| Intelligent Templates | Context-aware templates adapt to encounter type | Reduces variability in SOAP notes and progress notes |
| Integration with EHR | Auto-populates longitudinal patient record | Ensures comprehensive view across all encounters |
Why AI Documentation Matters
- Reduces Administrative Burden: Clinicians spend less time typing and more time on patient care. Studies show AI medical scribes can reduce documentation time by up to 50%.
- Ensures Clinical Accuracy: Real-time transcription and AI suggestions minimize errors in diagnoses, progress notes, and discharge summaries.
- Improves Compliance: Auto-generated summaries maintain audit trails and support regulatory adherence without extra work.
- Accelerates Decision-Making: AI highlights abnormal labs, missed follow-ups, or care gaps, empowering faster, safer decisions.
Best Practices for AI Documentation
- Enable real-time transcription during patient encounters for immediate note creation.
- Use AI-generated summaries to populate SOAP notes, progress notes, and discharge summaries efficiently.
- Integrate AI tools with care coordination and tasking modules to ensure updates are actionable.
- Monitor AI suggestions for clinical accuracy to maintain provider oversight.
- Combine AI notes with rich text attachments like lab results or imaging for a complete picture.
Impact on Clinical Workflow
AI-powered documentation creates a seamless bridge between patient encounters and structured records. Providers complete notes faster, high-quality documentation improves coding accuracy, and communication breakdowns are minimized. Multi-provider teams gain real-time visibility into patient status, while administrators have immediate access to compliant, traceable records.
By automating repetitive documentation, organizations can:
- Reduce clinician burnout by minimizing manual entry
- Improve consistency in SOAP notes, progress notes, and diagnoses
- Enhance patient experience with faster, coordinated care
- Unlock clinical insights and data-driven decision-making
AI-powered documentation is no longer a luxury; it’s a necessity for modern healthcare organizations. When combined with longitudinal patient records, comprehensive views, and structured clinical documentation, it transforms clinical workflow into a highly efficient, error-resistant, and patient-centered process.
5. Care Coordination
Effective care coordination ensures that every patient receives seamless, safe, and timely care. In fragmented systems, tasks are missed, handoffs are unclear, and treatment plans are inconsistently followed. Modern patient management platforms integrate tasking, handoffs, and treatment plan workflows to close these gaps.
Core Components of Care Coordination
| Component | Description | Benefit |
|---|---|---|
| Tasking | Assign, track, and complete tasks for care teams | Ensures accountability and timely action |
| Handoffs | Structured transfer of patient information between shifts or departments | Reduces errors and communication breakdowns |
| Treatment Plan Workflows | Multi-step plans with clear ownership | Guarantees that all care steps are executed |
| Alerts & Notifications | Automated reminders for pending or overdue tasks | Prevents missed follow-ups and critical care delays |
| Role-Based Access | Clinicians see tasks relevant to their role | Streamlines workflow and avoids overload |
Why Care Coordination Matters
- Eliminates Gaps in Patient Care: Structured handoffs and tasking ensure that nothing falls through the cracks.
- Supports Multi-Provider Teams: Physicians, nurses, and support staff have a shared view of responsibilities and timelines.
- Enhances Patient Safety: Automated reminders reduce missed follow-ups, delayed treatments, and inconsistent care.
- Improves Operational Efficiency: Standardized workflows reduce redundant communication and streamline daily operations.
Best Practices for Care Coordination
- Assign tasks to specific roles to ensure accountability.
- Standardize handoffs with structured templates for clarity.
- Integrate treatment plan workflows with longitudinal patient records for full context.
- Enable alerts for critical tasks, follow-ups, and abnormal results.
- Track completion metrics to identify bottlenecks and optimize workflows.
Impact on Clinical Workflow
By embedding care coordination into the patient management system, organizations can:
- Streamline tasking across departments
- Improve handoff reliability and reduce communication breakdowns
- Ensure that treatment plans are consistently followed
- Enhance provider confidence and reduce burnout
- Deliver a coordinated, patient-centered experience
Care coordination is the linchpin of effective modern healthcare. When combined with longitudinal patient records, AI-powered documentation, and structured encounter tools, it guarantees that patients move safely and efficiently through every step of their care journey.
6. Orders & Results
In modern clinical workflows, managing lab orders, imaging orders, and result tracking is a critical challenge. Delays, manual follow-ups, and disconnected systems lead to missed results, delayed diagnoses, and frustrated patients. Unified order management ensures clinicians see every result in real time and can act immediately.
Streamlining Orders
A modern platform integrates all lab and imaging orders into a single workflow. Clinicians can:
- Place orders directly from the patient chart.
- Track status and completion without switching systems.
- Automatically link results to the longitudinal patient record.
This integration eliminates redundant entry, reduces transcription errors, and ensures that abnormal results trigger alerts for timely intervention
Linking Results to Clinical Context
Simply receiving a result is not enough. Clinicians need context. Unified platforms automatically attach lab and imaging results to the encounter, linking them to:
- Active problems in the problem list
- Recent SOAP notes and progress updates
- Relevant medications and allergies
This linkage provides a comprehensive view of the patient’s condition, enabling clinical decision support and reducing diagnostic errors.
Benefits Across the Care Team
- Providers: Access complete results in real time, reducing delays in diagnoses and follow-ups.
- Nurses & MAs: Monitor pending orders and notify providers proactively.
- Administrators: Track order completion and identify bottlenecks for operational efficiency.
Key Advantages
- Eliminates missed results or delayed follow-ups
- Supports structured documentation and clinical accuracy
- Reduces time spent on manual tracking and phone calls
- Enhances patient trust through faster, coordinated care
By unifying orders and results management, healthcare organizations minimize risk, enhance team communication, and improve overall workflow efficiency. When combined with AI-assisted documentation, encounter tools, and care coordination, this creates a seamless loop where every test and result contributes directly to better patient outcomes.
Effective document management is critical to modern patient management. Clinical teams handle a wide range of files—lab reports, imaging studies, PDFs, scanned forms, and external records. Without a centralized system, documents are scattered across multiple platforms, creating delays, errors, and compliance risks.
Centralized Secure Repository
A modern patient management platform offers a secure repository where all patient documents are stored in one place. Key features include:
- Role-based access: Clinicians see only the records relevant to their role, maintaining privacy and compliance.
- Attachment support: Images, PDFs, and external files can be linked to patient charts.
- Search and retrieval: Standardized tagging ensures fast access during encounters.
Unified Access Across Teams
Unified access eliminates the need for repeated requests or redundant scanning. Physicians, nurses, and administrators can instantly retrieve critical documents, improving care coordination and reducing communication breakdowns.
- Example: A nurse can access a recent imaging report, a physician can view lab results, and an administrator can verify compliance documents—all in real time.
Enhancing Workflow and Compliance
- Reduces delays caused by missing or misfiled documents.
- Ensures audit trails for every upload or edit.
- Supports regulatory adherence through secure, traceable storage.
- Integrates seamlessly with longitudinal patient records, ensuring a comprehensive view of every patient encounter.
By centralizing document management, organizations eliminate fragmented workflows, enhance clinical decision support, and ensure that every file contributes to accurate documentation, timely care, and high-quality outcomes. It’s not just storage—it’s a strategic tool that supports efficiency, compliance, and patient safety.
Data without insight is wasted effort. Modern healthcare organizations generate enormous amounts of patient and operational data daily. Without clinical insights, this information sits idle, leaving providers blind to inefficiencies, care gaps, and performance trends.
Turning Data into Action
Imagine a clinic where lab results, progress notes, and task completion are tracked—but no one sees the bigger picture. Missed follow-ups, inconsistent documentation, and delayed interventions become the norm.
With a robust reporting and insights module, every piece of data is actionable:
- Provider Performance Metrics: Track chart closure rates, documentation accuracy, and task completion. Identify top performers and areas needing support.
- Operational Dashboards: Visualize appointment utilization, lab turnaround times, and workflow bottlenecks in real time.
- Clinical Quality Metrics: Monitor care gaps, compliance adherence, and patient outcomes across departments.
How Insights Improve Care
- Early Identification of Risks: Dashboards highlight abnormal labs, delayed treatments, or missing notes, allowing proactive intervention.
- Optimized Resource Allocation: Administrators can adjust staffing or reassign tasks based on real-time operational trends.
- Data-Driven Decision Support: Providers access trend analysis, aggregated patient histories, and predictive insights to make faster, more accurate decisions.
Real-World Example
A multi-specialty clinic used reporting dashboards to identify that over 15% of imaging orders were delayed due to missing follow-ups. By integrating orders & results management with care coordination, they reduced delays by 60%, improving patient safety and satisfaction.
Best Practices
- Use standardized metrics for provider performance and workflow efficiency.
- Combine clinical dashboards with longitudinal patient records to maintain a comprehensive view.
- Ensure real-time alerts for overdue tasks or care gaps to prevent inconsistent care.
- Integrate insights with AI-powered documentation and tasking for continuous workflow improvement.
Reporting and clinical insights are not optional—they are essential. When teams have real-time visibility, they can act decisively, improve compliance, enhance patient experience, and drive measurable outcomes across every layer of the organization.
9. Compliance & Interoperability
Ensuring regulatory compliance and seamless interoperability is non-negotiable in modern healthcare. Fragmented systems increase risk, create gaps in audit trails, and limit real-time visibility into patient data. Integrating standards like HL7 and FHIR within a secure framework ensures safe, efficient, and traceable workflows.
Key Compliance & Interoperability Features
| Feature | Description | Benefit |
|---|---|---|
| HL7 Integration | Standardized messaging for lab, imaging, and EHR data | Enables consistent data exchange across legacy and modern systems |
| FHIR Support | Fast, API-based data interoperability | Facilitates real-time data sharing and mobile access |
| Audit Trails | Automatic tracking of all data access, edits, and transfers | Supports regulatory compliance and clinical accuracy |
| Role-Based Access | Permissions based on user role | Maintains security and privacy across all clinical documents |
| Secure Data Exchange | Encrypted communication between systems | Protects patient data while allowing cross-system collaboration |
Why Compliance & Interoperability Matters
- Regulatory Adherence: Automatic audit trails and standardized exchanges reduce the risk of non-compliance with HIPAA and other regulations.
- Seamless Data Flow: Integrating HL7 and FHIR ensures labs, imaging centers, and EHRs communicate without manual intervention.
- Enhanced Clinical Decision Support: Real-time access to accurate, comprehensive data improves diagnoses and treatment planning.
- Reduced Operational Risk: Secure, standards-based exchange mitigates errors caused by manual data handling or missing records.
Best Practices
- Map all systems to HL7 and FHIR standards for unified access.
- Ensure all edits and accesses are logged to maintain a secure repository and audit trails.
- Conduct regular compliance checks and report on provider performance metrics tied to documentation accuracy.
- Train staff on interoperability workflows to ensure consistent use and adoption.
Impact on Patient Management
A compliant, interoperable system creates a single source of truth for all patient data. Providers access longitudinal patient records instantly, administrators can verify tasks and results, and patients benefit from safe, coordinated care. Integrating compliance and interoperability directly into daily workflows strengthens efficiency, accountability, and overall care quality.
How Patient Management Impacts Every Role in a Healthcare Organization
National surveys show clinicians spend a substantial share of time on administrative tasks, contributing to U.S. health administrative costs of ~17–25% of total system spending. Modern patient management software touches every corner of a healthcare organization. From providers to executives, streamlined workflows, AI-powered documentation, and unified data access transform daily operations, reduce errors, and improve patient outcomes.
Providers: Faster Documentation, Accurate Records, Fewer Clicks
Physicians and specialists benefit from longitudinal patient records, real-time SOAP notes, and AI medical scribes that minimize manual entry. Key impacts include:
- High-Quality Documentation: Structured templates ensure accuracy in progress notes, diagnoses, and discharge summaries.
- Time Savings: Real-time transcription and AI-generated summaries reduce charting time by up to 50%.
- Decision Support: Immediate access to lab results, imaging, and comprehensive histories enables faster, safer decisions.
Example: A cardiologist reviewing an urgent patient case can see all labs, imaging, and prior encounters in one view, enabling rapid, informed treatment.
Nurses & Clinical Staff: Clean Handoffs, Reduced Manual Entry
Nurses and allied health staff handle tasking, handoffs, and vital tracking daily. With unified access:
- Handoffs are structured, reducing errors and communication breakdowns.
- Task management dashboards prevent missed follow-ups or delayed interventions.
- Real-time updates to encounter tools ensure vitals and patient updates are accurate.
Example: A nurse taking over a shift immediately sees pending tasks, abnormal labs, and treatment updates, ensuring seamless continuity.
Medical Assistants: Streamlined Intake, Tasks, Vitals Capturing
Medical assistants benefit from automated intake forms, device-integrated vitals, and streamlined tasking. Advantages include:
- Reduced manual entry and duplication.
- Accurate population of problem lists, allergies, and medications.
- Faster preparation for provider encounters.
Example: An MA entering patient vitals automatically syncs the data to the patient chart, reducing errors and accelerating provider workflow.
Operations Teams: Workflow Consistency, Throughput Improvements
Administrative and operations staff rely on integrated reporting, order tracking, and compliance dashboards. Benefits include:
- Operational Visibility: Track appointment utilization, lab turnaround, and task completion in real time.
- Improved Throughput: Reduce bottlenecks and missed follow-ups.
- Standardized Workflows: Minimize ad-hoc manual processes.
Example: The front-desk team can immediately identify uncompleted lab orders and assign follow-ups without disrupting clinical teams.
Quality & Compliance Teams: Transparent Audit Trail, Unified Data
Quality and compliance professionals gain:
- Complete audit trails for every note, order, and task.
- Standardized reporting for regulatory adherence.
- Insights into gaps, care inconsistencies, and provider performance.
Example: A compliance officer can generate a report showing delayed discharges or incomplete documentation across multiple locations instantly.
Executive Leadership: Cost Efficiency, Scalability, Predictable Processes
Leadership teams benefit from the analytics, interoperability, and unified platform visibility. Key impacts:
- Predictable workflows reduce staffing stress and costs.
- Performance metrics highlight operational efficiencies and inefficiencies.
- Scalable solutions support enterprise expansion without added complexity.
Example: An executive can evaluate multi-location performance dashboards to make informed decisions on staffing, process improvements, and resource allocation.
Summary
From providers to executives, modern patient management software improves efficiency, reduces errors, strengthens compliance, and enhances patient experience. By embedding AI-powered documentation, care coordination, orders management, and reporting into one platform, healthcare organizations create a system where every role operates efficiently, informed, and aligned around patient-centered care.
Implementing Modern Patient Management at Scale
Rolling out a modern patient management system requires careful planning. Successful implementation combines frameworks, training, change management, and clear metrics to ensure adoption and measurable improvements.
Implementation Framework
Start with a structured approach:
- Requirements Gathering: Identify workflow gaps, documentation needs, and interoperability goals.
- Workflow Mapping: Document current processes for charting, orders, tasks, and handoffs.
- Data Migration: Consolidate longitudinal patient records, attachments, and existing documentation into the new system.
- Integration Planning: Ensure seamless connectivity with EHRs, lab systems, imaging platforms, and AI-powered tools.
Tip: Prioritize high-impact workflows first to demonstrate early wins.
Training & Adoption
Effective training drives adoption:
- Role-Based Paths: Customize sessions for providers, nurses, MAs, operations, and leadership.
- Hands-On Simulations: Practice documentation, tasking, and order workflows in a controlled environment.
- Continuous Support: Provide resources, FAQs, and superusers for ongoing guidance.
Quick win: Providers trained on AI-powered documentation can reduce charting time immediately.
Change Management Strategies for Clinical Teams
Change is hard. Minimize friction with:
- Communication: Clearly explain benefits and workflow improvements.
- Feedback Loops: Collect input during pilot phases to refine processes.
- Champions & Superusers: Identify early adopters who mentor peers.
- Incremental Rollout: Implement modules sequentially—charting first, then tasking, orders, and reporting.
Metrics for Success
Track measurable outcomes to ensure ROI and operational improvements:
- Chart Closure Time: Speed of completing SOAP notes and progress notes.
- Task Completion Rate: Percentage of tasks completed on time.
- Documentation Accuracy: Reduction in errors or missing data.
- Order Turnaround: Time from lab or imaging order to result availability.
- Provider Satisfaction: Survey clinicians on workflow efficiency and usability.
Takeaways
- Plan, map, and migrate workflows before deployment.
- Train every role with hands-on, role-specific sessions.
- Apply structured change management to encourage adoption.
- Track metrics to demonstrate value and optimize workflows.
Implementing a modern patient management platform at scale is not just about technology—it’s about aligning people, processes, and data. When done right, organizations see faster documentation, better care coordination, improved compliance, and measurable improvements in both provider satisfaction and patient outcomes.
How to Evaluate Patient Management Software
Choosing the right patient management software is critical for operational efficiency, clinical accuracy, and patient satisfaction. A structured evaluation ensures the platform aligns with organizational goals, supports workflows, and delivers measurable value.
Key Evaluation Criteria
| Category | What to Look For | Why It Matters |
|---|---|---|
| Workflow Coverage | Support across all 9 pillars: charting, encounter tools, documentation, AI documentation, care coordination, orders & results, document management, reporting & insights, compliance & interoperability | Ensures the platform addresses every operational and clinical need |
| AI Readiness | Real-time transcription, AI medical scribe, summary generation | Reduces administrative burden and improves clinical documentation quality |
| Interoperability | HL7, FHIR support, multi-EHR integration | Enables secure data exchange, unified access, and comprehensive view across systems |
| Clinical Tasking | Role-based tasking, handoffs, treatment workflows | Improves care coordination, reduces communication breakdowns, and prevents missed follow-ups |
| Security & Compliance | Audit trails, role-based access, encrypted data storage | Maintains HIPAA compliance and supports regulatory reporting |
| Data Governance | Structured templates, standardized problem lists, attachment management | Supports clinical accuracy and decision-making across teams |
| Scalability | Multi-location support, configurable workflows, cloud or on-prem options | Allows growth without disrupting workflows or adding complexity |
| Reporting & Insights | Dashboards for provider performance, operational metrics, and quality reporting | Enables real-time visibility and continuous improvement |
| User Experience | Intuitive interface, mobile access, customizable views | Increases adoption, reduces training time, and minimizes errors |
Evaluation Tips
- Prioritize Integration: Confirm the platform works seamlessly with existing EHRs, lab systems, and imaging tools.
- Test AI Capabilities: Evaluate AI-powered documentation in live scenarios for accuracy and efficiency.
- Check Customization: Ensure templates, tasks, and reporting dashboards can be tailored to your workflows.
- Measure ROI: Track improvements in task completion, documentation accuracy, and provider satisfaction.
Subtle Benchmarking
While evaluating, compare each feature against a high-performing, unified platform benchmark. Look for solutions that combine AI documentation, care coordination, secure interoperability, and real-time insights without adding workflow complexity.
Selecting the right patient management software transforms clinical workflows, reduces errors, enhances care coordination, and improves patient experience. A structured, criteria-driven evaluation ensures your organization invests in a platform that delivers both operational efficiency and clinical excellence.
The CERTIFY Health Difference: Unified, Intelligent, Proven
Healthcare organizations are moving toward platforms that unify clinical workflows, enhance efficiency, and drive measurable outcomes. Certify Health embodies this modern approach, providing a single, integrated solution across patient charting, documentation, care coordination, orders, and compliance.
Unified Platform Across Workflows
Certify Health eliminates the friction caused by fragmented systems:
- Patient Charting: Complete longitudinal patient records with real-time visibility.
- Clinical Documentation: Structured SOAP notes, progress notes, discharge summaries, and AI-powered documentation reduce administrative burden.
- Care Coordination: Tasking, handoffs, and treatment plans ensure nothing falls through the cracks.
- Orders & Results: Lab and imaging orders are tracked end-to-end, linked to encounters for immediate access.
- Compliance & Interoperability: HL7 and FHIR integration with secure audit trails ensures regulatory adherence.
Key Insight: Unified access across these pillars improves provider satisfaction, patient experience, and operational efficiency.
Intelligent, AI-Enabled Efficiency
AI is embedded at every stage of documentation and workflow:
- Real-Time Transcription: Convert patient conversations into structured notes instantly.
- Summary Generation: Automatically produce encounter summaries and discharge documentation.
- Clinical Insights: AI highlights care gaps, abnormal results, and task delays for immediate action.
This intelligence accelerates documentation closure, improves clinical accuracy, and supports decision-making across the care team.
Proven Performance
| Area | Demonstrated Benefit |
|---|---|
| Documentation | Reduces charting time up to 50%, ensures coding accuracy |
| Care Coordination | Streamlines task completion and handoffs, reduces missed follow-ups |
| Orders & Results | Ensures timely lab and imaging tracking, eliminates delays |
| Compliance & Interoperability | Provides traceable audit trails and seamless HL7/FHIR integration |
| Reporting & Insights | Real-time dashboards for provider performance and operational efficiency |
Why Organizations Choose Certify Health
- Scalable: Handles multi-location deployments without adding complexity.
- User-Friendly: Intuitive interface minimizes training and maximizes adoption.
- Data-Driven: Embedded analytics support continuous quality improvement.
- Patient-Centric: Faster workflows, coordinated care, and reduced delays improve the patient experience.
In essence, Certify Health combines unification, intelligence, and proven outcomes to create a patient management platform that doesn’t just digitize workflows—it transforms them. Providers work smarter, operations run smoother, and patients receive safer, more coordinated care.
Patient Management Software FAQs
Does this replace my EHR or augment it?
Patient management software is designed to augment your existing EHR, not replace it. It centralizes workflows like charting, documentation, tasking, and care coordination while integrating seamlessly with HL7/FHIR-enabled EHRs to provide a comprehensive view of patient data.
How does AI documentation maintain accuracy?
AI-powered documentation uses structured templates, real-time transcription, and clinical context from longitudinal patient records. Providers review and confirm AI-generated SOAP notes, progress notes, and discharge summaries, ensuring high clinical accuracy while reducing administrative burden.
What about privacy and regulatory compliance?
Modern platforms provide secure repositories, role-based access, and full audit trails. HL7 and FHIR integration ensures compliant data exchange, and all documentation meets HIPAA and other regulatory requirements.
How long does implementation take?
Implementation depends on workflow complexity, system integration, and training. Typically, a phased rollout with pilot departments ensures smooth adoption. Early wins in AI documentation, orders management, and care coordination accelerate overall deployment.
Can this support multi-location or enterprise environments?
Yes. Scalable architecture allows multi-location support, consistent workflows, and centralized analytics. Providers and staff across locations access the same longitudinal patient records, ensuring coordinated care.
What specialties is it optimized for?
The platform supports multi-specialty environments, including primary care, cardiology, dermatology, OB/GYN, radiology, and more. Flexible templates, encounter tools, and AI-assisted documentation adapt to specialty-specific workflows.
How is data exchanged with external systems?
Using HL7 and FHIR standards, patient data, lab orders, imaging results, and documentation flow securely between EHRs, lab systems, imaging centers, and other external systems. Audit trails track every interaction to maintain compliance and security.
How does this improve care coordination?
Integrated tasking, handoffs, and treatment plan workflows ensure nothing falls through the cracks. Alerts, role-based assignments, and linked documentation maintain real-time visibility, reducing communication breakdowns and supporting patient-centered care.
How does it support operational insights?
Real-time dashboards provide provider performance metrics, order tracking, and workflow analytics. Executives and administrators can optimize staffing, reduce bottlenecks, and track KPIs for continuous improvement.
What is the patient experience impact?
Streamlined workflows, faster documentation, and accurate, coordinated care reduce wait times, minimize repeated questioning, and increase patient satisfaction, creating safer and more reliable care journeys.
Transform How Your Organization Manages Clinical Workflows
It’s time to streamline documentation, eliminate workflow friction, and deliver higher-quality, coordinated care. Modern healthcare demands platforms that unify patient charting, AI-powered documentation, care coordination, orders management, and compliance in one intelligent system.
Why Upgrade Your Workflow Today
- Faster Documentation: Complete SOAP notes, progress notes, and discharge summaries in less time.
- Improved Care Coordination: Tasks, handoffs, and treatment plans are tracked in real time.
- Accurate, Unified Records: Access longitudinal patient records with real-time visibility.
- Enhanced Compliance: Full audit trails and HL7/FHIR interoperability reduce regulatory risk.
- Actionable Insights: Dashboards and analytics improve operations and provider performance.
Take Action Now
- Request a Live Demo: See how streamlined workflows can transform your practice.
- Get Pricing: Understand ROI and efficiency improvements before committing.
- Download the Buyer’s Guide: Learn the 9 pillars of modern patient management in detail.
- Talk to a Clinical Workflow Expert: Get customized recommendations tailored to your organization.
Strong positioning: With a unified platform, your team works smarter, patients experience coordinated care, and compliance and reporting become effortless.
Don’t let fragmented workflows slow your organization. Upgrade to a modern patient management system that reduces manual work, eliminates errors, and supports faster, safer care delivery. The right platform transforms every role, every workflow, and every patient encounter.