Table of Contents
Dental specialties face unique set of operational and financial hurdles across practice scales in the U.S., from independent clinics to large DSOs, and health systems. This guide is created for those dental specialties who face particular pain points and looking for technology driven solutions to solve these challenges.
The Quiet Crisis Behind Dental Practice Closures in the U.S.
In just one year, Becker’s Dental has tracked 18 dental practice closures across the U.S. and these aren’t isolated incidents or small-market anomalies. They span private practices, orthodontic groups, community clinics, nonprofit organizations, and academic dental centers, revealing a systemic strain across the dental ecosystem.
What’s striking is why these practices closed:
- Financial pressure and funding cuts (community clinics, nonprofits, emergency dental centers)
- Staffing shortages and provider dependency (single-dentist practices unable to recruit)
- Operational fragility (billing delays, poor continuity, lack of redundancy)
- Organizational risk concentration (closures triggered by one event – death, accident, or compliance issue)
This isn’t about demand disappearing. It’s about operations failing to scale, absorb shocks, or adapt.
17 Dental Practice Shutdowns That Reveal a Deeper Industry Breakdown
| Serial No. | Practice / Organization | Location | Closure Trigger | Underlying Vulnerability Exposed |
|---|---|---|---|---|
| 1 | Family 1st Dental | Nebraska (2 locations) | Dentist shortage | Heavy dependence on a single provider |
| 2 | The Smiling Face Company | North Carolina | Abrupt orthodontic shutdown | Continuity risk in long-term treatment models |
| 3 | Glendale Heights Family Dental | Illinois | Facility damage | Lack of operational redundancy |
| 4 | Harvard School of Dental Medicine Clinic | Massachusetts | Permanent clinic closure | Academic cost-containment pressure |
| 5 | Independent DDS Practice | Missouri | Legal enforcement | Compliance and governance failure |
| 6 | MetroHealth Dental Clinic | Ohio | Cost-cutting initiative | Financial sustainability strain |
| 7 | Dental Group Orthodontics | Texas | Full practice closure | Revenue and staffing instability |
| 8 | Scott Ervin, DDS | Texas | Owner’s sudden death | No succession or continuity planning |
| 9 | Orange County Emergency Dental Clinic | California | Federal funding cuts | Reliance on external reimbursement |
| 10 | Community Clinical Services (Pediatric) | Maine | Budget shortfall | Thin margins in pediatric care |
| 11 | Independent Dental Clinic | Wisconsin | Unexplained closure | Operational fragility |
| 12 | Medgaus Dental Group | Pennsylvania | Owner’s passing | Single-owner risk concentration |
| 13 | Hope Dental Clinic | Minnesota | Failed fundraising | Nonprofit funding volatility |
| 14 | Orthodontic Practice | Connecticut | Facility damage | Business interruption exposure |
| 15 | The Kid’s Dentist | New York | Sudden temporary closure | Poor patient communication systems |
| 16 | My Community Dental Centers (6 sites) | Michigan | Financial distress | Multi-site cost pressure |
| 17 | Southern Tier Orthodontics | New York | Personal + financial strain | Practice resilience gap |
Source : Beckers Dental
This guide is built to address a hard truth:
It’s not clinical care that sinks dental practices. It’s operations and finances.
In the sections ahead, we break down the core pain points driving dental practice instability.
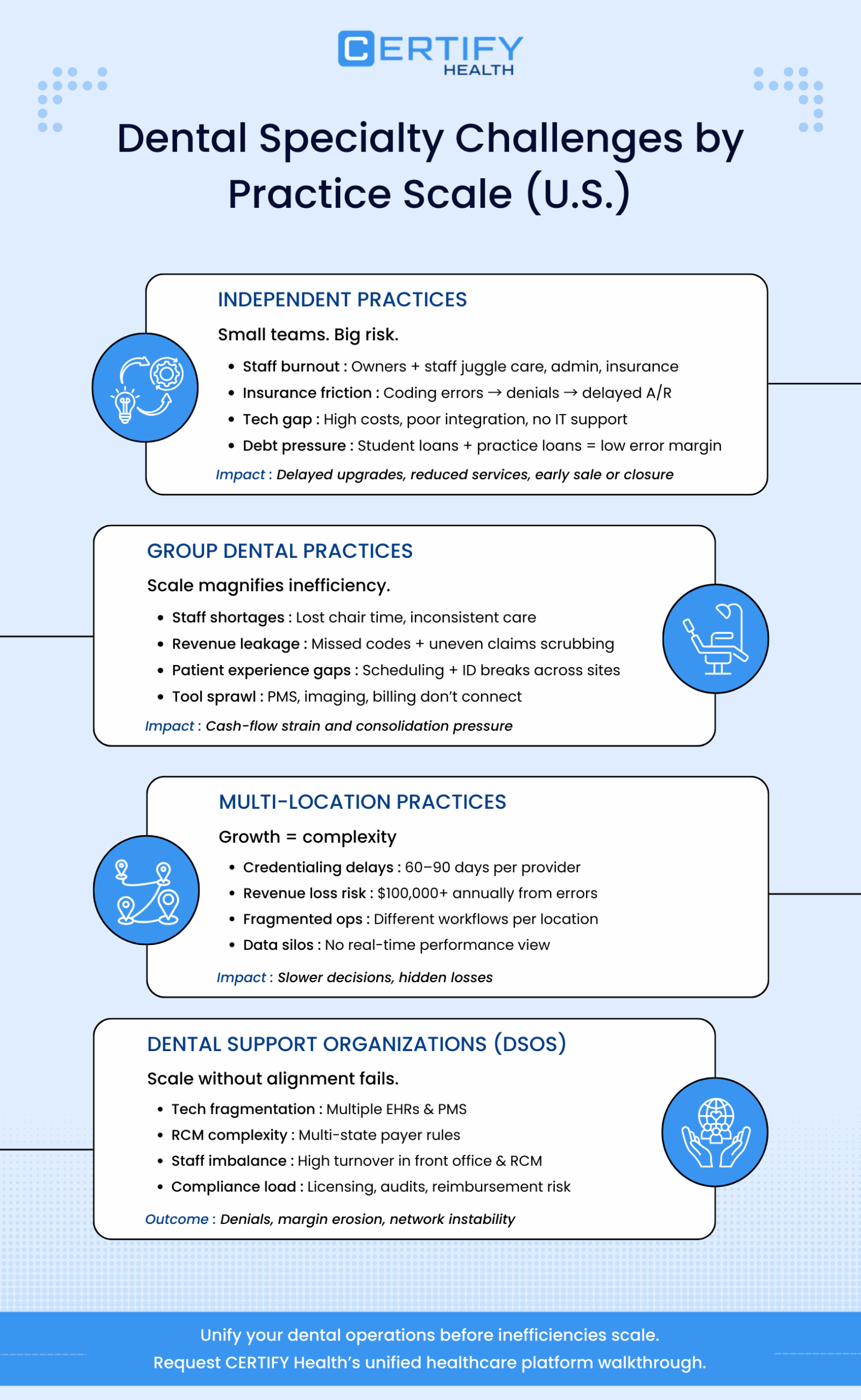
Dental Specialty Challenges by Scale
I. Independent Practice Challenges
This section explores the core pain points, revealing how interconnected issues like burnout, insurance friction, and tech gaps amplify risks for practices determined to stay independent.
1. Staffing Shortages and Burnout in U.S. Dental Practices
Staffing remains one of the most pressing challenges across U.S. dental practices, with orthodontic clinics particularly affected due to their reliance on specialized assistants and coordinators.
- Front-desk teams manage high patient volumes, insurance questions, and long treatment plans
- Clinical staff juggle chairside care alongside documentation and coordination
- Practice owners often absorb administrative tasks when staffing gaps emerge
While exact burnout percentages vary by market, industry commentary consistently highlights staff fatigue and turnover as a top operational risk for independent dental clinics, especially those without centralized systems to reduce manual work.
2. Insurance Complexity & Denial Management
Navigating payer rules, documentation requirements, and reimbursement delays has become increasingly difficult for independent dental clinics.
Common pain points include:
- Insurance denials due to coding or eligibility errors
- Delayed payments stretching days in A/R
- Heavy dependence on experienced billing staff, who are hard to hire
Insurance friction disproportionately impacts small practices that lack scale or automation.
3. Administrative Complexity & Workflow Inefficiency
Solo practices often rely on manual or semi-digital workflows across scheduling, billing, insurance verification, and documentation. Over time, this leads to:
- Administrative bottlenecks and daily operational friction
- Increased staff stress and role overload
- Inconsistent patient experiences
Operational inefficiency compounds quickly when a small team is responsible for both care delivery and business execution.
4. Structural Disadvantages for Independent Dental Practices
Across studies and industry surveys, a consistent theme emerges:
Independent dental practices face structural disadvantages compared to larger group models when it comes to scale, technology, and administrative efficiency.
APOS research notes a gradual decline in solo practice prevalence, driven by:
- Administrative overload
- Technology complexity
- Desire for operational support and work-life balance
This does not mean independent dental clinics are obsolete, but it does mean operating independently now requires smarter infrastructure and tighter workflows.
5. Technology Gaps in Independent Dental Clinics
Technology adoption is no longer optional, but it is unevenly accessible.
Research published by APOS highlights that solo and independent dental clinics struggle more than group practices or DSOs to keep pace with modern technology demands due to cost, complexity, and limited IT support.
Common technology challenges:
- High upfront costs for modern platforms
- Multiple point solutions that don’t integrate
- Ongoing maintenance without dedicated IT staff
While digital tools can improve outcomes, fragmented technology stacks often increase administrative burden instead of reducing it, especially in smaller practices.
Competitive reality:
Larger group practices and DSOs can spread technology costs across locations, while independent dental clinics absorb them alone, creating a widening operational gap.
6. When Student Debt Meets Ownership Risk: A Growing Financial Squeeze
Many independent dental practice owners enter ownership already carrying significant educational debt, often while taking on additional loans to acquire, expand, or modernize a practice. This dual financial burden places solo and small-group practices in a uniquely vulnerable position.
This pressure creates several downstream effects:
- Elevated financial stress and decision fatigue, especially for owner-operators managing both care delivery and business operations
- Lower tolerance for revenue leakage, insurance denials, and administrative waste that delay collections
- Limited ability to absorb short-term disruptions, such as staff turnover, payer policy changes, or temporary volume drops
For many solo and individual practices, prolonged financial strain accelerates tough decisions. Practices may delay upgrades, reduce services, or ultimately close or sell earlier than planned, not due to lack of clinical demand, but because the financial risk becomes unsustainable.
See how CERTIFY Health’s Practice Management System eliminates dental practice’s front-desk burnout with unified scheduling, intake, and eligibility workflows. Read the complete operations framework here: Practice Management System Guide
II. Challenges Faced by Group Dental Practices in the U.S.
As locations multiply and teams expand, operational cracks widen. What once worked for a single independent dental clinic often fails at scale, especially across multiple dental specialties.
Below are the most pressing challenges shaping group dental practice performance today.
1. Staffing Shortages That Disrupt Care Delivery
Staffing shortages remain one of the biggest threats to stability across group practices.
The impact is real:
- Scheduling conflicts due to limited hygienist or assistant availability
- Increased workload on remaining staff, accelerating burnout
- Inconsistent patient experience from site to site
When staffing gaps persist, practices risk follow-up loss, reduced chair utilization, and ultimately, revenue decline.
2. Financial Pressure From Revenue Leakage
Managing revenue at scale is hard. Group practices face compounding risks when RCM workflows are not standardized.
Key financial challenges include:
- Insurance denials due to inconsistent documentation
- Missed or incorrect perioperative and perio codes
- Incomplete claims scrubbing across locations
Without tight controls, even high-volume practices experience delayed payments and cash-flow strain, one of the hidden drivers behind dental practice closure in competitive markets.
3. Patient Experience Breakdown at Scale
Patients expect consistency. When one location delivers smooth care and another delivers friction, trust erodes quickly.
Group practices often struggle with:
- Disconnected scheduling systems causing appointment errors
- Weak patient identification and patient authentication across sites
- Poor continuity in follow-ups for specialty care or cosmetic surgery
When experience breaks down, patient loyalty drops, especially for long-term treatments in orthodontics or prosthodontics.
4. Technology Sprawl Without True Interoperability
Many group practices adopt new tools rapidly, but not always strategically. The result is a patchwork of systems that don’t talk to each other.
Common pain points include:
- Clinical data isolated from practice management systems
- Imaging, periodontal charting, and billing tools operating separately
- No unified dashboard to track performance across sites
Without interoperability, leadership cannot make timely decisions, and teams spend hours reconciling data manually.
Data trapped across disconnected systems kills efficiency in group dental practices. CERTIFY Health connects your PMS, EHR, and billing for seamless workflows. Full interoperability framework: Healthcare Interoperability Guide
5. Managing Multiple Dental Specialties Under One Roof
Group practices that offer multiple dental specialties gain reach, but also complexity.
Each specialty introduces unique needs:
- Orthodontics requires long-term treatment tracking and virtual mockups
- Endodontics demands precise documentation and fast referrals
- Pediatric surgery relies on seamless scheduling and caregiver communication
Without standardized workflows, specialty care becomes harder to manage, and outcomes suffer.
6. Financing Hurdles and Growth Risk
Expansion requires capital. For many groups, financing hurdles emerge when growth outpaces infrastructure.
Challenges include:
- Difficulty forecasting ROI for new locations
- Rising operational costs without corresponding efficiency gains
- Increased dependency on external funding or DSO partnerships
When financial strain combines with operational inefficiency, even established groups face tough decisions about consolidation or exit.
III. Challenges Faced by Multi-Location Dental Practices in the U.S.
Expanding a dental practice to multiple locations can unlock new patient volumes, specialty growth, and brand scale. But behind the promise of broader reach lies a set of operational, financial, and compliance challenges that many groups underestimate.
1. Regulatory and Credentialing Complexity
Growing beyond a single office means dealing with multiple sets of state licensing, facility permits, and insurance networks for each location. Every dentist, hygienist, and specialist must meet each jurisdiction’s regulatory standards.
- Practices must secure branch permits and state provider licenses for every location
- Credentialing with private payers and government networks can take 60–90 days per provider
- Improper credentialing can cost practices over $100,000 in lost revenue annually if not handled correctly
This administrative load is far more than a one-time task, it requires ongoing monitoring to ensure compliance and avoid costly fines.
2. Operational Fragmentation Across Sites
Each new office added to a group introduces another set of workflows: scheduling, billing, patient intake, staffing, and supply management. Without unified systems in place, these processes diverge from location to location.
Common outcomes include:
- Inconsistent patient experiences
- Redundant administrative tasks
- Confusion over standard operating procedures
Group practices may find that inefficiency multiplies with each added location unless uniform protocols are established early.
Modern patients expect digital scheduling and frictionless visits across multiple sites. CERTIFY Health delivers consumer-grade patient experience at scale. Check how: Ultimate Patient Experience Guide
3. Increased Financial Complexity
Financial management becomes more complicated as multi-location practices scale. Each new office adds:
- Additional payroll burdens
- Overhead costs for facilities and equipment
- Variability in cash flow timing across sites
When financial systems are not centralized, leadership loses visibility into which locations are thriving and which need support, slowing decision-making and undermining growth.
4. Insurance and Network Participation Barriers
Managing payer relationships at scale is no small task. Each location must:
- Maintain contracts with major payers
- Navigate variations in coverage policies
- Avoid insurance denials due to credentialing or billing inconsistencies
Failing to coordinate insurance participation centrally can lead to increased insurance denials and revenue leakage, which eat into profitability across the group.
5. Data Silos and Lack of Unified Systems
Many multi-location practices begin with independent systems at each office – different software, separate databases, and disconnected records. This siloed data restricts leadership’s ability to analyze performance, forecast trends, or proactively manage risk.
To scale effectively, multi-location groups need:
- Centralized patient and financial data
- Unified scheduling and RCM platforms
- Real-time dashboards for compliance and performance tracking
Without these, growth becomes harder to manage, not easier.
IV. Challenges Faced by Dental Support Organizations (DSOs)
1. Complex Integration of Clinical and Non-Clinical Operations
DSOs exist to unify functions that independent dentists traditionally handle on their own. But integrating clinical workflows with business operations across multiple locations isn’t simple.
Key integration challenges include:
- Aligning practice management protocols with centralized RCM and compliance systems
- Harmonizing scheduling, charting, and billing across different specialties
- Ensuring consistency in patient experience and follow-up
Without seamless integration, inconsistencies emerge, leading to operational bottlenecks, higher costs, and ultimately, loss of revenue that can jeopardize a practice’s viability.
2. Legacy Systems and Technology Fragmentation
Even for well-funded DSOs, technology often becomes a patchwork of best-of-breed tools that don’t communicate well. Multiple EHRs, practice management systems, and billing platforms create data silos that slow decision-making and obscure performance trends.
Common tech pitfalls include:
- Redundant data entry across platforms
- A lack of real-time interoperability
- Difficulty aggregating metrics across locations
This fragmentation diminishes the value of scale, erodes efficiency gains, and can lead to duplication of effort, missed claims, and cascading denials, all of which strain finances and contribute to practice closures.
3. Staffing and Workforce Optimization
DSOs promise standardized roles and centralized support, but scaling staff resources remains a challenge.
Key staffing issues include:
- Balancing workload across clinical and administrative teams
- High turnover in revenue cycle and front-office functions
- Specialty-specific support needs that aren’t evenly distributed
Even small imbalances in staffing scale dramatically across networks. When workflows break down due to understaffed teams or poorly matched skills, practices experience delayed appointments, billing errors, and patient dissatisfaction, all precursors to financial instability and potential closure.
4. Revenue Cycle Complexity and Insurance Friction
Large dental networks process high volumes of claims. While this gives leverage, it also heightens the risk of insurance denials and revenue leakage, especially when workflows aren’t tightly standardized.
Challenges include:
- Variability in payer rules across states and payers
- Multiple credentialing and re-credentialing timelines
- Limited visibility into denial causes across specialties or locations
Revenue leakage reduces operating capital. Over time, practices that cannot collect consistently find themselves unable to cover payroll, supplies, or lease commitments, a slow march toward closure.
Denials and delayed payments start at eligibility. CERTIFY Health closes revenue gaps for dental practices with automated RCM. Read Our: Healthcare Revenue Cycle Management Guide
5. Regulatory and Compliance Pressure
DSOs operate across multiple regulatory environments, each with evolving policy changes, credentialing requirements, and quality standards.
Challenges include:
- Tracking license renewals and provider eligibility across states
- Adapting to shifting telehealth and billing regulations
- Ensuring HIPAA, OSHA, and payer compliance consistently
Every compliance lapse risks fines, halted reimbursements, or audit liabilities. Cumulative penalties and interruptions can erode financial resilience, pushing practices closer to closure when margin buffers are thin.
6. Scaling Culture and Leadership Alignment
Growth can dilute organizational culture if it isn’t intentionally nurtured. DSOs that expand rapidly often struggle to maintain cohesion across leadership teams and clinical staff.
Key issues include:
- Divergent management styles across locations
- Uneven adoption of organizational values and best practices
- Leaders pulled in multiple directions without clear governance
Without unified culture and accountability, teams become disengaged, operations fragment, and quality declines, weakening patient trust and market position over time.
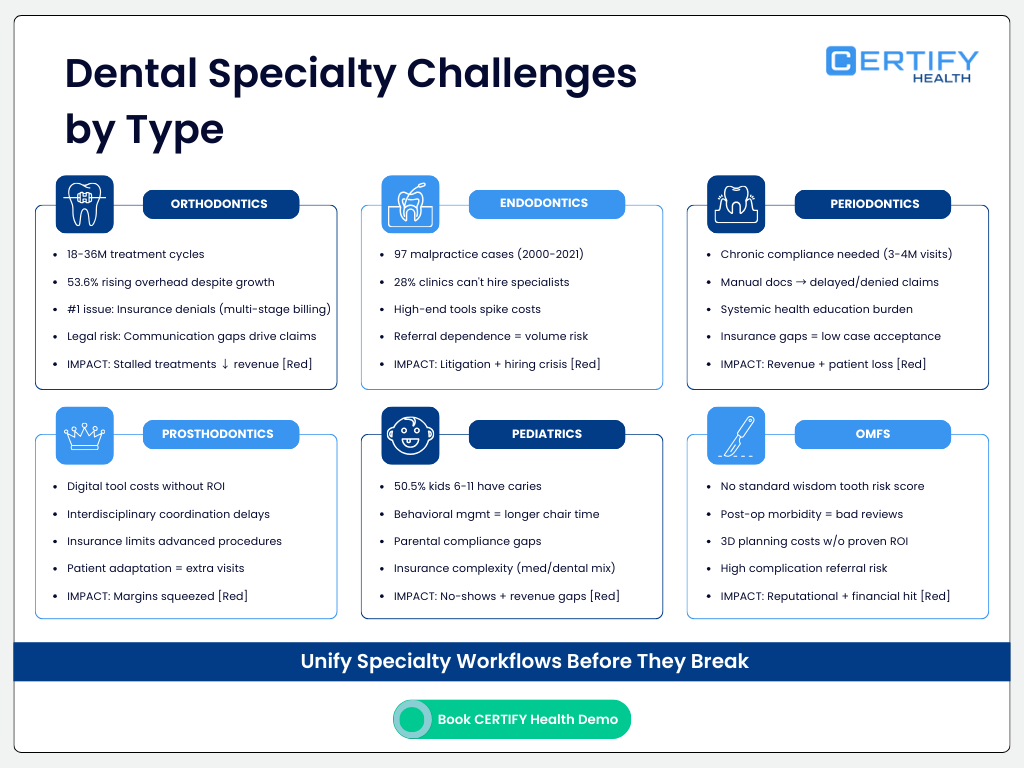
Unique Challenges Faced Everyday by Dental Specialties
I. Orthodontic Dental Specialty
Orthodontics sits at a unique intersection of healthcare, aesthetics, and long-term patient relationships.
While demand for orthodontic care remains strong, independent dental practices and independent dental clinics, group, multi-locations, and DSOs in the U.S. face mounting operational, financial, and organizational pressures that threaten sustainability if left unaddressed.
1. Long Treatment Cycles Heighten Operational Vulnerability
Orthodontic care is inherently long-term. Treatments often span 18–36 months, requiring repeated visits, ongoing documentation, and consistent patient engagement. For an independent dental practice, this creates operational strain that compounds over time.
Key operational challenges:
- Managing high visit volumes across extended treatment timelines
- Coordinating scheduling, adjustments, and follow-ups across multiple locations or chairs
- Maintaining accurate clinical and financial records over years, not weeks
When workflows rely on disconnected systems, separate tools for scheduling, clinical notes, billing, and patient communication, teams spend more time reconciling data than delivering care.
Why it matters:
Manual handoffs increase errors, slow throughput, and reduce chair utilization, directly impacting revenue and patient satisfaction.
Dental specialty workflows demand clinical-operational alignment. CERTIFY Health streamlines complex treatment coordination. Here’s how it works: Patient Management & Clinical Workflow Guide
2. Financial Pressure from Insurance Denials and Delayed Payments
Unlike general dentistry, orthodontics often involves multi-stage billing, extended payment plans, and prior authorizations, increasing exposure to insurance denials.
Common revenue challenges:
- Claims denied due to missing documentation or eligibility mismatches
- Delayed reimbursements across multi-year treatment cycles
- Inconsistent tracking of patient responsibility vs. payer responsibility
According to orthodontic industry surveys, over 53.6% of practices reported rising overhead costs, even during periods of production growth.
Why insurance denials hit orthodontics harder:
- Longer treatment durations mean more chances for eligibility changes
- Pediatric and orthodontic benefits often have lifetime caps
- Manual claim workflows increase denial risk
3. Heightened Legal and Compliance Risk in Orthodontics
Orthodontics carries unique medico-legal exposure due to:
- Long treatment timelines
- High aesthetic expectations
- Perceived outcome subjectivity
A 2025 review published in MDPI found that many orthodontic malpractice claims stem from communication gaps and expectation misalignment rather than technical clinical errors.
Common risk drivers:
- Inconsistent documentation over long care periods
- Poor tracking of informed consent updates
- Lack of centralized patient communication records
For U.S. dental practices, especially independent ones, compliance risk increases when records are spread across systems or manually maintained.
4. Patient Compliance Remains a Core Barrier
Effective orthodontic outcomes depend heavily on patients following instructions, managing removable appliances, maintaining hygiene, and attending every adjustment.
According to the Journal of Clinical Pediatric Dentistry study:
- Orthodontists reported poor oral hygiene and bracket breakage as common challenges in children, often undermining treatment progress.
In adult patients, irregular attendance was flagged as a major obstacle.
These human factors, while clinical, are shaped by practice management and patient engagement strategies.
Impact:
When patients fail to cooperate or attend appointments consistently, orthodontic treatments stall. This not only lengthens treatment time but also drives up costs and decreases patient satisfaction, threatening both revenues and referrals.
5. High-Quality Patient Education Is Hard but Essential
Orthodontists participating in a research shared that patients frequently worry about:
- Treatment cost
- Length of therapy
- Potential relapse after treatment
Patient concerns about aesthetics and long-term retention can result in resistance to recommended plans, especially when innovations like digital aligners or intraoral scanners are introduced without adequate context.
Why this is a challenge:
When patients don’t understand the value or rationale behind treatment plans or technology, adherence drops and treatment outcomes can falter. This places additional burdens on staff time for counseling and prolongs clinical cycles.
II. Endodontics Dental Specialty
Endodontics, the dental specialty focused on diagnosing and treating diseases of the dental pulp and root canal system is both highly skill-dependent and deeply intertwined with broader clinical and business realities of modern dentistry.
Below are the most pressing and unique challenges shaping Endodontic care delivery in the United States.
1. High Stakes of Technical Precision and Litigation Risk
Unlike many dental treatments, root canal therapy demands exceptional technical execution: the canal anatomy is variable, instruments are delicate, and procedural errors can lead to nerve injury or infection. As a result, endodontics carries a notable risk of malpractice claims.
- Between 2000 and 2021, U.S. courts reviewed 97 endodontic malpractice cases related to root canal therapy and similar procedures. The annual average was 4.41 cases per year.
- Of those, 43 of the 95 analyzed cases involved pre-procedural errors, like delayed diagnosis or missing informed consent.
- Certain complications, especially post-procedural infections and paresthesia (nerve damage), resulted in higher plaintiff success rates than other claims.
These malpractice pressures don’t just lead to legal exposure, they elevate operating costs through higher insurance premiums, potential payouts, and defensive practice patterns. Together, this increases the financial risk profile of an endodontic practice, making some specialists more cautious about growth, hiring, or investment.
2. Shortage of Trained Endodontic Specialists and Skill Gaps
Advanced endodontic care requires years of training beyond general dentistry. Market research consistently highlights a shortage of highly trained endodontists and persistent training gaps among clinicians:
In global market surveys, about 28% of clinics identify difficulty recruiting skilled endodontic professionals as a top barrier.
In the U.S., this shortage means that general practitioners often handle complex root canal treatments, which can increase variability in outcomes and risk. The lack of specialists can also bottleneck referral networks, reducing endodontists’ ability to expand practices or maintain manageable patient loads.
3. Rising Treatment Costs and Limited Patient Access
Endodontic care increasingly involves sophisticated imaging and instruments (CBCT, nickel-titanium rotary systems, operating microscopes) that improve outcomes but come with steep price tags.
- High-end equipment and advanced procedural tools significantly increase operating costs, a challenge shared with other dental specialties such as prosthodontics and orthodontics.
Patients facing higher out-of-pocket costs may decline conservative root canal therapy in favor of extractions or implants. This reduces patient volume, lowers revenue, and weakens long-term case continuity, particularly for practices that rely on referral networks rather than broad patient acquisition campaigns.
4. Evolving Technology and Training Barriers
Digital workflows and new diagnostic technologies are rapidly reshaping how endodontic care is delivered. Innovations like guided endodontics, AI diagnostics, and laser-assisted systems enhance precision and efficiency.
Yet, widespread adoption lags in many practices due to:
- Training gaps among clinicians
- High capital investment barriers
- Workflow disruption during implementation
When practices delay adopting modern tools or fail to integrate them with existing systems, they can lose efficiency and competitive edge. This is especially relevant when neighboring practices offer “single-visit root canal” or digital scanning as patient experience differentiators.
5. Patient Compliance and Perception Issues
Root canal treatments often carry anxiety and negative perceptions among patients, which can lead to:
- Missed appointments
- Refusal of dentist-recommended treatments
- Preference for extraction or implant alternatives
These behavior patterns directly impact revenue and case continuity. When patients disengage mid-treatment, it increases the risk of retreatment, infection, and even malpractice exposure if outcomes are suboptimal.
6. Referral Channel Dependence Adds Business Vulnerability
Endodontists typically depend on referrals from general practitioners rather than direct patient walk-ins. This referral model creates business risk:
- Any decline in GP referrals, due to practice consolidation, closed practices, or DSO realignment, translates quickly into lost case volume.
- Endodontic practices with weak referral ties struggle to maintain steady patient inflow, especially in saturated urban markets.
Without a diversified patient base, volatility in referral networks can directly undermine financial stability and, in extreme cases, contribute to dental practice closure.
7. Compliance, Documentation, and Communication Demands
According to the litigation analysis, insufficient pre-procedural communication, including gaps in informed consent, accounted for approximately 27.4% of malpractice allegations.
Accurate, timely documentation and shared decision-making with patients are not just good practice, they are essential risk mitigators. Weak systems for capturing consent, warnings, or clinical rationale invite legal exposure and increase operational burden.
Endodontic practices that lack robust digital records or standardized communication protocols can find themselves unprepared for audits, insurance reviews, or legal inquiry, which further erodes stability.
III. Periodontics Dental Specialty
Periodontics, the dental specialty focused on gum health and supporting structures of teeth, occupies a vital place in overall oral and systemic health. Yet unlike general dentistry, periodontics contends with complex disease biology, costly technology demands, patient compliance issues, and evolving regulatory expectations.
1. Complexity of Disease and Diagnostic Uncertainty
Periodontal disease isn’t a single condition, it ranges from mild gingivitis to aggressive periodontitis. Accurate diagnosis requires careful clinical evaluation and often advanced imaging.
However:
- Clinical signs can be subtle or masked by other conditions
- Disease progression varies widely between patients
This complexity increases diagnostic uncertainty, requiring practitioners to integrate clinical findings with radiographic evidence, a workflow that often stretches both time and cognitive attention.
If diagnostic systems are siloed or inefficient, practices waste clinical time and increase chances of misdiagnosis, a risk that translates directly to patient dissatisfaction and erosion of trust.
2. Reliance on Patient Compliance in Long-Term Care
Periodontal treatment is not a “one and done” procedure, effective therapy requires:
- Regular maintenance visits (often every 3–4 months)
- Rigorous home care by patients
- Lifelong periodontal monitoring
Patient compliance challenges include:
- Failure to return for scheduled maintenance
- Poor oral hygiene habits
- Misunderstanding the chronic nature of the disease
Noncompliance undermines clinical outcomes and increases the likelihood of recurrent disease. Practices then spend more time managing complications rather than delivering planned care, which frustrates both clinicians and patients.
This loop weakens patient loyalty and can shrink predictable revenue streams when follow-up visits are missed.
3. Integration of Technology Into Workflow
While technology like CBCT and digital periodontal charting has transformed diagnosis and treatment planning, many practices struggle to integrate these tools into everyday workflows.
Technology adoption is uneven and often limited by:
- Insufficient training and support
- Fragmented software systems that do not communicate
- Disruption during implementation phases
In other words, the practice may have access to advanced tools, but if they aren’t embedded in efficient clinical and administrative processes, the benefits are muted. Patients may face scheduling delays, longer chair times, or inconsistent treatment documentation, which impacts patient experience and outcomes.
4. Linking Periodontal Disease to Systemic Health
Periodontitis has been linked to systemic conditions like diabetes and cardiovascular disease. Clinicians confront the challenge of:
- Educating patients on complex disease interrelationships
- Collaborating with medical peers
- Navigating care boundaries without overstepping clinical scope
Despite evidence that periodontal health affects systemic outcomes, communicating this in ways that motivate patients remains difficult. When patients view periodontal disease as “minor gum issues,” they may undervalue treatment, undermining retention and compliance.
5. Regulatory and Documentation Burden
Periodontics often involves:
- Detailed charting
- Periodontal probing and documentation
- Treatment plan consent
- Claims that reflect complex interventions
This highlights the importance of structured documentation for both clinical decision-making and compliance with payer requirements (e.g., medical necessity, probing depth records, attachment loss). When documentation systems are manual or disconnected from clinical records, claims are more likely to be:
- Delayed
- Denied
- Underpaid
Practice teams then spend disproportionate time on rework rather than new patient care.
Repeated revenue cycle stress can reduce operating margins and contribute to financial vulnerability, especially for smaller clinics with limited administrative bandwidth.
6. Patient Financial Barriers and Insurance Complexity
Many periodontal therapies are not fully covered by dental insurance, leaving patients to shoulder higher out-of-pocket costs. This affects:
- Case acceptance
- Treatment sequencing
- Patient retention over long treatment courses
When practices cannot easily verify eligibility or predict patient responsibility, treatment plans may be postponed or rejected, decreasing revenue predictability and practice utilization.
For independent periodontal clinics without robust revenue cycle tools or real-time eligibility verification, this financial friction compounds operational stress.
IV. Prosthodontic Dental Specialty
Prosthodontics, the dental specialty focused on restoring oral function and aesthetics through prostheses like dentures, crowns, and implants, sits at the intersection of artistry and science.
Below are the top challenges shaping prosthodontic practice today.
1. Patient Adaptation and Psychological Factors
Getting patients comfortable with removable prostheses or complex fixed restorations isn’t only a mechanical issue, it’s behavioral. Many patients struggle with:
- Speech changes
- Salivary flow adjustments
- Psychological acceptance of prosthetic appliances
Adaptation challenges often necessitate extra appointments for adjustments and counseling. This ongoing care increases service time without corresponding reimbursement, which squeezes margins and can make some practices financially unsustainable.
2. Integrating Digital Workflows and Technology
Digital dentistry, including CAD/CAM systems, 3D scanning, and digital design software, offers powerful tools for precision and customization. However, many prosthodontic practices face significant technology adoption barriers:
- High upfront costs for digital fabrication systems
- Software limitations for complex cases or anatomical irregularities
- Training demands for clinicians and support staff to use digital tools effectively
For example, clinical reports show that digital workflows often must be combined with conventional techniques for complex defects because software tools still have limitations.
These barriers slow workflow efficiency and reduce return on investment (ROI), contributing to stress on practice finances, especially in smaller clinics.
3. Education & Continuous Professional Development
Prosthodontics evolves rapidly, from new materials science to digital design methods. Keeping clinicians and staff fully trained requires ongoing investment:
- Costs and time for continuing education
- Downtime during learning curves
- Variable payback on new competencies
Clinics that struggle to keep pace with new protocols and technologies risk falling behind patient expectations and competitive offerings, which can contribute to declining market share and financial stress
4. Patient Access, Cost Barriers & Insurance Limitations
Prosthodontic care is often perceived as elective or high-cost dental care, leaving many patients facing significant out-of-pocket expenses. Insurance coverage for advanced prosthetic services is often limited or inconsistent, especially for procedures beyond basic removable dentures.
This dynamic leads to:
- Reduced case acceptance
- Longer treatment intervals
- Patients electing less comprehensive care
Lower case acceptance directly impacts revenue streams. For specialty practices that rely heavily on prosthetic services, this financial pressure can erode sustainability and contribute to closures when practice volumes decline.
5. Interdisciplinary Coordination & Complex Treatment Planning
Many prosthodontic treatments, especially implant-supported restorations, rely on close coordination with surgeons, periodontists, and other specialists. Achieving predictable outcomes requires synchronized treatment sequencing, which can be hard to manage operationally.
Lack of coordination can cause delays, increase lab costs, and elevate risk for complications, all of which add financial and clinical burden.
V. Pediatric Dental Specialty
Pediatric dentistry plays a crucial role in building lifelong oral health by caring for infants, children, adolescents, and patients with special needs. However, delivering effective pediatric dental care brings a distinct set of clinical, behavioral, operational, and financial challenges.
1. Early Childhood Caries: A Persistent Epidemic
Children experience some of the highest rates of untreated dental disease among age groups.
According to research:
- About 50.5 % of children aged 6–11 years have experienced dental caries (treated or untreated).
- About 53.8 % of adolescents aged 12–19 years had experienced dental caries in either primary or permanent teeth (treated or untreated).
These figures illustrate that early childhood caries remains a prevalent and chronic problem in pediatric dentistry. High caries burden drives:
- Increased restorative workload
- Elevated preventive care demands
- Greater need for sedation or behavior management
Clinically, this creates long chair times and complex treatment planning, which in turn increases operational costs.
2. Behavioral Management & Communication Barriers
Children don’t respond to dental treatment the same way adults do. Fear, anxiety, and limited ability to follow instructions challenge pediatric dentists daily.
Common issues include:
- Fear of dental visits and needle anxiety
- Difficulty cooperating during exams and procedures
- Miscommunication between clinician, child, and parent/guardian
These challenges require clinicians to spend more time on behavior guidance per visit, lengthening appointments and reducing the number of patients that can be seen in a day. Inefficient scheduling and longer chair time contribute directly to rising overhead and can strain revenue sustainability in smaller practices.
3. Prevention vs. Treatment: Finding the Balance
Pediatric practices know that prevention is key, yet turning preventive advice into routine behavior for families is difficult.
Common preventive challenges include:
- Low adherence to brushing and flossing
- Continued consumption of sugary snacks and beverages
- Irregular dental visits influenced by caregiver priorities
The burden of preventive counseling often falls on the dentist and their team, diverting time from restorative care. When prevention fails and disease progresses, treatment demands escalate, adding stress to both clinicians and practice finances.
4. Special Needs Patients Require Tailored Protocols
Caring for patients with special healthcare needs (e.g., autism, cerebral palsy) requires:
- Additional time for communication
- Adaptive behavior guidance
- Modified clinical protocols
These patients often require extended appointments and heightened safety measures. Practices without dedicated training or resources struggle to meet these needs efficiently, which can reduce practice throughput and increase staff stress.
5. Workforce and Training Gaps
Delivering effective pediatric dentistry demands specific competencies not typically covered in general dental education alone. Challenges include:
- Staff turnover and training gaps in behavior management techniques
- Limited access to continuing education in pediatric sedation, trauma care, or special needs dentistry
- Difficulty recruiting team members who are comfortable working with children
When staff lacks confidence or skill, the practice experiences workflow bottlenecks, reduced capacity, and greater burnout, all of which erode operational resilience.
6. Sedation & Anxiety Management Considerations
Some pediatric dental procedures require sedation or advanced anxiety control techniques.
However:
- Regulatory requirements for sedation vary by state
- Additional staff training and monitoring equipment are required
- Risk management increases practice liability
These factors increase overhead and complicate scheduling, especially in smaller independent pediatric dental practices that may not have access to full anesthesia support.
7. Insurance Complexity and Reimbursement Challenges
Pediatric dental care is often billed to both dental and medical payers for preventative services. Coverage can vary widely, leading to:
- Confusion over benefit limits
- Frequent verification requirements
- Denials due to coding issues
Payer complexity increases administrative load and slows cash flow. For smaller pediatric clinics, prolonged claims processing or insurance denials can create revenue gaps that threaten financial sustainability.
8. Parental Expectations and Compliance
Parents play a critical role in the success of pediatric dental care. However, conflicting expectations and non-adherence complicate treatment:
- Caregivers may resist behavior guidance recommendations
- Parents may delay follow-up care due to costs or scheduling conflicts
- Misalignment between clinical goals and family expectations slows progress
This dynamic requires extra time for education and follow-up, which limits the number of patients a practice can manage effectively.
9. Technology Adoption & Workflow Integration
While advanced imaging, digital charting, and behavioral tools can improve care quality, pediatric practices face barriers to adoption:
- High upfront costs for child-friendly digital tools
- Staff training burdens
- Integration challenges with existing systems
Smaller practices often struggle to justify technology investments without clear ROI, resulting in continued reliance on manual workflows that hamper efficiency.
10. Population Health and Access Disparities
Pediatric dental needs are unevenly distributed across socio-economic lines. Children from underserved communities experience higher untreated caries rates and lower access to preventive care. Practices serving high-need populations often face:
- Higher no-show rates
- Greater uncompensated care burden
- Increased demand for extensive restorative care
This dynamic affects both patient mix and revenue predictability and can pressure a practice’s financial viability.
VI. Oral & Maxillofacial Surgery (OMFS)
Unlike many clinical dental procedures, OMFS integrates surgical precision, advanced anatomy knowledge, systemic risk management, and cutting-edge technology, all in high-stakes environments. These demands create unique practice challenges that affect outcomes, patient experience, and, ultimately, a practice’s financial stability and longevity.
1. Surgical Difficulty and Risk Prediction for Third Molar Extractions
Impacted wisdom tooth surgery isn’t always straightforward, complexity scales with anatomy, tooth position, and proximity to nerves. A systematic review of extraction difficulty scales found that multiple indices exist, but no universally accepted pre-operative scoring system is used broadly.
This means:
- Surgeons must rely on experience and judgment rather than standardized risk tools
- Unexpected complications (nerve injury, excessive bone removal, sinus involvement) are more common
- Operating times and postoperative morbidity can be hard to predict
For practices without strong triage and referral pathways, this leads to higher complication rates, dissatisfied patients, and increased postoperative care burdens that can weigh on profitability.
2. Multifaceted Clinical Controversies Increase Diagnostic Burden
A comprehensive multidisciplinary review of OMFS highlights that several high-impact conditions remain controversial, including:
- Third molar management
- Medication-related osteonecrosis (MRONJ)
- Optimal anesthesia techniques
- Timing and technique for orthognathic surgery
- Infection vs. surgical management decisions
This emphasizes that no clear consensus exists for many standard practice areas, forcing clinicians to rely on individualized judgment or institutional protocols.
In practice, this results in:
- Greater documentation burden
- Higher need for informed consent discussions
- More second opinions and potential referral to other surgeons
These factors can reduce operative throughput and generate patient uncertainty, both negative for practice growth.
3. Integration of Advanced Technologies and Digital Planning
Modern OMFS increasingly relies on advanced digital tools like 3D imaging, virtual surgical planning, intraoperative navigation, CAD/CAM guides, and potentially robotics to enhance precision. However, these technologies come with hurdles:
- High acquisition and maintenance costs
- Steep training requirements for surgeons and support staff
- Workflow disruptions during implementation
Though promising, many innovations (especially robotic systems) are not yet validated with robust clinical evidence, and their practical value in routine maxillofacial surgery remains under investigation.
For many practices, the cost of technology adoption without clear revenue return, combined with the need to maintain productivity, creates a barrier to sustainable investment and can widen the gap between well-capitalized group practices and smaller independent surgeons.
4. High Postoperative Morbidity and Patient Experience Pressures
Even the most routine OMFS procedures, like wisdom tooth removal, commonly produce pain, swelling, and temporary disability (e.g., trismus). Postoperative morbidity persists despite advances in analgesia and aftercare.
Surgical recovery impacts patient perceptions:
- Poor healing or pain can lead to negative reviews and reputational risk
- Unsatisfactory outcomes may require extra follow-ups, eating into clinician time
- Complications such as alveolar osteitis (dry socket) remain notable postoperative events in oral surgery
When practices struggle with patient experience and postoperative burden, retention and referral patterns decline, and booking new patients becomes more challenging.
CERTIFY Health: Unified Solutions for Modern Dental Specialty Practices
CERTIFY Health is a modern, unified healthcare platform designed for US dental practices. From a single-location independent dental clinic to a fast-growing group dental practice or enterprise-level dental support organization (DSO), CERTIFY Health adapts to how your practice operates today and how it needs to grow tomorrow.
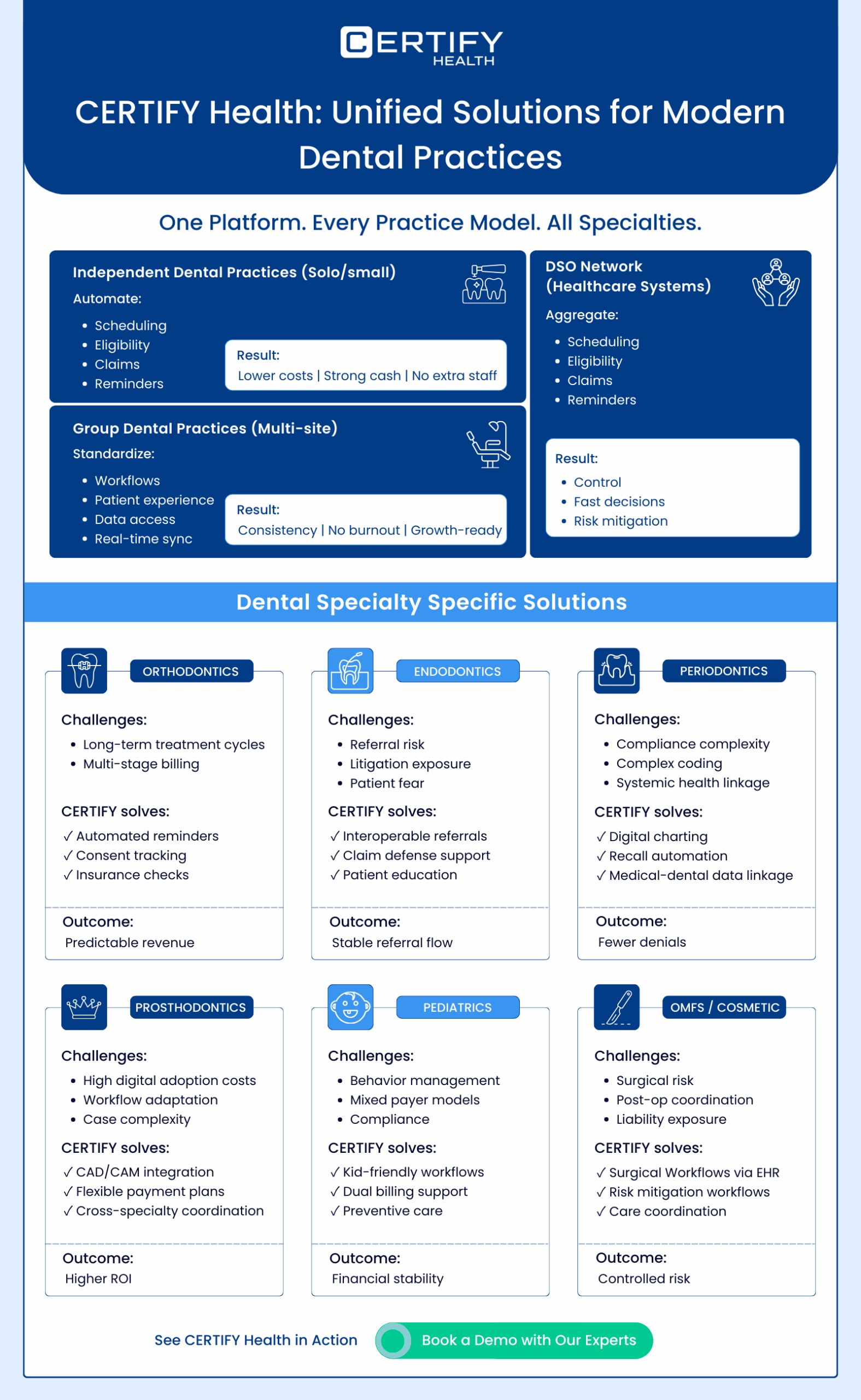
Built to Support Every Practice Model
Independent Dental Practice & Independent Dental Clinic
For the independent dental practice, survival depends on efficiency, collections, and patient loyalty, without adding staff. CERTIFY Health automates scheduling, reminders, eligibility checks, and claims scrubbing, helping small teams do more with less.
Integrated patient identification and patient authentication reduce front-desk friction, while unified RCM protects margins against rising insurance denials and financing hurdles.
Result: lower overhead, stronger cash flow, and operational control without enterprise complexity.
Group Dental Practice
As a group dental practice expands, consistency becomes the challenge. CERTIFY Health standardizes workflows across providers and locations while preserving clinical autonomy.
Centralized practice management, shared patient management, and real-time interoperability prevent follow-up loss and data silos, ensuring patients receive the same experience at every site.
Result: scalable growth without operational chaos or staffing burnout.
Dental Support Organization (DSO)
For a dental support organization, visibility and control define performance. CERTIFY Health delivers a powerful DSO dashboard that aggregates scheduling, collections, denials, and patient engagement across all locations.
Credentialing, compliance tracking, and RCM optimization happen centrally, while FaceCheck ensures secure patient authentication at scale.
Result: enterprise-level oversight, faster decision-making, and reduced risk of revenue decline across the network.
One Platform, All Dental Specialties
CERTIFY Health is purpose-built to support every dental specialty, including Orthodontics, Endodontics, Periodontics, Prosthodontics, Pediatric surgery, Cosmetic surgery, and Oral & Maxillofacial Surgery.
1. Orthodontics
Orthodontics faces extended treatment timelines, multi-stage billing, compliance gaps, and frequent follow-up loss.
CERTIFY Health offers:
- Automated practice management calendars track long-term plans and prevent scheduling conflict.
- Automated reminders through patient experience reduce no-shows and improve compliance.
- RCM tools verify eligibility and prevent insurance denials tied to staged claims
- Patient management centralizes consent and communication records to reduce legal exposure
- Interoperability and FaceCheck ensure seamless referrals and accurate patient authentication
Outcome: predictable cash flow, higher retention, and protection from revenue decline.
2. Endodontics
Endodontics depends heavily on referrals while facing litigation risk and patient hesitation due to financing hurdles.
CERTIFY Health offers:
- Interoperability unifies CBCT imaging and procedure notes across dental health systems
- Automated referral tracking in practice management prevents follow-up loss
- RCM simplifies complex claims and out-of-pocket scenarios
- Secure patient identification with FaceCheck reduces billing errors
- Education via patient experience portals improves treatment acceptance
Outcome: stable referrals, defensible documentation, and sustained revenue for every independent dental practice or group dental practice.
3. Periodontics
Periodontal specialists struggle with complex periodontal charting, payer variability, and long-term maintenance adherence.
CERTIFY Health offers:
- Digital charting tools in CERTIFY Health’s patient management software support seamless periodontal assessments.
- RCM validates documentation to avoid denials tied to probing depth records
- Personalized recall workflows in patient management reduce follow-up loss
- Interoperability links systemic health data to support education and medical necessity
- A unified DSO dashboard ensures consistency across locations
Outcome: stronger compliance, fewer denials, and reduced risk of dental practice closure.
4. Prosthodontics
Prosthodontics encounters digital workflow friction, adaptation challenges, and reimbursement limits.
CERTIFY Health offers:
- CAD/CAM integration and virtual mockups within practice management
- Cross-specialty coordination through interoperability for implant planning
- Visual education tools in patient experience drive case acceptance
- RCM manages payment plans and complex claims to overcome financing hurdles
- Accurate patient authentication prevents billing discrepancies
Outcome: higher ROI on technology investments and smoother high-value case execution.
5. Pediatric Dentistry and Pediatric Surgery
Pediatric-focused practices, including pediatric surgery, face behavior management issues, sedation protocols, and payer complexity.
CERTIFY Health offers:
- Child-friendly patient experience tools reduce anxiety and no-shows
- Sedation and protocol tracking via practice management
- Dual medical–dental billing managed through RCM to prevent insurance denials
- Risk-based reminders in patient management for preventive care
- Family-friendly FaceCheck simplifies patient identification
Outcome: balanced schedules, safer care delivery, and financial stability even in underserved regions.
6. Oral & Maxillofacial Surgery and Cosmetic Surgery
OMFS and cosmetic surgery demand precision, liability protection, and cost control.
CERTIFY Health offers:
- CERTIFY Health integrates with EMR/EHRs for full interoperability, ensuring patient data flow where it’s needed, supporting 3D surgical planning workflows.
- Predictive scheduling tools in practice management reduce complications
- RCM scrubs anesthesia and surgical claims to avoid denials
- CERTIFY Health empowers practices to improve care coordination through robust communication solutions, enabling continuous support and timely interventions.
- Secure patient authentication protects against liability exposure
Outcome: controlled risk, reliable revenue, and operational resilience for multi-site DSOs.
Join CERTIFY Health at Yankee Dental Congress 2026
Post-COVID, dental facilities face relentless strain: staff shortages, manual workflows slowing patient flow, revenue leaks from eligibility errors, and inconsistent experiences across sites. These aren’t effort issues, they’re systemic gaps unaddressed by fragmented tools.
CERTIFY Health changes that.
See us at Yankee Dental Congress 2026
Date: Jan 29–31, 2026
Location: Thomas M. Menino Convention & Exhibition Centre, Boston
Booth No.: #830
Experience live demos of unified workflows that automate intake, verify insurance instantly, engage patients seamlessly, and stabilize revenue, scaling from solo practices to DSOs without added complexity.
Stop by our Booth for 15 minutes of real insight.
Turn Dental Practice Pressure into Performance
CERTIFY Health helps every dental specialty transform operational strain into a competitive advantage.
To understand how we fix Dental Specialty Challenges & Prevent Dental Practice Closures, read next:
Or
Schedule your demo today and future-proof your practice.
You Might Also Like to Read: