Table of Contents
Introduction
The behavioral health market is growing fast—expected to reach $330.35B globally by 2034, with the U.S. accounting for nearly half of that expansion. But with growth comes mounting reimbursement pressure and tighter margins for outpatient clinics.
For clinics with 1–3 sites and 5–80 full-time staff, led by Program Directors, Billing Supervisors, and Clinical Directors, the uphill battle against insurance rules, billing errors, and workforce turnover is all too familiar.
If you’re reading this, you don’t need a lecture on your pain points. What you need is a clear, proven framework for evaluating behavioral health RCM solutions that actually plug your revenue leaks. Grab your notepad—because by the end, you’ll know exactly how to guide your team through the RCM selection process and get measurable results.
What is Behavioral Health Revenue Cycle Management?
Behavioral Health Revenue Cycle Management (RCM) oversees every financial step of a patient’s journey—from scheduling appointments and verifying insurance to coding, submitting claims, managing denials, and collecting payments.
What Makes RCM for Behavioral Healthcare Centers So Complex?
TL; DR:
What are the key challenges that make RCM for behavioral health clinics complex?
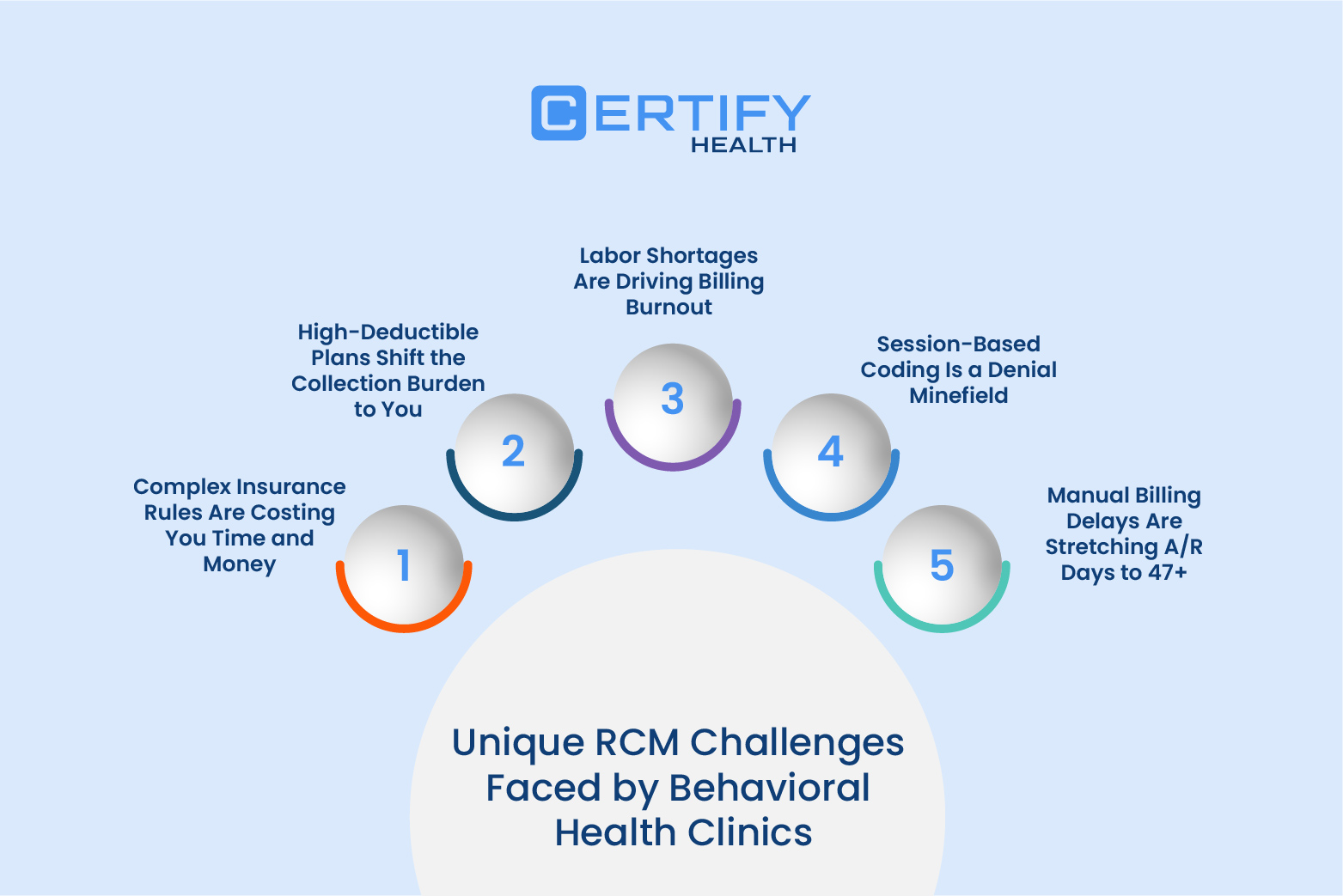
Behavioral health clinics face unique and significant hurdles in RCM like:
- Complex insurance rules cause high claim denials and delayed payments.
- Patient high-deductible plans increase revenue collection challenges.
- Labor shortages drive billing errors, slower processing, and staff burnout.
- Session-based coding mistakes lead to frequent, preventable claim denials.
- Manual billing delays extend accounts receivable days beyond best practice.
These challenges collectively strain clinic revenue and staff efficiency.
Understand Your Clinic’s Unique RCM Challenges
Complex Insurance Rules Are Costing You Time and Money
Let’s not sugarcoat it: behavioral health clinics frequently see denial rates. Why?
- Inconsistent payer policies
- Missing prior authorizations
- Session limits per plan
The fallout: delayed reimbursements, A/R days well above best practices, and depressed clean claim rates. Every denial and rejected claim means your team spends more rework time, pushing claims backlog and stretching staff overtime.
Key KPIs:
- Clean claim rate
- Days in A/R
- Denial rate
Research shows that providers lose about $500,000 annually due to denials and delays; manual RCM tools can slow payments by 8+ weeks.
High-Deductible Plans Shift the Collection Burden to You
With 58% of patients now holding high-deductible plans, the risk is clear: patient balances make up nearly 30% of revenue, yet less than half is ever collected at the point of care. Outstanding patient balances and increasing write-offs steadily erode net revenue, triggering a compounding financial strain on your bottom line.
Key KPIs:
- Net patient revenue
- Point-of-service collection rate
- % of patient-responsibility A/R
HDHPs (High-Deductible Health Plans) are linked to a 4.8% reduction in mental health care spending, with direct impacts on access and outcomes.
Pro tip:
Solutions like CERTIFY Health’s CERTIFY Pay, offer modern payment options like online payments, payment links, virtual terminals (for card payments), omnichannel payments, and QR payments to help clinics collect patient balances efficiently, minimizing write-offs and improving cash flow through seamless integrations.
Labor Shortages Are Driving Billing Burnout
Labor shortages and staffing issues aren’t just HR problems—they are financial threats. High turnover and burnout lead to billing errors, slower turnaround times, and an ever-worsening claims backlog. The process grinds down staff morale and results in more overtime—and, eventually, more turnover.
Key KPIs:
- Claims processing turnaround time (TAT)
- Billing error rate
- Staff overtime hours
Over 45.2% of physicians report symptoms of burnout—burnout which worsens as patient demand outpaces workforce growth.
Session-Based Coding Is a Denial Minefield
Behavioral health billing centers rely on time-based session codes—think 90837, among others. Unfortunately, one misstep in code selection or case manager documentation can lead to denial rates (1 in 5 and 80% of them are preventable), rejected claims, and compliance issues.
Key KPIs:
- Coding accuracy rate
- First-pass claim acceptance rate
- Denial rate by CPT code
Manual Billing Delays Are Stretching A/R Days to 47+
Relying on manual billing and patient statement cycles? You are likely stuck at a median of 47.3 A/R days—far from best practice (<30 days). This means longer timelines to get paid, more unpaid patient balances, and lower patient satisfaction.
Key KPIs:
- Days in A/R
- Patient billing cycle length
- Collection rate over 30/60/90 days
Pro Tip: Behavioral health billing isn’t just complex—it’s personal. With CPT coding inconsistencies and evolving payer rules, one small error can stall reimbursement.
CERTIFY Health’s Revenue Cyle Management solution is purpose-built for behavioral health clinics, with automated coding checks, eligibility verification, and claims scrubbing that dramatically reduce denial rates.
Curious how it handles your specialty’s quirks? Book a Demo Now.
You might also like to read: 8 Tactics to Improve Healthcare Revenue Cycle Management
What is Behavioral Health RCM tool?
A Behavioral Health Revenue Cycle Management (RCM) tool is a specialized software platform designed to streamline and optimize the entire billing and revenue process for behavioral health clinics. It manages complex billing workflows, payer-specific rules, session-based coding, prior authorizations, and compliance needs—all tailored to the unique challenges of behavioral healthcare services.
Benefits of a Behavioral Health RCM Tool:
- Customized workflows that align perfectly with your clinic’s service types and documentation practices, minimizing manual workarounds.
- Improved claim accuracy and faster reimbursements by automatically applying payer-specific rules and catching errors pre-submission.
- Real-time dashboards providing clear financial and operational insights, empowering teams with actionable revenue metrics.
- Seamless integration with electronic health records (EHR), clearinghouses, and accounting systems to reduce duplicate data entry and errors.
- Enhanced compliance with healthcare regulations and data security standards, protecting sensitive patient and billing information.
- Scalable technology that grows with your practice, avoiding unnecessary costs on unused features and allowing easy updates.
RCM for Behavioral Healthcare Centers: Essential Features to Optimize Your Practice
Here’s what sets the best behavioral health RCM solutions apart from others:
Feature Category | Why It Matters |
Customizable Payer Logic & Automation | Adapts to different payer policies, with pre-auth, session caps, and state-specific insurance rules. |
Upfront Patient Financial Management | Integrates real time eligibility, supports payment plans, and manages patient balances. |
Denial Tracking & Analytics | Tracks denial rates by payer and code, automates rework, and helps visualize compliance issues. |
Seamless EHR & Integration | Syncs therapist, psychiatrist, and case manager documentation for flawless claims submission. |
Labor-Saving Workflow Tools | Auto-posts payments, edits claims in batches, and sends self-serve patient statements. |
Therapist-Friendly Documentation Sync | Syncs notes, treatment plans, and codes in real time to cut rework, reduce denials, and stay compliant. |
Pro Tip: Checking off a feature list is one thing—having them work together seamlessly is another.
That’s where CERTIFY Health’s end-to-end RCM toolkit shines. It’s not just a billing engine—it connects scheduling, documentation, payment, and reporting under one smart interface.
Want to test-drive a platform that’s tailored to behavioral workflows? Book your personalized walkthrough now.
Bonus Tip: When taking a demo of RCM solutions, ask vendors to show how their rules engine handles a typical 90837 (60-min psychotherapy) with dual payer coverage.
Step-By-Step Selection Process
TL; DR:
How to choose behavioral health RCM solutions?
- Form an evaluation team including program director, billing supervisor, and clinician for balanced insights.
- Benchmark current KPIs like denial rates, A/R over 90 days, and staff overtime.
- List must-have vs. nice-to-have features focused on key pain points.
- Shortlist vendors with behavioral health experience and request references.
- Use scorecards during demos to evaluate KPI impact, usability, and cost.
- Pilot chosen solution for 60 days; measure improvements in claims and staff efficiency.
- Finalize contract with service guarantees on denial rates and support response.

1. Assemble an Evaluation Team
Include your Program Director, Billing Supervisor, and one frontline clinician. Diverse roles = well-rounded decisions.
2. Benchmark Your Current KPIs
Track your baseline metrics: claim denial rates, A/R over 90 days, collection percentages, billing team overtime, error frequency, and claims turnaround time.
3. Draft Must-Have vs. Nice-to-Have Features
Reference the essential RCM tools features listed above—focus on what solves your highest-cost pain points.
| Must-Have Features | Nice-to-Have Features |
|---|---|
| Time-Based Session Coding Support | AI-Powered Auto-Coding & Session Summarization |
| Customizable Payer-Specific Rules and Logic | AI-Driven Denial Prediction and Resolution |
| Prior Authorization Management | Patient Billing Chatbots for 24/7 Query Handling |
| Session Tracking and Visit Caps | Advanced Revenue Forecasting |
| Real-Time Insurance Eligibility Verification | Customizable Reporting and Alerts |
| Automated Claims Scrubbing and Error Checking | Integration with Telehealth Platforms |
| Denial Management Tools with Quick Resubmission | Flexible Patient Payment Plans & Online Portals |
| Integration with EHR/EMR Systems | Patient Financial Transparency Tools |
| Compliance and HIPAA Data Security | Customized Workflows for Multi-Provider Collaboration |
| Automated Payment Posting and Reconciliation | AI-Powered Revenue Analytics |
| Analytics and KPI Dashboards | Multi-location Management |
| Efficient Patient Balance Management and Collections | Interoperability Across Health Information Exchanges (HIE) |
4. Vendor Shortlisting & RFI
Request references from similar behavioral health clinics (ideally 1–3 sites). Ensure they understand the unique payer logic and compliance issues in your space.
5. Scorecard Demo Sessions
Weigh solutions by their impact on key KPIs, usability, staff rework time, compliance support, and cost.
6. Pilot & Measure
Run a 60-day parallel pilot. Track lift in clean claims rate, drop in denial rates, staff hours saved, and turnaround times.
7. Finalize Contract
Insist on service-level guarantees: denial reduction targets, support response times, and RCM solution uptime.
Pro Tip: CERTIFY Health offers a frictionless onboarding experience, with plug-and-play EHR integrations and intuitive dashboards that don’t overwhelm your staff.
Still evaluating options? Schedule a live demo
Calculating ROI: Quick Formula for Small Behavioral Healthcare Centers
Let’s get practical:
- Reduce denial rates by 10%: If annual revenue = $3M, and denials currently cost you 8%, reclaiming even 10% lifts collections by $24,000/month.
- Formula: Increase in collections =Annual revenue x Denial rate x fraction of denials you aim to reclaim
- Cut billing hours by 15%:
On $3M revenue, if billing costs are $150,000/year, saving 15% returns $22,500/year.
Formula: Savings=Billing costs x Savings percentage
- Improve patient collections by 8%: With $1M in patient balances, lifting your patient payment plans and collection rates adds $80,000 in cash flow.
Formula: Increased cash flow=Patient balances x Improvement percentage
Result? Most clinics see ROI from a modern behavioral health RCM solution like CERTIFY Health’s RCM tools in less than 9 months—sometimes far sooner, especially when key KPIs improve across multiple pain points.
You might also like to read: How to Measure Patient Collections: 5 Key Metrics for the Healthcare Revenue Cycle
Common Pitfalls to Avoid
- Opting for a generic RCM solution without behavioral health-specific payer logic leaves you scrambling for workarounds (and more denied claims).
- Overlooking patient financial management features like payment plans and real time eligibility means your patient receivables and write offs spiral.
- Ignoring the clinician workflow fit often results in documentation gaps and more compliance issues, sending denial rates soaring.
- Underestimating the need for training and support can leave your small billing team vulnerable to billing errors and unnecessary rework time.
Conclusion
The right behavioral health RCM solution is not just a piece of tech—it’s your revenue defense, your staff support system, and a crucial tool for patient financial management. Stop the snowball effect of claims backlog, burnout, and revenue loss.
Ready to take control? Check out: Top 10 Revenue Cycle Management Solution in 2025 or Book a 30-minute discovery call with our experts and see how a tailored RCM solution can transform your clinic’s bottom line—without further delay.
FAQ's
What’s the average denial rate for behavioral health clinics?
Industry averages show denial rates ranging from 10%–20%, though behavioral health clinics often face higher rates due to session-based coding and inconsistent payer rules.
What common reasons cause claim denials in behavioral health?
In behavioral health, the following are typical reasons for claim denials:
- Missing or incorrect prior authorizations required by many payers.
- Patient eligibility issues or inaccurate insurance verification.
- Coding errors due to complex, session-based coding and payer-specific rules.
- Incomplete or insufficient documentation to prove medical necessity.
- Claims exceeding coverage limits or visit caps.
- Late or untimely claim submissions beyond insurer deadlines.
- Duplicate claims or billing discrepancies across providers.
How does behavioral health billing differ from general medical billing?
Behavioral health billing focuses on session-based services like therapy and counseling, often requiring time-based CPT codes, frequent prior authorizations, and adherence to stricter privacy regulations. Unlike general medical billing, which is procedure-oriented and covers physical health treatments, behavioral health billing involves unique payer rules, session limits, and more complex documentation to ensure compliance and reimbursement.
How soon can a small behavioral clinic see ROI from a new RCM system?
With reduced denial rates and streamlined claims, many clinics see ROI in as little as 6–9 months—sometimes sooner if key KPIs improve across denial management and patient collections.
























