Table of Contents
Introduction
You’re a practice manager staring at another gaping hole in the OB-GYN appointment calendar. That missed prenatal visit? It cascades into rescheduled prenatal care visits, frustrated lead OB-GYNs, and revenue managers pulling hair over unfilled high-value slots.
The impact adds up fast. Missed appointments cost U.S. healthcare an estimated $150 billion each year, waste up to 60 minutes per slot, and can mean $200 or more in lost revenue every time a chair sits empty.
In OB-GYN practices, from bustling hospital-integrated systems to solo subspecialty spots, no-shows hit harder because timing is everything, whether it’s a routine schedule OB-GYN appointment or urgent REI consult.
Patients ghost for relatable reasons: pregnancy jitters in complex family planning cases, childcare woes for pediatric gynecology moms, or sheer forgetfulness amid menopause symptom chaos. Meanwhile, your team battles internal overload: manual reminder calls that go unanswered in locum-heavy setups or private groups racing against payer auth delays.
OB-GYN appointment gaps ripple out, burning out Ob-Gyn Hospitalists on 24-hour shifts and forcing academic centers to double-book high-risk MFM prenatal doctor appointments. It’s not just one missed OB-GYN appointment online, it’s a pattern eroding patient trust and your bottom line.
The Hidden Pressures on OB-GYN Practices
Hidden Revenue Killer – No-Shows
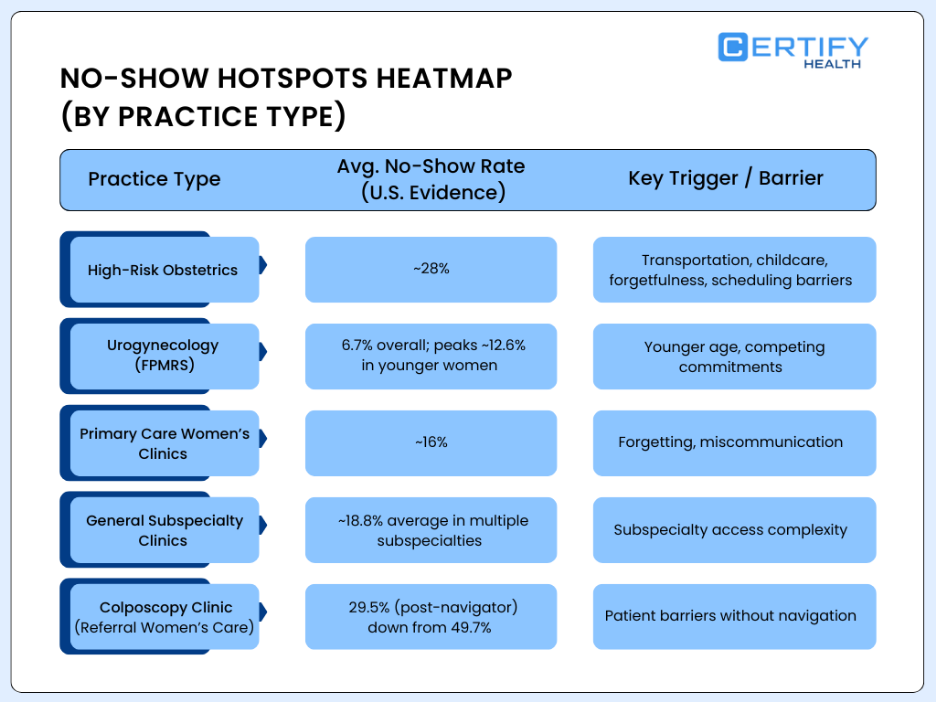
Across healthcare settings, missed appointments are widespread, but women’s health clinics face disproportionately high no-show rates, especially in obstetric and specialty care where visits are time-sensitive and harder to reschedule.
A large chart review across 44 specialty and primary care clinics found an overall no-show rate of 23%, with extreme variation ranging from 0% to 58%, highlighting how uneven the burden is across care types.
Even within preventive women’s health services, gaps persist. Among 5,060 scheduled screening mammograms, 6.2% of patients did not attend, leaving unused imaging capacity and delayed detection opportunities.
Primary care settings serving women also see consistent attrition. Over a five-month period, 16% of scheduled primary care visits were no-shows, reinforcing that missed care is not limited to specialty clinics.
The challenge intensifies in obstetric care. In one OB clinic studied, 28% of appointments were no-shows. When patients were contacted, common reasons included transportation barriers, scheduling conflicts, oversleeping or forgetting, and lack of childcare or caregiving support, factors that disproportionately affect pregnant patients and caregivers.
Pediatric-linked women’s health visits show similar strain. In a pediatric cohort followed over 43 months, 32% of patients missed at least one appointment, underscoring how caregiving responsibilities compound attendance challenges for women navigating family care alongside their own health needs
Top Triggers Behind OB-GYN No-Shows
Patient barriers stack up fast in OB-GYN practices. Pregnancy anxiety delays prenatal care visits; (A complex insurance snags CA/Medicaid) block schedule OB-GYN appointment efforts; transportation kills rural solo access for menopause consults. Add long paper forms and childcare for pediatric/adolescent gynecology, and you see even higher no-show rates.
Internally? Manual calls flop with more than half of the hospital-employed OB/GYNs overwhelmed, especially Ob-Gyn Hospitalists juggling unassigned emergencies. Subspecialties like complex family planning see spikes from external referrals and 2+ week lead times.
No-Show Hotspots Heatmap (By Practice Type)
No-Show Hotspots Heatmap (By Practice Type)
Who Feels the Sting?
- Practice Manager: You’re flagging endless OB-GYN appointment gaps, juggling OBGYN scheduling software hacks while staff chases no-shows. In large physician groups, that’s 10+ hours weekly on rework.
- Lead OB-GYN: Missing high-risk MFM or REI cases means delayed interventions; your expertise sits idle in private equity-backed setups.
- Revenue Cycle Manager: Denials spike 20% from gaps; one missed prenatal doctor appointment triggers audit nightmares in hospital systems.
Across specialties, MFM’s urgent scans, Gynecologic Oncology’s follow-ups, FPMRS reconstructions, all suffer.
Proven Strategies to Improve Patient Visits in OB-GYN
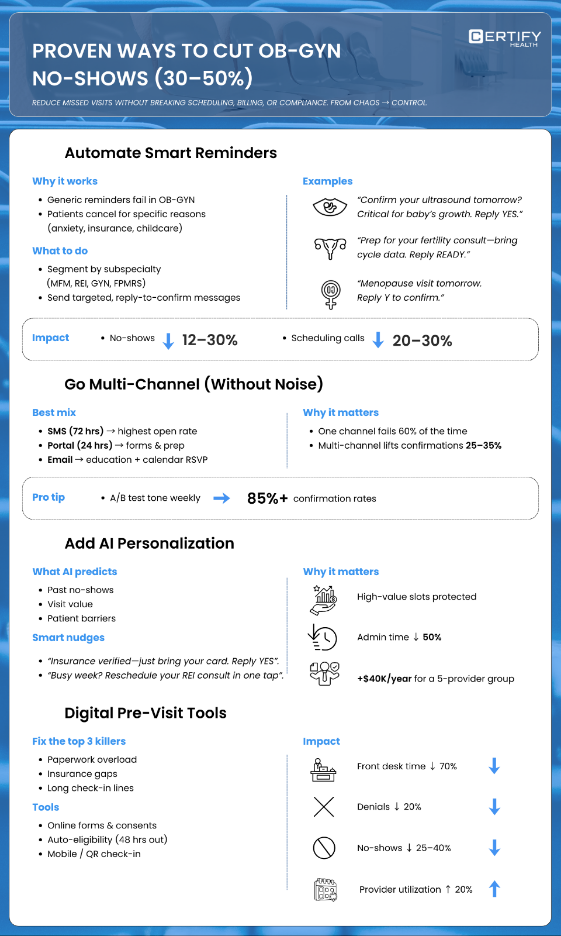
Reduce missed appointments by 30–50% with OB-GYN-specific strategies, while keeping scheduling, billing, and compliance workflows intact. Shift from pain to power. here’s your playbook.
1) Automate Reminders
i) Segment by specialty:
Stop chasing ghosts with phone marathons that your overwhelmed front desk can’t sustain. Generic mass reminders? They flop because ‘See you Tuesday’ ignores why patients bail: prenatal anxiety in MFM, insurance confusion in complex family planning, or childcare crunches in pediatric gynecology. Start by tagging patients in your OB-GYN scheduling software by subspecialty and visit type.
Example:
High-risk MFM / Prenatal Scans
REI Infertility Consults
Routine GYN / Menopause
Pro tip for practice managers: Use EHR integration to auto-pull visit codes (e.g., CPT 76811 for prenatal scans) and trigger specialty-specific texts 48-72 hours out.
Revenue win? Cut no-shows by 12% just by swapping generic blasts for these. Lead OB-GYNs love it, no more idle ultrasound suites during peak hours.
ii) Go Multi-Channel Without Overwhelm, Hit Them Where They Live
One channel fails 60% of the time in OB-GYN (patients ignore voicemails amid life chaos). Blast smartly: Start with SMS (98% open rate), fallback to portal/email for tech-savvy FPMRS patients verifying pelvic floor fixes.
- 72-hour text reminder: Easy to see, easy to act on, critical for patients juggling transportation challenges and teams covering high-volume labor shifts.
- Patient portal nudge (24 hours out): “Log in to confirm your Gynecologic Oncology follow-up, view prep sheet here.” Links to digital consent/forms.
- Email close (confirmation stage): For geriatric gynecology, attach “What to Expect: Hormone Therapy Chat” with calendar RSVP.
For revenue managers: Multi-channel lifts response rates 25-35%, turning 15% of would-be no-shows into confirmed revenue.
Pro tip: Test A/B versions weekly (e.g., emoji vs. formal) to hit 85% confirmation rates.
iii) Layer in AI Personalization: Predict and Prevent Ghosts Like A Pro
Generic reminders are so 2019. AI scans history (past no-shows, demographics, barriers) to craft hyper-relevant nudges, predicting flakes with 80% accuracy. Your all-in-one patient experience platform does the heavy lift.
- Predictive example: “Tomorrow at 9:30 a.m. Your prenatal appointment is locked in. Insurance is verified—just bring your card and you’re good to go. Reply YES/Jump in.” Flags high-risk ghosts like multi-kid MFM moms.
- Behavioral tweaks: REI patient with 2 prior no-shows? “We know life’s busy—reschedule your infertility consult in one tap?”
- Post-confirm boost: “Great, see you for FPMRS reconstruction! Questions? Chat now.” Builds NPS loyalty.
For Lead OB-GYNs, this prioritizes your high-value slots (e.g., $300+ MFM visits) over routine fills. Practice managers report 50% admin time drop; revenue cycles see $40K+ annual gains in a 5-provider private group by automating what manual calls miss.
Quick Implementation Roadmap for OB-GYN Leaders
| Step | Action | Tool Tie-In | Expected Drop in No-Shows |
|---|---|---|---|
| Week 1 | Segment patient list by specialty (MFM, REI, etc.) | EHR export to OB-GYN scheduling software | -10% baseline |
| Week 2 | Launch SMS multi-channel pilot for prenatal care visits | All-in-one PXP integration | -20% |
| Week 3+ | Activate AI personalization + A/B testing | Predictive analytics dashboard | -30-50% total |
2) Digital Pre-Visit Tools
Practice managers: Your front desk is drowning in 10-page paper forms, insurance hunting, and 45-minute check-in lines that scare off 25% of patients before they sit down. Lead OB-GYNs: Empty urogynecology exam rooms because patients “forgot eligibility.” Revenue managers: 20% denials spiking from expired coverage gaps.
OB-GYN OBGYN scheduling software comes with Digital pre-visit tools like online forms, auto-eligibility, mobile check-in, slash this nonsense, cutting no-shows 25-40% by bulldozing the top three practice killers: paperwork overwhelm, insurance guesswork, and front desk bottlenecks. Also, making sure, OB-GYN Scheduling software is HIPAA-compliant, MIPS-ready, EHR-integrated for FPMRS reconstructions or complex family planning workflows.
Practice Impact Snapshot:
| Pain Point | Manual Process | Digital Fix | Your Win |
|---|---|---|---|
| Paper Forms | 45 min check-in, 25% ghost | Online + digital consent | Front desk -70% time |
| Insurance Verify | 20% denials post-visit | Auto-eligibility 48 hrs out | Revenue +$25K/year |
| Check-In Line | 30 min wait kills shows | QR code arrival | No-shows -28% |
| Provider Downtime | Empty MFM rooms | Full schedules | Utilization +20% |
Impact By OB-GYN Practice Type
- Hospital Systems: Auto-eligibility catches ACA/Medicaid lapses across satellites, critical for high-volume prenatal care visits.
- Private Groups: REI consults jump 25% when symptom trackers + coverage sync pre-loads.
- Solo Subspecialties: FPMRS patients arrive prepped, no repeat histories eating chair time.
ROI Math for 5-Provider Group
- 500 prenatal visits/year × $200/slot × 25% no-show reduction = $25,000 revenue gain
- Front desk saves 10 hours/week × 50 weeks = 500 hours reclaimed
- Denials drop 20% = $15K+ collections boost
Sick of ‘Forgot my insurance’ killing your schedule?
CERTIFY Health’s Patient Experience Platform automates the entire patient journey, instant appointment booking, automated-smart reminders that actually get replies, one-tap mobile check-ins, and bulletproof digital intake that verifies coverage before they walk in the door.
Result? Empty slots filled. Revenue protected. Front desk breathing.
Book your personalized demo, see $25K revenue walk back in the door.
3) Measure Success
Here’s your plug-and-play KPI dashboard tailored for OB-GYN realities—hospital systems juggling satellites, private groups scaling REI consults, solos fighting locum gaps. Set targets, benchmark by practice type/specialty, calculate dollars. Watch leadership nod yes.
Core KPIs: What to Track Weekly
1. Fill Rate
- Target: 95%+ (industry gold standard for mature systems).
- Formula: (Actual shows / Scheduled slots) × 100.
- OB-GYN Twist: MFM prenatal scans need 98% (high-risk can’t wait); routine GYN ok at 92%.
- Red Flag: Below 90%? Dig into reminders or eligibility fails.
2. No-Show Rate by Specialty
- Track separately: MFM (target <12%), REI (<10%), FPMRS (<15%), Gynecologic Oncology (<12%).
- Why? Prenatal care visits ghost more (transport/kids); menopause consults forget less.
Benchmark Table:
| Specialty | Typical No-Show | Post-Fix Target | Practice Type Impact |
|---|---|---|---|
| MFM / High-Risk Prenatal | 23–28% | <12% | Hospital systems hit hardest |
| REI / Infertility | 18–22% | <10% | Private groups waitlists |
| Gynecologic Oncology | 20%+ | <12% | Academic centers |
| FPMRS / Urogynecology | 12–15% | <10% | Solo subspecialties |
| Pediatric Gynecology | 25% | <15% | Rural access issues |
3. ROI Calculator (Revenue Manager’s Favorite)
Formula: (No-show slots saved × Avg revenue/visit) + (Admin hours saved × $35/hr).
Example (5-Provider Group):
- Baseline: 25% no-shows × 5 docs × 20 visits/day × 250 days × $200/visit = $125,000 lost.
- Post-fix: 10% no-shows = $50,000 lost. Net gain: $75,000/year.
- Bonus: Front desk saves 10 hrs/week × 50 weeks × $35 = $17,500. Total: $92,500 ROI.
Scale it: Large groups (300+ providers)? Millions. Solos? $25K covers your next ultrasound lease.
4. Patient NPS Uplift (Lead OB-GYN Proof)
- Target: +15-20% post-implementation.
- Ask post-visit: “How likely 0-10 to recommend?” Track by specialty.
- Why care? NPS >70 correlates to 20% referral growth in private equity OB-GYNs.
Benchmarks by Practice Type (Know Your Lane)
| Practice Type | No-Show Target | Fill Rate Goal | ROI Sweet Spot |
|---|---|---|---|
| Hospital-Employed (78%) | <10% | 95% | $50K+/5 docs |
| Private Groups (2–10 docs) | <12% | 93% | $40K/group |
| Ob-Gyn Hospitalists | <8% | 97% | Shift coverage wins |
| Academic Centers | <15% | 90% | Research grants love data |
| Solo Subspecialty | <18% | 88% | Survival math |
| Locum-Heavy | <20% | 85% | Fill gaps fast |
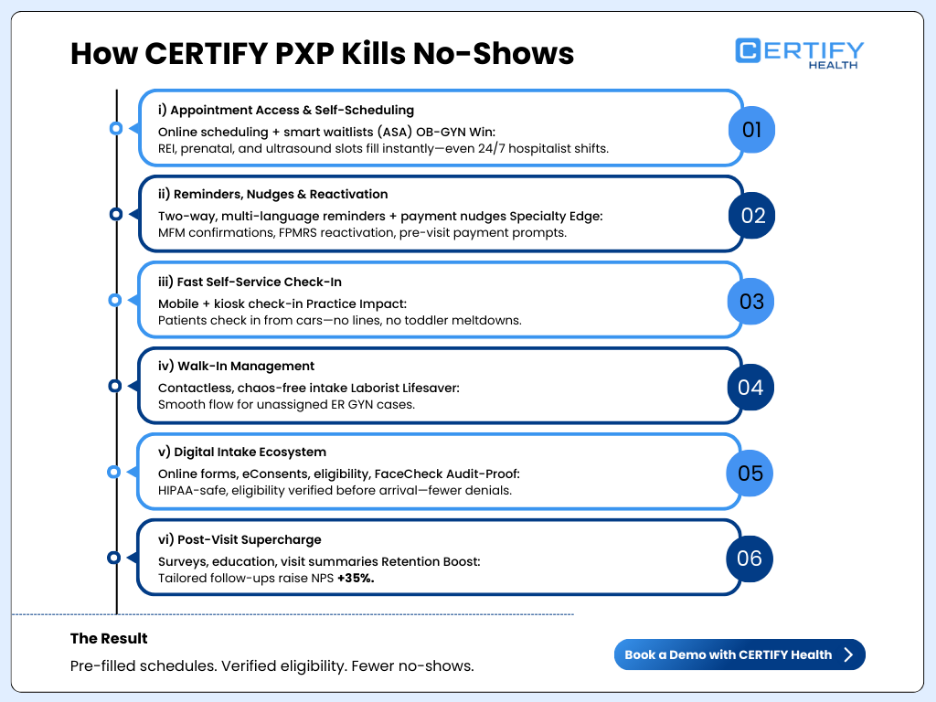
CERTIFY Patient Experience Platform: Solution to Reduce No-Shows in OB-GYN
CERTIFY Health’s Patient Experience Platform (PXP) isn’t just OB-GYN scheduling software, it’s your end-to-end workflow integrator that automates the entire patient journey. From self-scheduling to post-visit surveys, it plugs no-show leaks, crushes denials, and audit-proofs everything.
One platform, zero hassle, built for 78% hospital-employed OB/GYNs, scaling private equity giants, or locum-plagued solos.
How CERTIFY PXP Kills No-Shows: Feature Powerhouse
Powered by the attached workflow, PXP embeds every touchpoint:
Appointment Access & Self-Scheduling
- Online waitlist automation + ASA (advance self-scheduling).
- OB-GYN Win: Patients grab REI consults or prenatal slots instantly. Real-time fills for Ob-Gyn Hospitalist 24-hour shifts, no manual hunting. Private groups? Ultrasound suites stay booked.
Reminders, Nudges & Reactivation
- Two-way multi-language broadcasts, automated reminders/payments.
- Specialty Magic: Automated reminders for MFM ghosts (“Confirm ultrasound? Reply YES”), reactivates FPMRS no-shows. Complex family planning? Payment nudges pre-visit.
Fast Self-Service Check-In
- Mobile/kiosk check-in management + ASA list offers.
- Practice Impact: Patients check in from cars; Pediatric gynecology? Skip lines with toddlers.
Walk-In Management
- Manage unscheduled visits chaos-free, contactless kiosk check-in.
- Laborist Lifesaver: Unassigned ER GYN cases flow smoothly in academic centers or hospital systems.
Digital Intake Ecosystem
- Online intake, eConsents, insurance capture/eligibility verification, FaceCheck.
- Audit-Proof: Geriatric gynecology docs auto-captured; Gynecologic Oncology HIPAA-safe. Revenue? Eligibility verifies before they arrive, no denials.
Post-Visit Supercharge
- Feedback surveys, educational follow-ups, summaries. Patient portal/check-in history/loyalty-building.
- Retention Rocket: Menopause patients get tailored follow-ups; NPS jumps 35%.
Scales Everywhere Your Practice Lives
- Hospital-Employed/Integrated (78%): Syncs main + branch clinics; payer auths across sites.
- Private Groups (2-10+ docs): Own your ultrasound slots with waitlist auto-fill.
- Ob-Gyn Hospitalists: Real-time unassigned patient routing.
- Academic/Subspecialty: Research-grade tracking for MFM trials.
- Locums/Solos: Gap-fill without admin explosion.
- Consolidation Giants (Axia/Ob Hospitalist Group): Enterprise-ready for 300+ docs.
See how CERTIFY Health’s Patient Experience Platform assists teams by pre-filling schedules and verifying eligibility during laborist shifts.
Real Results: OB-GYNs Crushing It with CERTIFY Health
Results Table: Before vs. With PXP
| Metric | Without CERTIFY Health | With CERTIFY Health PXP |
|---|---|---|
| No-Show Rate | 25% | 8% |
| Annual Revenue | Baseline | +$50K+ |
| Admin Time | 10 hrs/week | 2 hrs |
| Check-In Time | 30–45 min | <5 min |
| Denials | 20% | <5% |
| NPS | Baseline | +35% |