Table of Contents
Many find MIPS reporting confusing and full of government jargon and you might too.
Every year, countless healthcare providers stare at acronyms, complex rules, and submission deadlines, wondering: How does MIPS reporting work?
The good news is that MIPS isn’t as intimidating as it seems once you break it down step by step. And if you do it right, you are not just avoiding penalties… you are unlocking powerful Medicare incentives that reward you for delivering better care.
In this post, we’ll walk you through the essentials of the Merit-Based Incentive Payment System—better known as MIPS. By the end, you’ll know exactly what MIPS is, how MIPS reporting works, why it’s tied to your Medicare Part B payments, and how to turn the system into an opportunity instead of a headache.
What Is MIPS in Healthcare?
Let’s start at the top.
What is MIPS in healthcare?
In plain English: It’s a Medicare program created to transform the way clinicians get paid. Instead of rewarding quantity (number of visits or procedures), MIPS ties payments directly to healthcare quality, outcomes, and efficiency.
Think of it this way:
The higher your performance, the more Medicare incentives you earn.
The worse your performance, the greater the likelihood of facing a payment penalty.
MIPS is part of Medicare’s Quality Payment Program (QPP), which offers two participation paths: standard MIPS reporting or joining an Alternative Payment Model (APM). Most clinicians start with MIPS but can later expand into MIPS APMs like bundled payments or Accountable Care Organizations (ACOs), depending on practice goals.
So, if you’ve ever asked, “What is MIPS reporting?”
MIPS reporting is essentially how Medicare evaluates your performance and calculates whether you get bonuses or penalties on your MIPS Medicare Part B claims.
Why Does MIPS Reporting Matter?
You might be thinking: All this paperwork for some score, why bother? Here’s the reality:
- Financial impact: Your composite performance score directly affects your reimbursement. Bonus or penalty, it all comes down to how well you report.
- Professional growth: MIPS forces practices to adopt best practices that improve patient outcomes and operational efficiency.
- Long-term readiness: MIPS prepares you for the inevitable shift toward value-based care, where success depends on quality, not just volume.
By embracing MIPS today, you are not just chasing incentives, you are safeguarding your practice’s financial health for tomorrow.
MIPS 2025 Penalty Tiers
| MIPS Score (Composite Performance Score) | Penalty on Medicare Part B Payments | Impact Description |
|---|---|---|
| 75 points or above | None (0%) | Safe zone—no penalty applies |
| 19 to 74 points | Up to -8.99% (sliding scale) | Minor to moderate payment cuts |
| 0 to 18.75 points | Full -9% penalty | Maximum reduction; steepest loss |
Breaking Down the Four MIPS Performance Categories
TL;DR – 4 MIPS Performance Categories
- Quality: Monitor and document patient care results, including preventive screenings and chronic condition management.
- Improvement Activities: Show efforts to boost care coordination & patient safety
- Promoting Interoperability: Use certified EHRs for secure data sharing & e-prescribing
- Cost: CMS auto-calculates from claims; smart resource use improves your score
MIPS reporting revolves around four weighted categories. These categories combine into your composite performance score (CPS), which determines your Medicare payment adjustments.
1. Quality
This is all about clinical quality reporting, tracking how you are delivering care from preventive screenings to chronic condition management. Your choice of quality measures matters because it demonstrates the value you bring to patient health.
2. Improvement Activities
These are tangible efforts like strengthening care coordination, implementing patient safety checks, or improving patient engagement. Strong performance here improves your ability to adapt to complex care environments.
3. Promoting Interoperability
Here’s where you leverage technology. Using certified EHR systems (Certified EHR Technology – CEHRT) is not optional, it’s a must. This category looks at how effectively your systems share patient health data to improve communication and streamline care.
4. Cost
Yes, cost efficiency counts. Medicare automatically calculates cost measures from claims, so no extra reporting is required. But your strategic decisions around case management and resource use heavily influence this score.
Together, these categories create the formula for success in MIPS reporting. Balance is key, but understanding category weights can help you prioritize for max impact
Step-by-Step Guide to MIPS Reporting
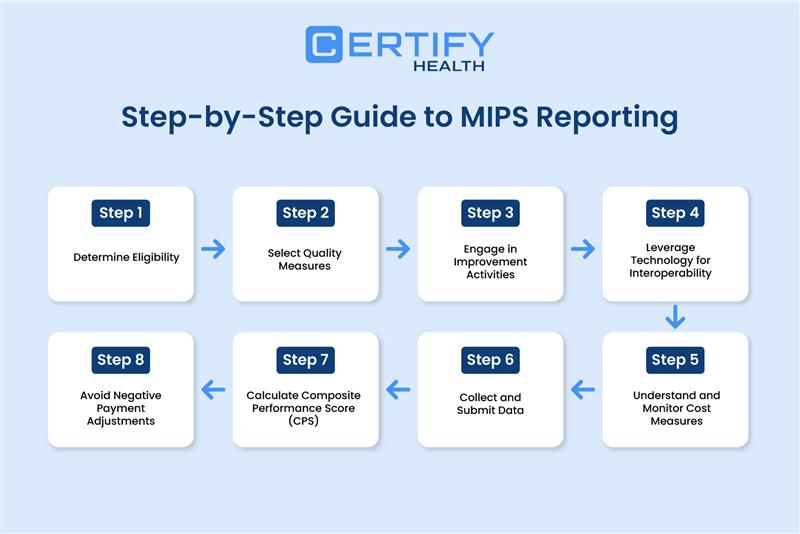
TL;DR – MIPS Reporting Made Simple
- Check Eligibility: First things first—check if you qualify. (>$90K Part B billing, 200+ patients/services).
- Pick Quality Measures: Choose specialty-relevant metrics for meaningful reporting.
- Collect Data: Use EHR (eCQMs), claims, registries, and CAHPS surveys.
- Do Improvement Activities: Document initiatives that boost outcomes & engagement.
- Promote Interoperability: Use certified EHRs for secure data sharing & e-prescribing.
- Monitor Costs: CMS auto-calculates; smart referrals & resource use improve scores.
- Submit Data Early: Avoid last-minute stress; report consistently.
- Calculate CPS: Composite score determines bonus or penalty.
- Stay Above Threshold: High scores = bigger Medicare incentives.
Think of this section as the GPS for your Medicare journey.
1. Determine Eligibility
Who is eligible for MIPS?
You’re eligible for MIPS if your Medicare Part B billing > $90,000, or if your practice treats more than 200 patients or provides 200+ covered services in a year—basically, if your practice hits these milestones, MIPS applies to you.
2. Select Quality Measures
Zero in on the quality measures that really match your specialty—this way, your reporting is meaningful and actually reflects the care you provide.
How We Collect Measures?
- eCQMs: Pulled directly from your EHR data.
- CQMs: Set of quality measures (including eCQMs).
- QCDR Measures: Specialty-focused or patient-reported measures from qualified registries.
- Medicare Part B Claims: Measured based on submission of Part B claims.
- CAHPS for MIPS: Quality related feedback gathered through surveys.
3. Engage in Improvement Activities
Document activities that boost outcomes or streamline processes. Examples: care coordination strategies, advanced training programs, and patient self-management support.
4. Leverage Technology for Interoperability
This focuses on demonstrating improved care by enabling secure electronic record sharing, including health information exchange and e-prescribing.
Pro Tip: With CERTIFY Health’s integrated health platform, practices streamline data sharing, enable secure patient access, and close the loop on care coordination, all while staying PI (Promoting Interoperability) compliant.

5. Understand and Monitor Cost Measures
Cost measures are automatically calculated by CMS from your Medicare claims, so you don’t need to submit anything extra. That said, they still require your attention.
Your referral patterns, treatment decisions, and resource use all impact your cost score.
6. Collect and Submit Data
Submissions can be done through registries, claims, or electronic reporting tools. Don’t wait until the end of the year, collect as you go to minimize stress.
7. Calculate Composite Performance Score (CPS)
Your final CPS is a blend of all four MIPS performance categories. This score determines if you’ll see a bonus or risk a negative payment.
8. Avoid Negative Payment Adjustments
Stay above the minimum performance threshold. The higher you score, the bigger your slice of the Medicare incentives pie.
Additional Participation Through MIPS APMs
If you are ready to level up, explore MIPS APMs. These models blend MIPS requirements with innovative care approaches.
- Alternative Payment Models (APMs): these programs reward practices that provide high-quality care while keeping costs under control, offering incentives for smarter, value-based care.
- Examples include advanced bundles and joining ACO healthcare groups.
- Benefits? More revenue opportunities, stronger networks, and improved systems for managing high-risk populations.
Participation in MIPS reporting doesn’t prevent you from joining APMs, it enhances your ability to maximize rewards.
MIPS vs APM – A Side-by-Side Comparison
| Aspect | MIPS (Merit-based Incentive Payment System) | APM (Alternative Payment Model) |
|---|---|---|
| Program Structure | You are evaluated based on Quality, Cost efficiency, Improvement Activities, & PI. | Value-oriented model tying payments to outcomes and efficiency; often involves upside/downside risk |
| Reporting Mechanism | Clinicians submit data and earn a composite score; influences payment adjustment (~±9%) | Participants often bypass separate reporting; performance is tracked via the APM structure itself |
| Risk & Reward | Low-to-moderate risk—bonuses or penalties based on scoring | Higher risk—participants assume financial risk but can earn incentive payment (e.g., 5%) |
| Use of EHR (PI requirement) | Reporting includes Promoting Interoperability (PI) measures linked to certified EHR usage | Must use certified EHR technology to qualify, especially for Advanced APMs |
| Exemption Status | All eligible clinicians must participate unless exempt for other reasons | If you’re a qualifying APM participant, you’re off the hook for MIPS reporting—and you could even earn a bonus on top. |
| Ideal for | Practices seeking incremental improvements through a structured scoring framework | Practices ready to align with value-based care and handle financial/shared risk dynamics |
Practical Tips for Successful MIPS Reporting
- Prioritize categories weighted heavily toward your final score.
- Align clinical quality reporting measures with areas where your practice already performs well.
- Stay on top of CMS updates so you are never blindsided by rule changes.
- Consider joining accountable care organizations for real team-based advantages.
- Make MIPS reporting part of your workflow—not a year-end scramble.
Conclusion
MIPS reporting doesn’t have to be overwhelming. Once you understand the Merit-Based Incentive Payment System, you’ll see more than paperwork, you’ll see a roadmap for higher quality, better patient outcomes, and yes, bigger Medicare incentives.
It comes down to this:
- Learn the rules.
- Select the right measures.
- Report consistently.
- Aim higher than minimum thresholds.
Do this, and you don’t just avoid the sting of negative payment adjustments. You’ll position your practice as a leader ready for the future of value-based care. With the right approach, MIPS reporting isn’t just paperwork—it becomes a real opportunity to grow your practice and boost revenue.
Simplify MIPS reporting, leverage PI compliant technology like CERTIFY Health that helps track performance in real time and create reports automatically, so you can focus on what matters most: delivering better care.
























