Table of Contents
Why Improving Patient Experience Will Define Healthcare Leadership
Patient expectations have changed. Hospitals haven’t kept up.
That gap is now both the biggest threat and the biggest opportunity for healthcare organizations.
Patients expect speed, convenience, transparency, and digital workflows.
They don’t compare you to other clinics; they compare you to Uber, Amazon, and digital banking. If your experience feels slow, manual, or confusing, they switch…quietly and permanently.
In 2024, one in five patients left their provider, and patient experience was the reason nearly 9 out of 10 times. The shift accelerated through 2025 and is expected to increase again in 2026.
Patient experience has become a business-critical function. Not a soft metric. Not a vanity score.
Clinics that modernize Patient experience win on:
- Retention (patients come back)
- Operational efficiency (staff stop drowning in manual work)
- Revenue (fewer no-shows, faster payments, higher completion rates)
- Quality of care (patients follow instructions when communication is clear)
In the next decade, improving patient experience is the fastest path to growth, loyalty, and clinic stability.
The Difference Between Patient Experience, Satisfaction, and Engagement
Most clinics confuse Patient experience, satisfaction, and engagement.
They’re not the same.
Use this quick comparison to get everyone on your team aligned on the fundamentals: what you measure, how you measure it, and what drives patient loyalty and outcomes.
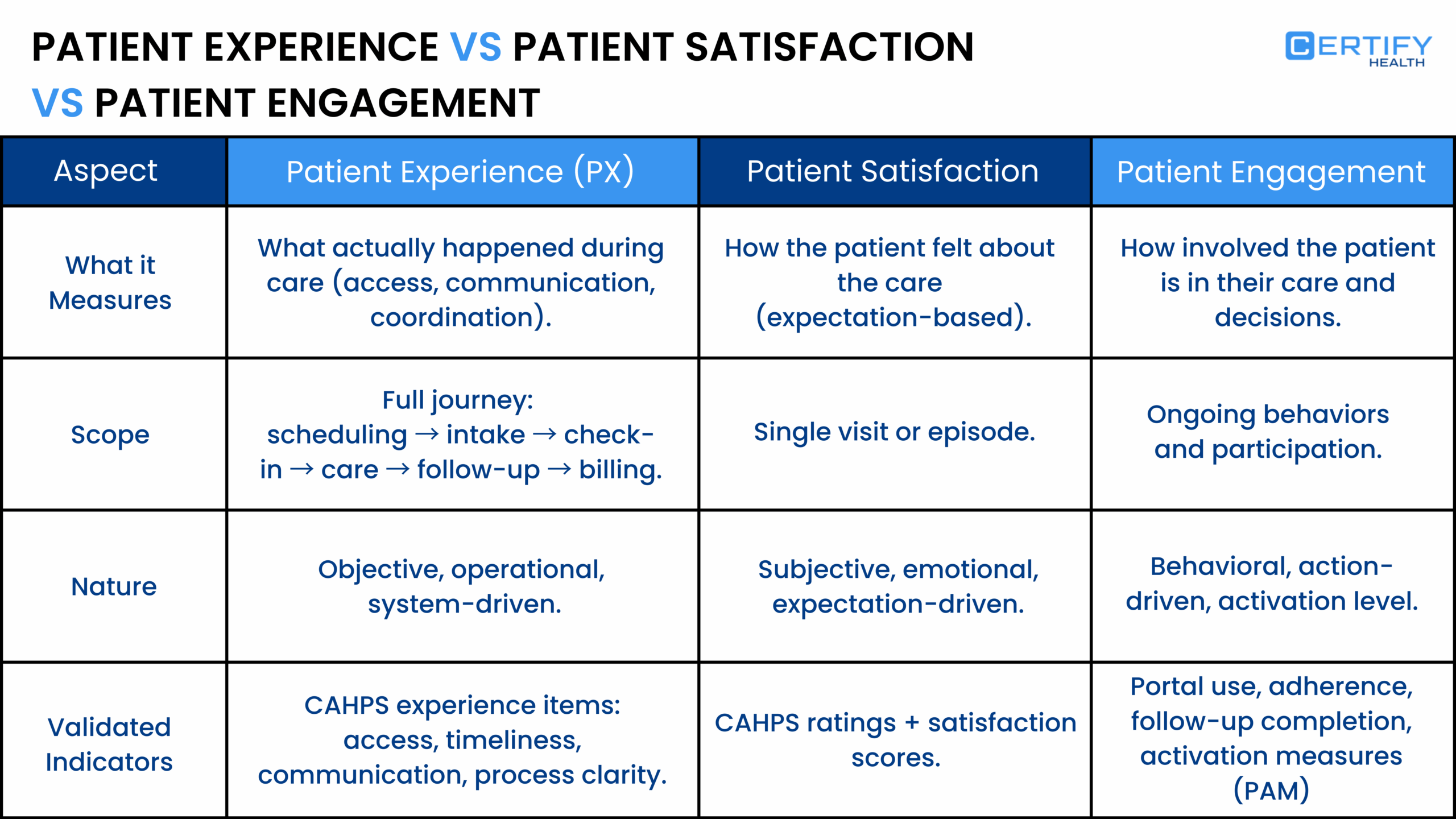
If you’re treating these three terms interchangeably, you’re leaving revenue, efficiency, and trust on the table.
Experience shapes perception. Satisfaction reflects it. Engagement sustains it.
Want to see how leading systems streamline all three with one platform?
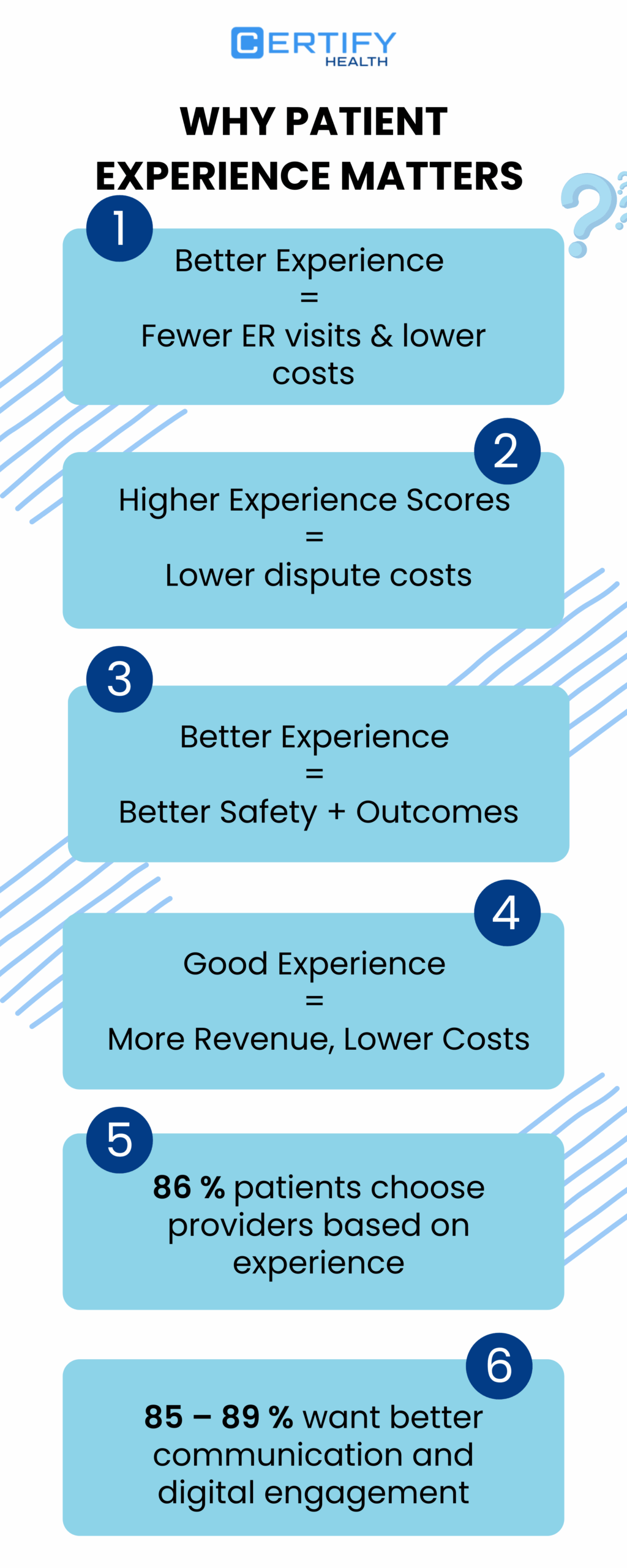
How Does Improving Patient Experience Impact Key Business Outcomes
Improving patient experience paves way for a smarter, more profitable clinic.
When patients move through your system without friction, everything improves: loyalty rises, referrals grow, financial performance stabilizes, and care quality lifts.
Here’s what the data-backed wins look like:
Patient Retention
- Patients stay with clinics that respect their time.
- Every minute saved reduces churn and switching risk.
Referrals
- A seamless, modern experience outperforms paid marketing.
- Satisfied patients refer friends and family organically.
Revenue
A study shows what happens when providers automate even one core workflow: claims management.
- 7% increase in cash flow
- 16% reduction in A/R days (faster payments, stronger liquidity)
The takeaway is blunt: Digitization doesn’t just cut admin friction. It puts real dollars back into the organization.
Digitized workflows directly increase financial performance:
- Fewer no-shows
- Faster patient payments
- Cleaner claims submission
- Higher visit completion rates
- Improved provider throughput
Quality of Care
- Clearer instructions → better adherence
- Timely follow-ups → stronger outcomes
- Reduced confusion → higher satisfaction & CAHPS performance
What is CAHPS Performance?
CAHPS: Measuring Patient Experience with Precision
CAHPS (Consumer Assessment of Healthcare Providers and Systems) is the industry-standard survey program used to measure patient experience across hospitals, clinics, and health plans.
- Captures what patients feel and report about access, communication, and care quality
- Standardized scoring allows benchmarking across providers and regions
- High CAHPS scores = better patient satisfaction, loyalty, and often higher reimbursements
CAHPS performance turns patient experience into actionable, comparable metrics that drive retention, reputation, and revenue.
It is safe to conclude that patient experience systems are a profit lever, a growth engine, and a quality multiplier. Clinics with strong PX consistently outperform those without.
Why Do Most Clinics Struggle with Improving Patient Experience? Evidence-Backed Insights
1. Fragmented patient touchpoints
Care feels disjointed because patients bounce between systems, clinics, and hospitals.
A large multi-hospital analysis found 10% of all emergency visits and 9.1% of admissions were from patients who had recently been seen at a different hospital, highlighting how fragmented the care journey has become.
2. Manual intake creates bottlenecks
Paper intake isn’t just outdated; it injects 20–30 minutes of avoidable delay into every visit.
A controlled comparison found:
- 15 to 20 minutes to complete paper forms
- 5 to 10 minutes to complete digital intake
- Staff time drops from 10 to 15 minutes (paper) to 0 to 2 minutes (digital)
Across a clinic day, backlog compounds into long queues, delayed rooms, and rushed providers.
3. No real-time communication and rising digital expectations
National data shows patients now expect digital access and use multiple portals by default.
The 2024 HINTS survey found:
- Nearly two-thirds of Americans were offered and accessed their patient portal
- 59% had multiple online medical records or portals
This means phone trees and voicemail workflows feel wildly misaligned with actual patient behavior.
4. Unknown wait times drag down experience
Wait-time uncertainty is one of the fastest ways to erode the patient experience.
A 2025 ED satisfaction study found:
- 51.1% waited 31–60 minutes
- 25.4% waited more than 60 minutes
Longer waits correlated with lower satisfaction and weaker return likelihood.
Outpatient data echoes the same issue:
The average wait-time satisfaction score was 6.82/10, showing that wait times remain one of the lowest-rated parts of care.
5. Weak post-visit follow-up
Follow-up breakdowns are a silent killer of outcomes and experience.
A 2025 compliance study found:
- 67.9% of patients follow post-operative instructions
- Only 66% attend scheduled follow-up visits
- Forgetfulness was the top reason for missed follow-ups
This isn’t a patient problem; it’s a communication systems problem.
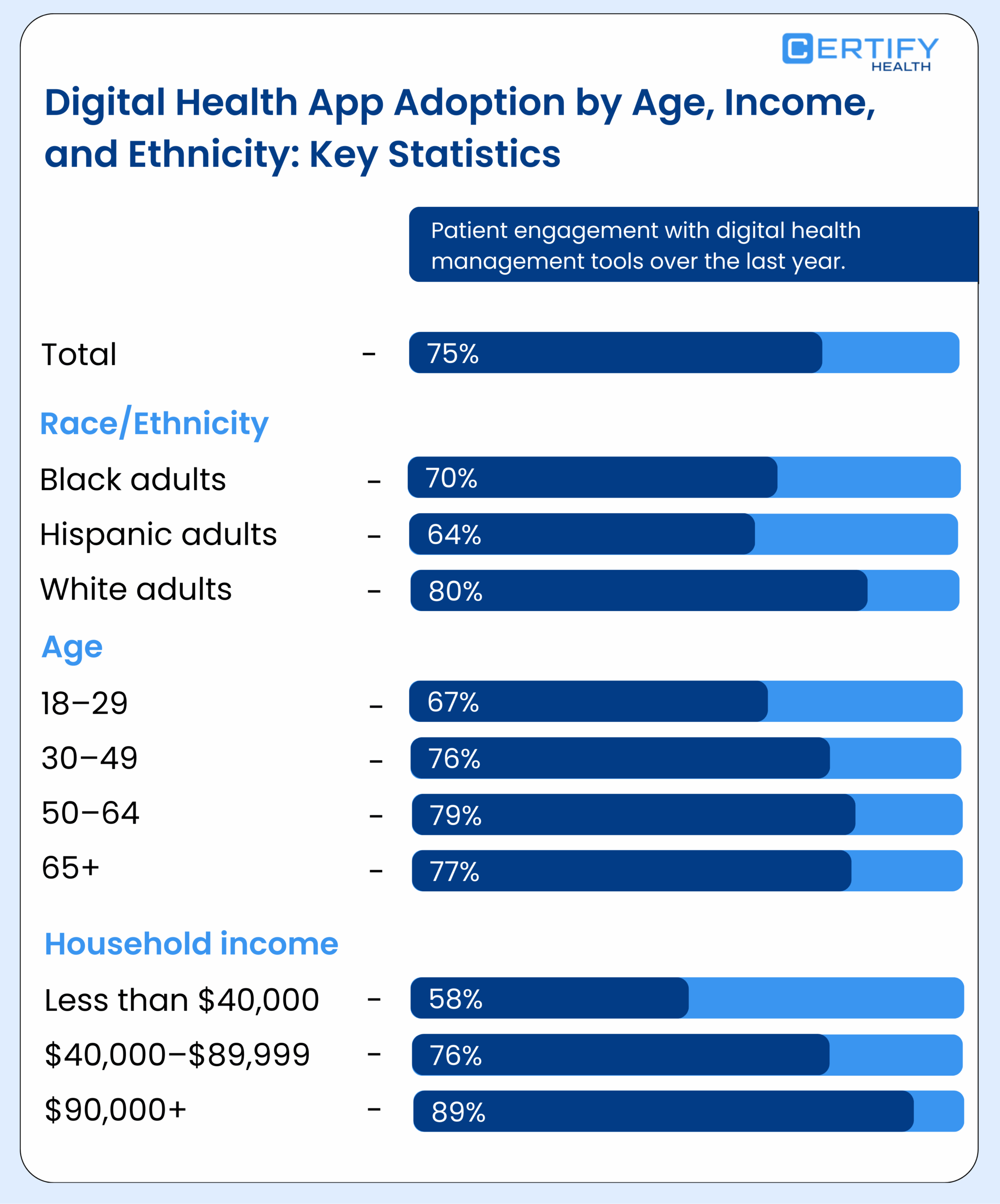
6. Limited digital adoption despite surging demand
Even though most patients now expect digital-first healthcare, national data shows adoption is still shallow and fragmented.
According to 2024 HINTS data:
- Nearly two-thirds accessed their online record
- 59% had multiple portals
- <10% used an app to integrate their records
This means clinics deliver a “digital experience” that is scattered across portals and apps…not unified.
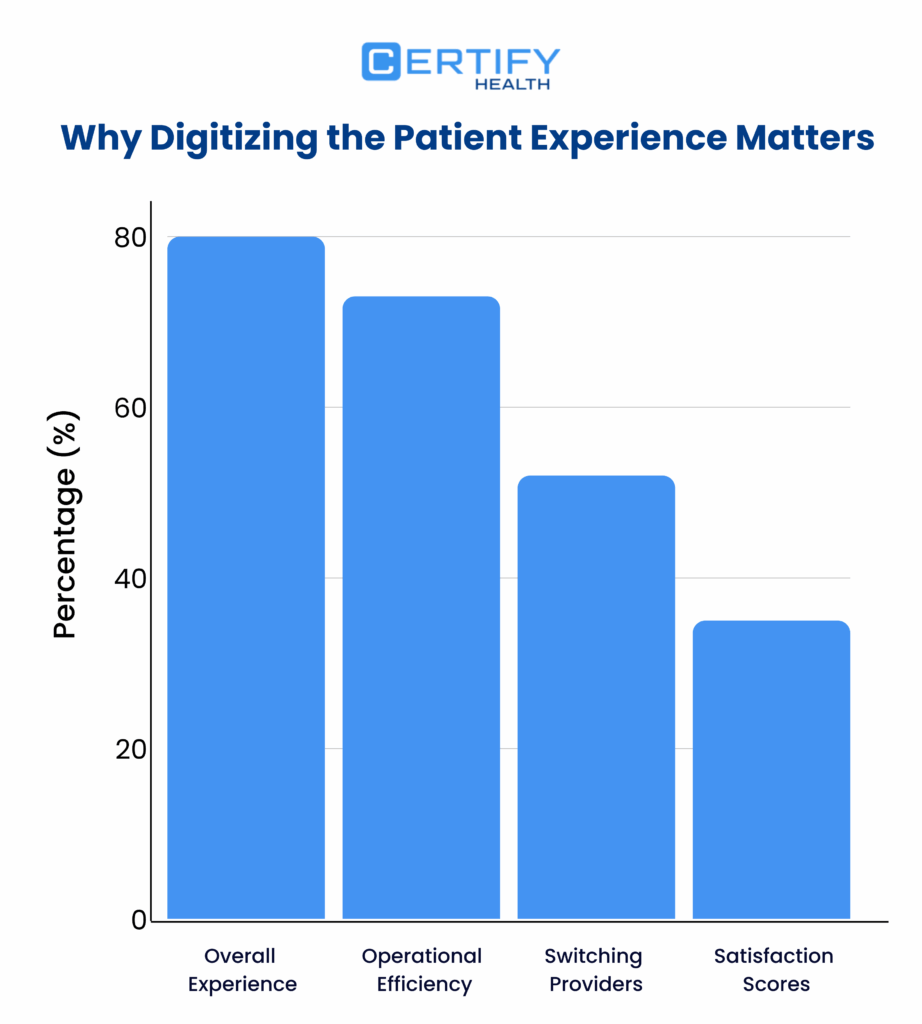
How to Improve Patient Experience: The CERTIFY Health Evidence-Based PX Model
A modern patient experience depends on one thing: a unified workflow.
Clinics lose consistency when scheduling, intake, messaging, and follow-up live in separate systems.
The CERTIFY Health Patient Experience Platform consolidates every touchpoint into one evidence-based, measurable model that upgrades speed, clarity, and trust across the patient journey.
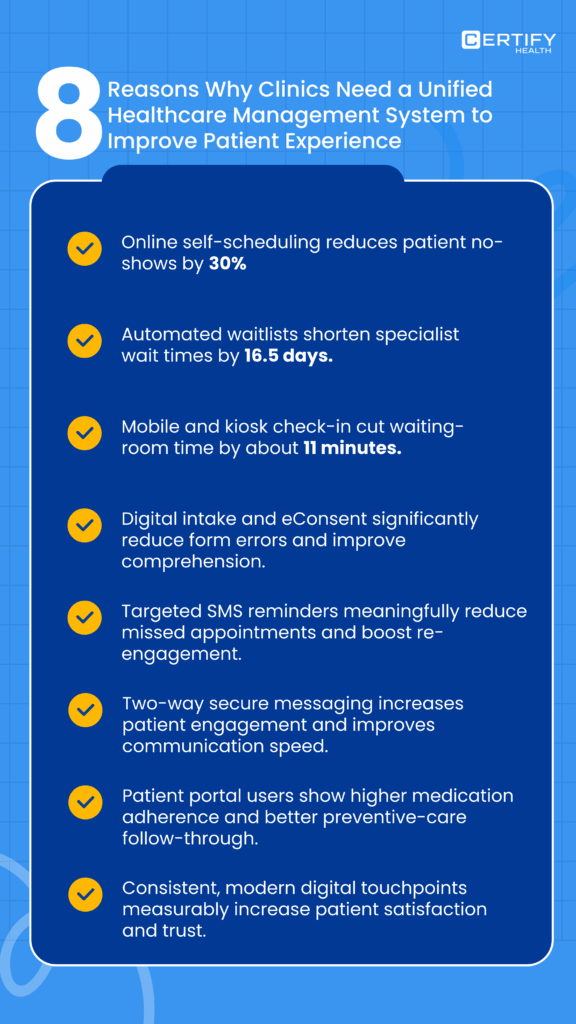
Access and Convenience in Patient Scheduling and Check-In
Patients judge a clinic before they ever walk in. Faster access reduces churn and boosts first-visit completion rates.
Recent federal research shows that over 70% of patients prefer digital-first scheduling and expect real-time updates.
How to Elevate Patient Experience Through Smarter Scheduling and Check-In
- Offer online self-scheduling so patients book without phone delays
- Add ASAP waitlist automation to fill cancelled spots instantly
- Provide walk-in queue transparency to lower perceived wait anxiety
- Enable mobile and kiosk check-in to reduce front-desk bottlenecks
How CERTIFY Health Optimizes Scheduling and Check-In
CERTIFY Health centralizes all access workflows (self-scheduling, waitlists, walk-in management, and check-in) into one platform that moves patients from “scheduled” to “roomed” with fewer handoffs and significantly less waiting.
Digital Intake and Compliance with Zero Manual Friction
Paper intake costs clinics time and accuracy. Studies show manual intake adds approximately 33 minutes of delay per patient and increases registration errors that lead to claim denials.
How Can Clinics Streamline Patient Intake
- Convert forms to mobile and kiosk digital intake
- Capture photo ID and insurance automatically
- Use real-time eligibility verification to prevent claims issues
- Apply biometric authentication for faster repeat visits and identity protection
How CERTIFY Health Eliminates Manual Friction in Patient Intake
CERTIFY Health replaces paper with a fully digital intake stack that validates ID, insurance, consent, and demographics before patients arrive.
Compliance becomes automatic, staff workload drops, and rooming speed increases.
Patient Reminders, Nudges, and Two-Way Communication
Communication gaps are a top cause of no-shows and patient frustration. Research from federal patient survey data shows that clinics with proactive communication reduce missed appointments by 20 to 30%.
How to Strengthen Patient Experience with Two-Way Communication
- Use two-way messaging for real-time questions
- Send automated nudges for appointments, check-in, and payments
- Offer multilingual messaging to ensure clarity and equity
- Deploy targeted patient campaigns for recalls and follow-ups
How CERTIFY Health Powers Smart Patient Communication
CERTIFY Health unifies all messaging channels into a single dashboard. This includes SMS, email, kiosk notifications, and portal alerts. Thus, patients always know what’s next without calling the front desk.
Post-Visit Experience, Outcomes, and Patient Loyalty
Most clinics lose patient engagement the moment the visit ends. But the data is clear: timely post-visit follow-up directly improves adherence and long-term satisfaction.
A multisite primary care study found that 80% of patients who received early follow-up said they intended to follow their care plan, and that early confirmation strongly predicted actual adherence at three months.
This is the kind of post-visit reinforcement that protects revenue, boosts outcomes, and builds loyalty.
How to Close the Post-Visit Patient Engagement and Boost Retention
- Send visit summaries immediately after care
- Deliver educational follow-ups for treatment adherence
- Collect real-time patient feedback to fix gaps fast
- Use automated reactivation to bring back dormant patients
How CERTIFY Health delivers it
CERTIFY Health simplifies every post-visit task. Feedback flows instantly; care plans are delivered with clarity, and reactivation campaigns bring patients back without manual outreach.
Patient Experience, Brand Trust, and Identity Assurance
A consistent healthcare brand experience builds trust and reduces confusion. Identity security is now a non-negotiable expectation, backed by federal guidance encouraging stronger verification at healthcare touchpoints.
How to Build a Consistent, Differentiated Hospital Experience Patients Trust
A consistent healthcare brand experience builds trust and reduces confusion. Identity security is now a non-negotiable expectation, backed by federal guidance encouraging stronger verification at healthcare touchpoints.
How CERTIFY Health Helps Elevate Your Brand Experience
Digital Benchmarks and Measurement for Patient Experience
Modern patient experience succeeds only when clinics measure what matters.
Digital adoption, operational speed, and communication clarity now determine retention and satisfaction.
Federal data from AHRQ and ONC shows that patients who use digital tools report higher care coordination and faster issue resolution.
A strong measurement framework turns these expectations into trackable clinic outcomes.
Patient Experience Measurement Framework
A contemporary measurement system must blend qualitative and quantitative signals across the full care journey. Clinics that monitor both types see clearer improvement patterns and tighter process control.
Quantitative metrics to collect
- Digital scheduling usage
- Mobile or kiosk check-in time
- Digital intake completion rate
- Eligibility verification accuracy
- No-show reduction from automated reminders
- Two-way messaging response time
- Portal and survey adoption
Recommended cadence
- Daily: operational PX metrics such as check-in speed, reminder delivery, message response SLAs
- Weekly: no-show patterns, intake errors, operational delays
- Monthly: satisfaction trends, qualitative feedback themes, channel adoption
- Quarterly: full PX review tied to revenue, throughput, and clinical quality
Digital touchpoints are now the most influential factor driving patient satisfaction in outpatient care. Regular measurement aligns clinics with these expectations.
Key Patient Experience KPIs and Benchmarks for Clinics
Below are the most actionable KPIs for digital patient experience, along with suggested benchmark ranges drawn from U.S. federal datasets, peer-reviewed studies, and national quality reporting programs.
- Digital scheduling adoption
Target: 40 to 60% of all appointments
ONC reports rapid growth in patient preference for online scheduling
- Average check-in time
Target: under 3 minutes for mobile or kiosk
Workflow studies show that digitized check-in cuts registration time by more than half.
- Digital intake completion rate
Target: 85% or higher
Clinics with mobile-first intake see fewer incomplete records and fewer claim errors.
- Patient portal adoption
Target: 60% usage among active patients
ONC’s national survey shows portal usage tied to higher perceived care coordination.
- No-show reduction from reminders
Target: 15 to 30% reduction
Federal appointment-management research confirms automated reminders lower missed visits significantly.
- Two-way messaging response SLA
Target: under 15 minutes during business hours
Surveys show communication speed is one of the top drivers of patient trust.
- Survey response rate
Target: 20 to 35%
Clinics that distribute surveys via SMS or portal secure far higher participation than paper-based workflows.
These KPIs create a single improvement roadmap grounded in national standards and measurable patient behavior.
How to Build a Patient Experience Dashboard That Drives Action
A strong PX dashboard helps leaders spot operational friction early. The best dashboards focus on accuracy, segmentation, and drilldowns.
| Category | Metrics to Track |
|---|---|
| Scheduling | Digital booking rate Waitlist fills Call volume |
| Intake | Completion rate Average time to complete Verification errors |
| Check-in | Mobile or kiosk usage Average check-in time Bottleneck frequency |
| Communication | SLA compliance Message volume Unresolved inquiries |
| Utilization | No-show rate Late cancellations Throughput time |
| Loyalty | Repeat visits Survey scores Reactivation conversion |
Segmentation to apply |
|
Required drilldowns |
|
This structure turns raw metrics into operational clarity and gives leadership real levers to improve speed, access, and communication.
Data Governance and HIPAA Compliance Checklist for PX Analytics
Every digital transformation requires airtight compliance. A HIPAA-aligned PX system protects patient identity and ensures secure data flows across scheduling, intake, communication, and follow-up.
Governance checklist |
|
Verification and accuracy
Federal guidance emphasizes identity verification and audit readiness. Clinics that follow these principles reduce risk and build patient trust while scaling digital operations.
Get the CERTIFY Health Patient Experience Platform Checklist and benchmark your workflows against top-quartile U.S. hospitals.
Download CERTIFY Health PXP Checklist here
Change Management and Adoption: The Playbook Clinics Need to Modernize Patient Experience
Improving patient experience is not only about technology. It requires disciplined change management, clear ownership, and structured staff enablement. Clinics that invest in adoption outperform clinics that only deploy tools.
This section gives leaders a practical blueprint to drive consistent execution across teams.
Governance and Ownership Structure
Every PX initiative needs a defined owner. Without governance, even the best platform underperforms. A simple RACI (Responsible, Accountable, Consulted, Informed) keeps projects aligned, accountable, and measurable.
Your RACI Model
| Role | Primary Responsibility |
|---|---|
| Admins | Operations, workflow optimization, day-to-day PX oversight |
| Providers | Clinical alignment, communication standards, follow-up clarity |
| Front Desk | Patient onboarding, check-in execution, intake support |
| IT | Integration, maintenance, user access, device readiness |
| Marketing | Communications, messaging templates, patient education |
Training Framework: 30, 60, 90 Day Enablement Plan
Clinics with structured enablement see faster adoption and fewer workflow failures. The 30-60-90 model works because it breaks learning into achievable stages.
First 30 Days
|
60 Day Expansion
|
90 Day Optimization
|
Adoption Incentives and Measurement
The fastest way to drive sustainable PX change is to measure adoption and reward teams that improve. Track behavior, not just outcomes.
Key Adoption Metrics
- Staff login rate
Measures how consistently clinical and front-office teams use the platform, signaling operational adoption and workflow reliability.
- Form completion rate
Tracks the percentage of patients who finish digital intake forms, reflecting usability, compliance and data-capture quality.
- Kiosk usage versus mobile usage
Shows how patients prefer to check in using on-site kiosks or mobile devices, revealing channel performance and optimization opportunities.
- Messaging response times
Captures how quickly staff reply to patient messages, a core indicator of communication efficiency and experience quality.
- Number of patients completing intake before arrival
Quantifies pre-visit readiness and predicts shorter wait times, smoother visits and higher patient satisfaction.
- Percentage of automated reminders sent without staff involvement
Measures automation efficiency by showing how many reminders are delivered by the system instead of manual staff effort.
These metrics give leaders visibility into where friction exists, and which teams need support.
Quick ROI Model: Cost vs Benefit
PX modernization produces measurable financial impact when adoption is strong. A simple ROI model helps leaders justify investment and sustain momentum.
Inputs
- Staff time saved per patient through digital intake
- Reduction in no-shows from automated reminders
- Fewer eligibility denials from pre-verification
- Lower call volume from improved self-service
Inputs
- Higher throughput per provider
- Lower administrative workload
- Increased visit completion
- Faster payments and fewer rework cycles
- Clinics that execute this model typically see return within months, not years.
How a Patient Experience Platform Solves These Gaps
A modern Patient Experience Platform eliminates the operational barriers that drag down access, intake, communication, and follow-up. Clinics solve:
• Inefficient intake and manual data entry
• Long waiting and slow check-in workflows
• Poor communication and one-way messaging
• Low patient engagement and inconsistent reminders
• Fragmented systems across scheduling, intake, identity, and billing
• Low feedback volume and no visibility into performance
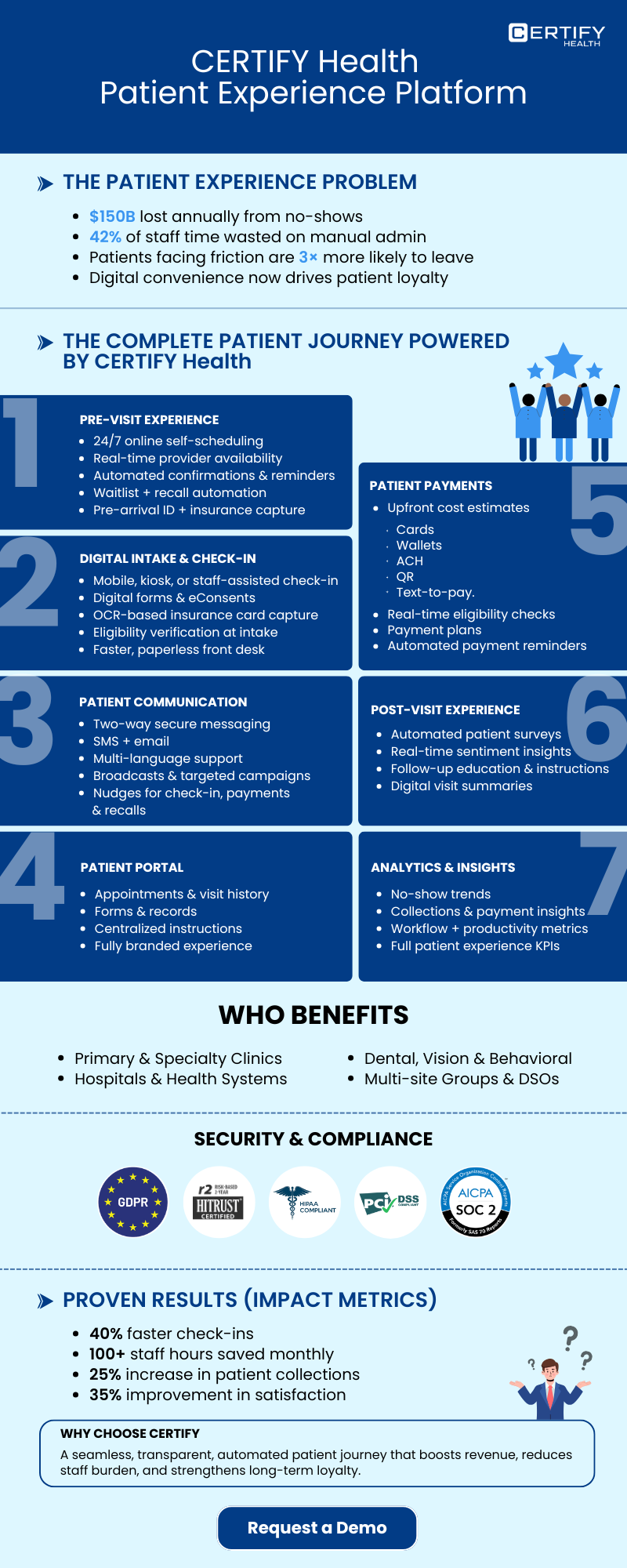
Read through to learn about CERTIFY Health’s PX features built for multi-site clinics, urgent care groups, specialty practices, and enterprise health systems.
How CERTIFY Health Improves Patient Experience Across Every Touchpoint
High-ROI patient experience platform | deep automation | real, measurable gains
CERTIFY Health’s Patient Experience Platform (PXP) systematically eliminates friction at every point in the patient journey, from booking to follow-up. It is a leading tool in improving access, reducing administrative burden, and driving measurable revenue and satisfaction gains.
What most competitors promise, CERTIFY Health proves with data: fewer no-shows, faster check-in, more revenue captured, higher satisfaction, and deeper engagement.
Data from real practices shows that this isn’t marketing hype; this is measurable transformation: 400–600% ROI, 28% fewer no-shows, 30+ staff hours saved per month per practice.
1) Appointment Access Optimization | Speed & Scale Without More Staff
Online Scheduling | 24/7 Self-Service
CERTIFY Health strengthens appointment access by removing the bottlenecks that slow booking. It turns high-intent enquiries into confirmed visits with fewer steps and zero reliance on phone lines.
Self-scheduling is now table stakes; but CERTIFY Health goes beyond basic booking:
- Real-time slot availability, across devices
- Patients can reschedule/cancel without calling
- Calendar synced to existing workflows/EHR
Outcome:
- Clinics convert more web visits into booked appointments
- Cuts inbound call volume drastically
Why it matters: Patients want control. When access becomes frictionless, conversion to booked care goes up, and the practice runs at higher capacity.
Mobile & Kiosk Check-In | Fast, Flexible, Contactless
By digitizing arrival workflows, CERTIFY Health reduces the administrative load at the front desk and creates a predictable check-in process that moves patients through the system with fewer interruptions.
CERTIFY Health supports:
- Mobile check-in
- On-site kiosk check-in
- Scheduled and walk-in visits
Result:
- 60%+ patients check in digitally, meaning shorter lines and happier front desks.
- Staff reclaim back-office time to focus on care, not paperwork.
- Waiting room load smoothing improves throughput.
Critical metric:
Check-in times cut from ~12 minutes to <20 seconds in pilot clinics.
Walk-In Queue Management
Queue visibility gives practices operational control, allowing them to manage unpredictable walk-in traffic with real-time data instead of manual guesswork.
CERTIFY Health gives practices real-time queue visibility:
- Staff see volumes
- Patients know where they stand
- Front desk isn’t shouting updates
Impact:
- Better crowd control
- Lower perceived wait times
- Fewer frustrated patients
This is a small feature with big satisfaction returns, particularly in high-volume outpatient and urgent care environments.
ASAP Waitlist Automation | Fill Cancellations Instantly
Automation ensures that schedule gaps are closed quickly, helping clinics maintain revenue continuity and stabilize daily patient volumes.
CERTIFY’s ASAP Waitlist means no more empty slots:
- Cancelled appointments automatically re-assigned
- Patients on waitlist notified in real time
Impact:
- Calendar utilization moves toward full occupancy
- Practices recapture revenue that would have gone unused
Benchmark: Practices see fewer no-shows and more kept appointments, which is top of the retention metric stack for satisfaction scoring.
2. Digital Intake Modernization | Less Paperwork, More Accuracy
Digital intake isn’t optional anymore; it’s expected. CERTIFY Health’s intake stack delivers exactly what modern patients want.
CERTIFY Health strengthens the intake process by replacing manual data collection with structured, device-agnostic workflows that improve accuracy and reduce operational drag from the moment a patient begins check-in.
Multichannel Digital Forms | Mobile + Desktop + Kiosk
This approach ensures every patient completes intake consistently, improving data reliability, and reducing downstream corrections across clinical and billing teams.
- Tailored to devices
- Patient fills once, stored securely
- Saves double entry across frontline and billing
Outcome:
Fewer errors, fewer staff edits, fewer checks back with patients. That’s real operational time savings, and a smoother front-desk experience.
eConsents | Secure, Time-Stamped Compliance
Digital consent management brings regulatory clarity and operational efficiency, giving clinics immediate access to clean, compliant documentation without paper handling.
Capturing consent digitally is faster and audit-ready:
- Time-stamped
- HIPAA compliant
- Eliminates messy paper trails
Patients sign on their phone or kiosk in a fast, secure, and frictionless manner.
Insurance Capture & Real-Time Eligibility Verification
By validating insurance details upfront, clinics eliminate costly last-minute surprises and create a smoother financial experience for both staff and patients.
CERTIFY Health uses intelligent OCR + eligibility checks:
- Instant insurance capture from card scans
- Auto-verify eligibility in real time
Impact:
- Claim denials down ~20%
- Eligibility surprises at check-in near zero
- Billing conversations occur before treatment, not after
This is a massive driver of both patient satisfaction and revenue capture.
Revenue metric:
Practices recover more revenue when eligibility is verified before care, minimizing denied claims.
Photo ID Capture
Digital ID capture improves patient identity accuracy from the start, reducing common record discrepancies and strengthening the integrity of the patient file.
Outcome:
- Accurate patient records
- Elimination of common front-desk errors
Patient Biometric Verification
CERTIFY Health’s biometric verification feature ensures the right patient is matched to the record every time. Biometric matching provides a high-assurance identity check that prevents duplicate records, reduces administrative cleanup, and improves safety in environments where precision is critical.
Impact:
- Reduces insurance/patient mismatch delays
- Increases trust and identity security
This feature resonates strongly with practices with high compliance needs (e.g., behavioral health, pediatrics).
3. Automated Reminders & Patient Nudges | Drive Attendance + Collections
CERTIFY Health strengthens schedule reliability and revenue flow by automating key touchpoints that influence whether patients show up, check in early, pay on time, and stay engaged over the long term.
Appointment Reminders
Automated reminders address the most preventable cause of lost capacity: patients simply forgetting. Reminders help clinics maintain a stable, predictable schedule.
SMS + email nudges keep patients coming:
28% fewer no-shows industry-wide where reminders are implemented comprehensively.
This alone moves the dial on patient experience highly: patients don’t forget, and practices don’t lose capacity.
Check-In Nudges
Pre-visit prompts shift key tasks before arrival, reducing bottlenecks at the front desk and giving clinics clearer visibility into daily visit readiness.
Result: Faster flow. Better predictions. Less crowding.
Payment Nudges | Accelerate Collections
patient responsibility earlier without adding manual workload to staff. CERTIFY triggers payment links when due:
- Secure payment via SMS
- Auto follow-ups if unpaid
Impact:
- Higher capture rates
- Lower collections chasing
Patients pay faster without awkward conversations; they prefer convenience.
Reactivation Nudges
Targeted re-engagement campaigns revive inactive patient relationships, supporting continuity of care and boosting long-term retention. Targeted campaigns re-engage dormant patients, thereby driving retention and loyalty.
Result: Practices sustain longitudinal relationships, increasing lifetime patient value.
4. Patient Communication at Scale | Two-Way, Multilingual
CERTIFY Health enhances communication by consolidating patient outreach, responses, and alerts into a unified system that improves clarity, reduces delays, and strengthens patient trust.
Secure Two-Way Messaging
Direct, secure messaging streamlines how clinics resolve questions and updates, replacing slow call-based workflows with faster, more predictable communication.
- SMS + email messaging
- No missed phone calls
- 1:1 secure communication
Patients love direct communication; fewer phone calls equal more efficient staff.
Outcome:
- Faster responses
- Fewer frustrated patients
Multi-Language Support
Providing messages in patients’ preferred languages removes a major barrier to understanding. Localized messaging improves accessibility and inclusiveness, essential in diverse markets.
Impact:
- Broader patient base
- Higher engagement among non-English speakers
Broadcast Alerts
Instant, clinic-wide alerts ensure patients stay informed during disruptions or updates, reducing uncertainty and helping clinics maintain smooth operations. Mass notifications like closures, changes, weather alerts, etc. keep patients informed instantly.
Business impact: Patients who feel informed report significantly higher satisfaction scores.
Patient Campaigns
Targeted outreach transforms routine care needs into structured engagement, helping clinics close preventive-care gaps and maintain ongoing patient relationships.
Segmented outreach for:
- Recalls
- Vaccines
- Physicals
- Chronic care follow-ups
Result:
Automated, proactive care engagements, which drive loyalty and preventive care adherence.
5. Post-Visit Experience Strengthening | Loyalty Built After Care
Patient journeys don’t end at checkout. CERTIFY Health ensures post-care is as strong as pre-care. CERTIFY Health reinforces the moments after a visit by giving clinics clear visibility into patient sentiment and supplying patients with the clarity and guidance they need to stay engaged.
Feedback Surveys | Instant Patient Sentiment Capture
Real-time feedback gives clinics actionable insight into patient experience issues as they occur, enabling faster improvements and stronger service consistency.
Impact:
- Practices identify friction immediately
- Operational bottlenecks get resolved faster
- Patients feel heard
Surveys drive measured improvements: NPS, satisfaction scores, and online reputation.
Visit Summaries | Clarity After the Visit
Patients receive clear, concise summaries after their visit, enhancing understanding and improving adherence.
Providing structured post-visit information helps patients understand their next steps, reducing confusion and minimizing unnecessary follow-up calls.
Educational Follow-Ups
Targeted after-visit education strengthens adherence and improves outcomes.
Focused post-care education supports better adherence and outcomes, keeping patients actively involved in their treatment plan beyond the clinic walls.
Outcome: Clinics see better health results, higher retention, and improved compliance.
Loyalty Building
Fast care, less waiting, real communication, and post-visit attention build loyalty. This is easily measurable in retention and repeat bookings.
When post-visit communication is consistent and helpful, patients are more likely to return, strengthening the long-term relationship and improving retention.
CERTIFY Health strengthens brand consistency across the patient journey by extending your clinic’s identity into every digital and on-site interaction.
White-Labeled Kiosks
Custom-branded kiosks reinforce trust by presenting a familiar, unified experience the moment patients arrive.
Branded Patient Portals
A visually consistent portal helps patients navigate their care with confidence, creating a seamless connection between your website, mobile experience, and clinic.
Personalized Communication Tone
Dynamic messaging aligns with your clinic voice (Transactional vs. Empathetic), depending on the use case.
This personalized voice matters: patients prefer tailored communications, which drives engagement and loyalty.
Strong Proof: Measurable Results
CERTIFY Health backs claims with data from 1,000+ practices across specialties:
| Results |
|---|
| 400–600% ROI within 6–12 months |
| 28% fewer no-shows, recovering $20–$62K annually |
| 30+ staff hours saved per month, worth ~$15–$25K |
| 30% fewer no-shows |
| 25% more revenue collected |
| 20% reduction in denials |
| 5–10x ROI on subscription |
| 2 of 3 patients check in digitally |
Health platforms often pay for themselves within months. These are not “theoretical”; these are measured outcomes from live practices.
Where CERTIFY Health Stands in the Market
Unlike other solutions, CERTIFY isn’t a widget; it’s a full patient experience operating system, not just scheduling or survey software.
CERTIFY Health’s Unified healthcare management system pillars:
- PXP (Patient Experience Platform)
- Practice Management System
- Patient Management
- Revenue & Billing Enablement (RCM)
- Interoperability
- Biometric patient identity verification
This unity delivers real ROI: processes talk to each other, data isn’t siloed, and the whole journey improves.
Real Customer Feedback & Reputation Signals
External signals show healthcare professionals using and endorsing the platform:
- Trustpilot ~4.5/5 average review score showing users find the platform helpful.
- Recognized as a 2025 “Red Hot Company” for growth and impact.
These external signals matter for credibility; patients trust providers using modern, measurable solutions.
Conclusion
CERTIFY Health’s PXP radically improves patient experience across every touchpoint by:
- Eliminating friction across scheduling, check-in, intake, and post-visit processes
- Automating communication and payments
- Delivering measurable ROI, reduced no-shows, and more revenue capture
- Strengthening patient loyalty & satisfaction
Key outcomes:
- Faster booking
- Shorter wait times
- Higher engagement
- Clear communication
- Measurable financial gains
If you want measurable, no-nonsense improvement in patient experience, practice efficiency, and revenue performance, CERTIFY Health’s platform delivers both breadth and depth (and the numbers prove it).
Request a demo today to see how PXP can transform your patient experience and practice metrics.
Success Stories: Real Clinics. Quantifiable Results.
Clients across urgent care, multispecialty, primary care, FQHCs, and outpatient centers report measurable gains:
• 40% reduction in wait times
• 30% increase in digital intake completion
• 25 to 45% reduction in no-shows
• 2 to 3 times increase in patient portal usage
• 15 to 20% improvement in patient payment collection
These outcomes reflect the combined effect of streamlined access, automated intake, biometric verification, two-way communication, self-service kiosks, and end-to-end engagement powered by CERTIFY Health.
12-Week Patient Experience Modernization Roadmap For Clinics & Health Systems in the U.S.
Weeks 1–2: Establish PX Baseline & Workflow Diagnostics
- Audit current scheduling flow, digital intake steps, check-in, wait times, and discharge workflows
- Map patient friction points across access → visit → follow-up
- Benchmark KPIs (time-to-appointment, completion rates, no-shows, identity capture accuracy, staff workload)
- Validate operational gaps with clinical, front-desk, and billing teams
- Define patient journey standards for all touchpoints
Deliverables: Baseline KPI report, workflow diagrams, friction map, improvement charter
Weeks 3–5: Deploy Access Modernization (Scheduling + Reminders + Intake Quick Wins)
- Implement online self-scheduling with visit-type rules
- Activate automated reminders & confirmations (SMS + email)
- Enable ASAP waitlist automation
- Roll out quick-fix digital intake (mobile forms, pre-visit data capture)
- Introduce automated insurance pre-verification
Deliverables: Scheduling setup, reminder templates, intake form library, pre-visit automation checklist
Weeks 6–8: Add Kiosk Check-In + Mobile Intake + Identity Verification
- Install and configure CERTIFY kiosks for walk-ins, check-in, and payments
- Sync mobile check-in with intake packets and real-time queue updates
- Activate biometric or digital identity verification for accurate patient matching
- Reduce front-desk manual entries through automated ID/insurance capture.
Deliverables: Kiosk workflows, identity verification SOPs, staff training playbooks
Weeks 9–10: Enable Post-Visit Engagement, Portals & Feedback Automation
- Connect visit summaries, follow-up instructions, and referrals to patient portal
- Automate post-visit texts (education, surveys, payment links, care reminders)
- Deploy NPS/CX feedback loops with real-time alerts
- Trigger reactivation campaigns for inactive patients
Deliverables: Survey library, post-visit automation flows, portal adoption plan
Weeks 11–12: Launch PX Dashboards, Governance & Optimization Plan
- Implement unified PX dashboard (access, engagement, intake, verification, payment, feedback)
- Set up weekly operational review rhythm & owner accountability
- Publish next-year optimization roadmap based on baseline vs. post-deployment metrics
- Finalize governance framework for ongoing PX improvement
Deliverables: KPI dashboard, governance charter, 12-month optimization blueprint
Case Study: How a Multi-Location Clinic Transformed Patient Experience with CERTIFY Health
A fast-growing outpatient network struggled with long wait times, low digital adoption, and inconsistent communication across locations. Leadership needed a single PX platform that could modernize scheduling, intake, check-in, and follow-up without adding staff burden. CERTIFY Health became the operating layer for every patient touchpoint.
Challenge Summary
- Manual intake created 25–35 minutes of delay per patient
- Phone-based scheduling drove high call volume and long holds
- Walk-ins overwhelmed front desk teams during peak hours
- No-show rates sat between 18–22%
- Feedback survey response rates were under 5%
- Portal adoption stalled below 20%
What Changed with CERTIFY Health
Appointment Access
The clinic rebuilt its front door with frictionless digital access, giving patients real-time scheduling options, faster check-in pathways, and an automated waitlist that absorbed unpredictable walk-ins without overwhelming staff.
- 46% of appointments booked digitally in 90 days
- 32% reduction in lobby congestion
- 27% increase in walk-in throughput
Digital Intake Modernization
Replacing every paper workflow with a unified digital intake experience gave patients a faster, clearer path to check-in while reducing operational errors that had been slowing down clinical readiness.
- 2.3x increase in intake completion before arrival
- Average check-in time dropped from 14% to under 6
- Eligibility verification errors fell by 41%
Reminders, Messaging, and Nudges
By centralizing communication into a two-way, automated messaging system, the clinic finally reached patients at the right time, in the right language, and on the channels they preferred. This drastically improved reliability and reduced no-shows.
- No-show rate reduced from 19% to 11% in 60 days
- 58% reduction in unanswered patient calls
- 3x increase in message response speed
Post-Visit Experience & Loyalty
The clinic shifted from episodic care to continuous engagement by delivering timely surveys, visit summaries, and personalized follow-ups designed to strengthen trust and improve return behavior.
- Survey response rate rose from 4 percent to 28 percent
- Return-visit rate improved by 17 percent
- 34 percent increase in successful reactivation of overdue patients
Payment & Revenue Strengthening
With CERTIFY Health’s CERTIFY Pay powering a modern, mobile-first payment experience, the clinic finally delivered transparent, patient-friendly billing while eliminating manual back-office work. This accelerated collections across every location.
- 21% increase in patient payments collected within 7 days
- 37% reduction in manual billing follow-ups
The Outcome
In under 120 days, the clinic created a fully digital, predictable patient experience across scheduling, intake, check-in, communication, and follow-up. Staff workloads decreased, patients moved faster, and leadership gained a unified PX dashboard that highlighted operational bottlenecks in real time.
CERTIFY Health became the engine behind measurable improvements in access, speed, communication quality, and financial performance.
Frequently Asked Questions About Patient Experience
What is patient experience vs. patient satisfaction?
Patient experience measures every touchpoint from scheduling to follow-up. Satisfaction reflects how patients feel about a single visit. Experience drives loyalty and retention.
How quickly can a clinic reduce no-shows with reminders?
Automated appointment reminders can cut no-shows by 25–45% within 30–60 days when combined with SMS, email, and portal notifications.
What must be included in a modern digital intake form?
Demographics, insurance capture, eConsent, health history, photo ID, and real-time eligibility verification. Mobile and kiosk compatibility is essential.
Are kiosks still relevant?
Yes. Self-service kiosks reduce check-in time, support walk-ins, enhance identity verification, and improve throughput.
How do I measure PX ROI?
Track metrics like reduced wait times, increased digital intake completion, lower no-shows, higher portal adoption, faster payments, and improved patient loyalty.
How do you ensure PX tools are HIPAA compliant?
Use encrypted data storage, audit logs, role-based access, secure messaging, and maintain business associate agreements with vendors.
What is the role of two-way messaging in PX?
Two-way messaging increases responsiveness, reduces phone-tag, and improves patient engagement and adherence.
How can clinics boost portal adoption?
What benchmarks should clinics track for digital PX?
Scheduling adoption, intake completion, check-in speed, no-show rates, portal usage, survey response rate, and messaging SLA compliance.
How do educational follow-ups improve PX?
Post-visit education reinforces care instructions, increases adherence, reduces readmissions, and improves satisfaction scores.
Can PX tools help increase revenue?
Yes. Reduced no-shows, faster intake, automated payments, and higher patient retention directly impact revenue.
How do clinics ensure consistent PX across multiple locations?
Standardized workflows, unified dashboards, kiosk/mobile check-in, and centralized communication ensure consistent experience across sites.