Table of Contents
TL;DR: Communication in Healthcare
Effective communication is the core strength of a safe and efficient hospital.
Breakdowns cost U.S. hospitals billions and are a leading cause of preventable adverse events and medical errors.
How Critical is Healthcare Communication?
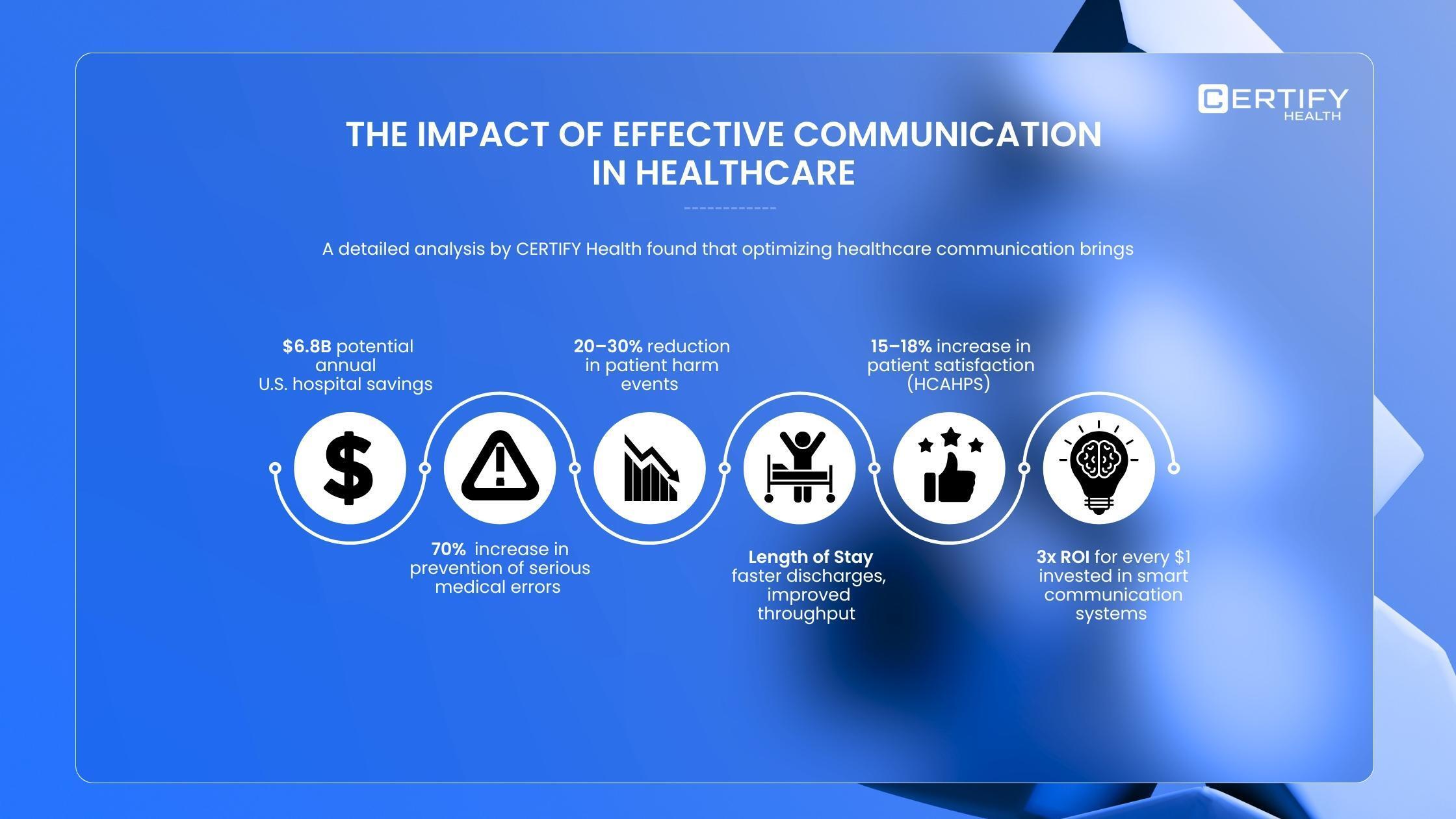
- Financial Impact: Robust communication systems could save U.S. hospital systems up to $6.9 billion annually by boosting efficiency and reducing costly readmissions and delays.
- Patient Safety: Clear communication is essential for safety, helping prevent an estimated 671,440 adverse events each year.
Root Causes and Solutions
Communication failures most often stem from unverified assumptions, poor shift handoffs, fragmented technology/EHRs, and a lack of standardized protocols.
Key technology features to drive success include:
- Real-Time, Secure Messaging with read receipts for accountability.
- Automated Alerts for critical information like lab results.
- Structured Handoff Templates (e.g., SBAR) to ensure complete information transfer.
- Patient Engagement Modules like two-way texting and campaigns.
Measuring Success (KPIs)
Hospitals must track performance using key indicators to measure effectiveness:
- Readmission Rates: Reflects the clarity of discharge instructions.
- Average Turnaround Time: Measures efficiency in diagnostics and results.
- Patient Experience (HCAHPS): Gauges clarity of communication from staff.
- Staff Responsiveness: Assesses how quickly patient needs are met.
Roadmap to Communication Excellence
A successful initiative involves auditing current workflows, setting clear KPIs, adopting integrated technology, and training staff (especially in methods like Teach-Back).
The ultimate goal is to embed communication excellence into the hospital’s continuous improvement culture.
Communication in Healthcare: Why It Can Make or Break Your Hospital
Healthcare communication is more than just interaction. It’s a lifeline.
Yet, too often, care providers overlook the tiny nuances that make communication in hospitals effective. Ignoring them can cost millions.
In the United States alone, hospital systems could save up to 6.9 billion dollars annually with robust communication platforms.
Financial imperative matters. Ethics matter more.
Clear communication isn’t just financially beneficial; it’s essential for patient safety.
The benefits of investing in communication strategies and systems far outweigh the hesitation.
The return on investment is tangible: fewer adverse events, optimized patient length of stay, faster discharges, and higher patient satisfaction.
And satisfied patients translate into credibility and trust for your healthcare brand.
Did you know?
Patients who face communication challenges are three times more likely to experience preventable adverse events than those who do not.
What Are Preventable Adverse Events?
Preventable adverse events (PAEs) are incidents that could have been avoided through proper care and adherence to established guidelines.
Reducing communication barriers could prevent an estimated 671,440 adverse events in the US each year.
In this blog, we will explore why communication barriers exist, the tools and strategies hospitals can implement for better outcomes, and the key metrics used to measure communication performance.
Why Communication Breakdowns Happen in Modern Hospitals
Here’s the truth: even leading hospitals struggle with bidirectional information exchange.
Without a streamlined structure for communication, collaboration suffers, and care transitions become vulnerable moments where critical information can slip through the cracks.
5 Key Reasons Communication Breaks Down in Hospitals
- Incomplete or missing information
- Errors during shift handoffs and department transfers
- Slow workflows due to fragmented tech & incompatible EHRs
- Language barriers & low health literacy affecting patient car
- Lack of standardized communication protocols
The Human and Financial Cost of Poor Communication
Poor communication does more than just confuse staff.
It makes patients doubtful about medications and hesitant to share their follow-up needs.
Ineffective communication is the leading cause of healthcare sentinel events.
What Are Preventable Adverse Events?
Preventable adverse events (PAEs) are incidents that could have been avoided through proper care and adherence to established guidelines.
Even more startling, healthcare staff spend almost half their day on EHR and data entry, yet most errors are linked to EHR-related communication bottlenecks.
These lapses frustrate both patients and staff, driving high staff turnover and operational inefficiencies.
Inefficient communication systems make delays inevitable.
A single communication lapse can cause care delays ranging from hours to several weeks, affecting hospital stay lengths, appointments, and staff time.
These issues may seem small in isolation, but together they lead to avoidable readmissions, safety events, and malpractice claims.
Did you know?
30% of all malpractice claims in healthcare stems from communication failures.
What are malpractice risks?
Malpractice risks are the chances healthcare providers face legal action, refunds, or claims due to communication errors that harm patients and compromise safety and satisfaction.
Defining Communication Success: KPIs and Measurable Outcomes
1. Readmission Rates
When patients leave without full clarity, they often come back.
That’s a readmission, and it’s a return visit that essentially could have been avoided with better communication.
Track your 30-day readmission rates to understand how well your team communicates discharge instructions and follow-up care.
Simple fixes work wonders.
Clear instructions, teach-back methods, and written care plans can dramatically reduce unnecessary readmissions.
What Is the Teach-Back Method in Healthcare?
The Teach-Back Method is an essential two-way communication micro step for patient safety.
We move beyond simply asking, “Do you understand?”
Instead, we ask the patient to restate critical details in their own words.
This process immediately flags confusion, forcing providers to re-explain until the message is clear.
This simple technique dramatically reduces medical errors and readmissions, ensuring patients are empowered and truly thriving in their care.
2. Average Turnaround Time for Tests and Results
How long does it take from ordering a diagnostic test to sharing results with the care team or patient?
That’s your average turnaround time and it’s one of the clearest indicators of internal communication health.
Gaps between departments like labs, radiology, nursing, and physicians often create bottlenecks.
Real-time updates and integrated communication tools can close these gaps and speed up results, thereby ensuring faster, safer care delivery.
3. Patient Experience Measures (HCAHPS Scores)
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey gives hospitals a powerful mirror into patient perception.
It captures everything from how clearly doctors and nurses communicate, to whether patients understood their medications, to how responsive staff were during discharge.
High HCAHPS scores are proof that your communication strategy is working.
4. Responsiveness to Patient Needs
Every patient moment matters. Metrics that measure nurse responsiveness, pain control, and how quickly patient needs are met reveal much about your care environment.
When communication flows seamlessly, patients don’t just recover faster; they leave with confidence in their care and trust in your brand.
Communication Tool Features That Drive KPIs
Once you have identified your communication with KPIs, the next step is to record your baseline values.
This means noting the current performance of your communication systems before introducing a new tool or strategy.
Tracking progress begins with knowing wh
1. Real-Time Messaging with Read Receipts
Real-time messaging makes healthcare communication faster, clearer, and more accountable.
It enables secure, two-way communication between providers and patients with features like read receipts, so everyone involved knows the status of a task and who has received or responded to important updates.
Unlike casual messaging apps, healthcare-grade messaging tools are HIPAA-compliant and auditable, making them both secure and trustworthy for sensitive clinical communication.
2. Automated Alerts for Lab Results or Bed Turnovers
Studies show that automated alerting systems for lab results can cut the waiting time between tests and treatments from 1.6 hours to just 1 hour.
That is a 38% reduction in response time, speeding up critical clinical decisions and patient care.
3. Structured Handoff Templates
Handoffs are one of the most vulnerable moments in care delivery.
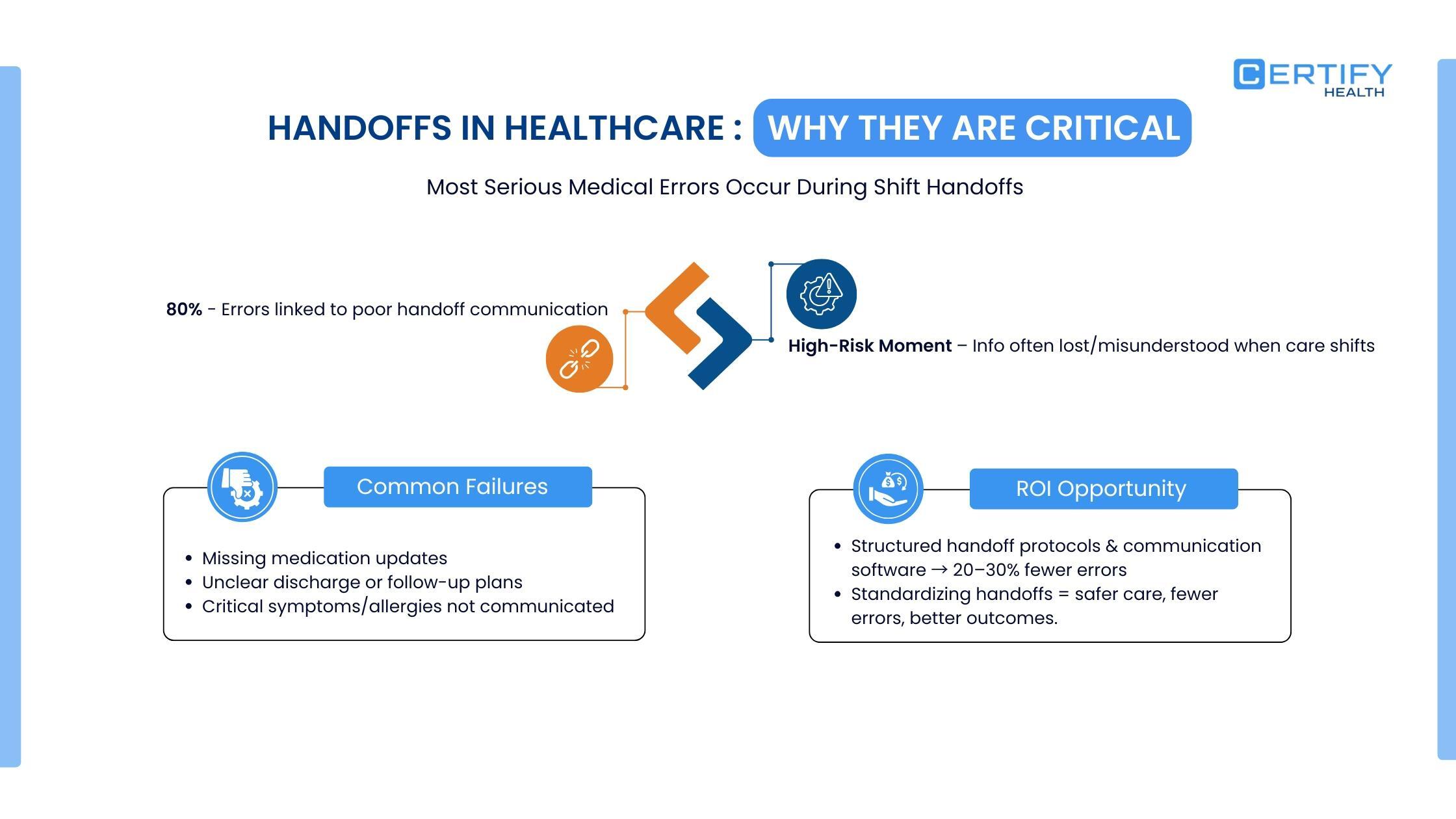
Structured templates remove ambiguity and ensure that information is passed accurately and completely.
A proven framework used across healthcare is SBAR, which stands for Situation, Background, Assessment, Recommendation.
| Component | Description | Focus |
|---|---|---|
| Situation | A brief, clear statement of the problem and reason for communication. | What is happening right now? (Eg: “I’m calling about Mr. Jones in room 302 who has new-onset chest pain.”) |
| Background | Relevant clinical context and history related to the situation. | What is the background? (Eg: “He had a knee replacement two days ago and has a history of coronary artery disease.”) |
| Assessment | Analysis of the situation and what you believe the problem might be. | What do I think is happening? (Eg: “He may be having a cardiac event. His pulse is 120, and he’s restless.”) |
| Recommendation | A specific request or action that you want the receiver to take. | What do I need from you? (Eg: “I recommend immediate EKG and stat labs. Can you see him now?”) |
At CERTIFY Health, structured handoff forms and workflow templates support consistent, reliable transitions of care.
They act as a repository of documentation, ensuring that information remains consistent across the entire patient’s journey and can be referenced later for continuity and safety.
4. Patient Engagement Modules
Unified healthcare platforms like CERTIFY Health bring all communication tools together.
It combines two-way messaging, automated alerts, and structured handoffs within one connected system.
It also helps streamline patient outreach, recalls, reminders, and surveys, making it easier to stay engaged and reduce missed appointments. Educational follow-ups after visits reinforce care and support better outcomes.
This creates a seamless, omnichannel communication flow across departments and touchpoints.
| Term | Definition |
|---|---|
| Two-Way Texting | A secure, asynchronous method of patient-provider communication that supports scheduling, reminders, follow-ups, and non-urgent care guidance. |
| Post-visit Engagement Campaigns | A systematic approach to automate outreach, follow-ups, patient education, and surveys across all care touchpoints to boost post-visit engagement, reduce no-shows, reinforce care, and improve outcomes. |
Next Steps: Launch Your Communication Excellence Initiative
Maximizing Your Healthcare Communication Strategy
Before launching a communication improvement plan, review KPIs, identify gaps, and choose tools that solve real bottlenecks.
CERTIFY Health delivers secure, scalable, and integrated communication solutions, from real-time messaging to structured handoffs, keeping teams aligned and patients safe.
Leading vs. Lagging Indicators in Healthcare Communication
Leading indicators are predictive measures. They help anticipate outcomes and guide proactive improvements in communication workflows.
Lagging indicators analyze past events. They reveal gaps, bottlenecks, or inefficiencies, which can then be addressed to strengthen future performance.
Lagging metrics feed directly into leading indicators, creating a continuous improvement cycle.
Deploy, Measure, and Optimize
Once you’ve identified gaps and chosen your tools, it’s time to put your plan into action. Use your tool analytics dashboard to link initiatives directly to results.
Monitor KPIs, track adoption, and measure improvements in real time.
Stepwise Roadmap to Communication Excellence in Hospitals
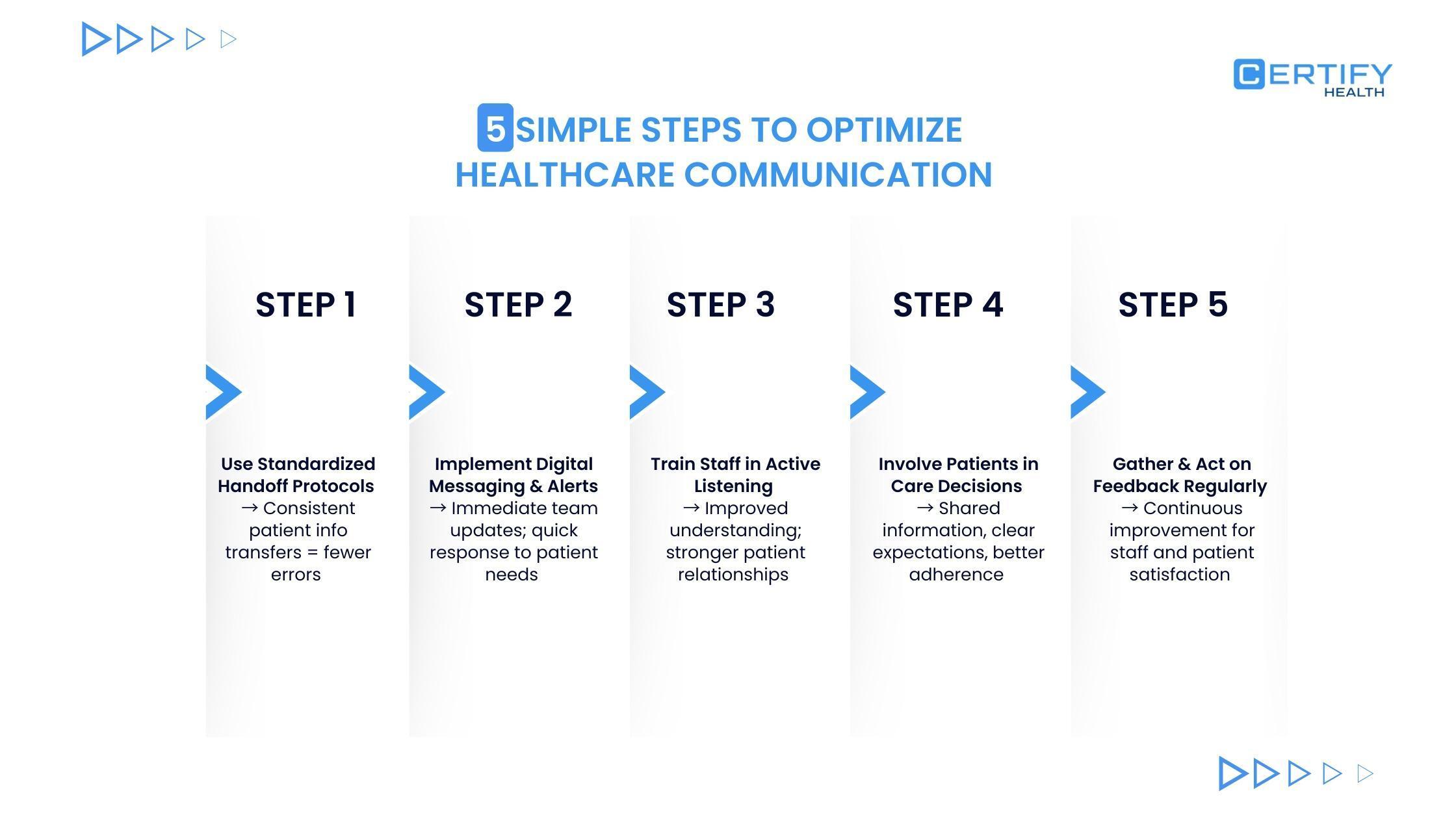
1. Conduct an Internal Assessment
- Audit current communication workflows and technology.
- Identify gaps in handoffs, team coordination, patient engagement, and language or cultural support.
- Map pain points to measurable KPIs such as readmissions, turnaround times, patient satisfaction, and staff efficiency.
2. Set Clear Goals and KPIs
- Define short-term and long-term communication objectives.
- Align KPIs with hospital priorities: safety, efficiency, patient experience, and financial outcomes.
- Establish baseline measurements for comparison after implementation.
3. Evaluate Technology Solutions
- Assess secure messaging platforms, mobile collaboration tools, and patient engagement modules.
- Check interoperability with existing EHR systems and HIPAA compliance.
- Consider scalability and vendor support for training and troubleshooting.
4. Develop a Phased Implementation Plan
- Pilot improvements in high-impact units like ED, ICU, or discharge processes.
- Expand gradually to other departments after validation.
- Assign accountability to project leads and cross-functional teams.
5. Train Staff and Manage Change
- Conduct competency-based training for nurses, doctors, and support staff.
- Establish “superuser” networks to support adoption.
- Use change management strategies to minimize resistance and sustain engagement.
6. Monitor Performance and Adjust
- Use dashboards to track KPIs and adoption rates.
- Hold periodic review meetings to identify bottlenecks or inefficiencies.
- Adjust workflows, templates, or tools based on data and staff feedback.
7. Communicate Wins and ROI
- Share measurable improvements like reduced errors, faster turnaround, and lower readmissions.
- Highlight cost savings and improvements in patient and staff satisfaction to maintain executive support.
- Document lessons learned for future cycles.
8. Plan for Continuous Improvement
- Establish ongoing feedback loops and quarterly KPI reviews.
- Introduce iterative improvements as technology evolves.
- Make communication excellence a permanent part of hospital culture.
Future Trends in Healthcare Communication
HIPAA-Compliant Messaging
Secure messaging in healthcare is taking off.
In just six months, adoption has increased by 30%, with each provider sending at least 30 messages daily.
This drives faster response times and fewer errors.
Video Consultations
High-quality video conferencing is changing healthcare delivery.
Studies show that video consultations cut specialist response times by over 50%, speeding up diagnoses and treatment for inpatients.
Integrated Patient Portals
Patient portals that combine telehealth and messaging increase engagement and reduce missed appointments by 35% thanks to automated reminders and two-way communication.
AI-Based Alerts
AI systems analyze workflows, spot anomalies, and predict errors in real time.
These tools show 113% higher accuracy in flagging potential mistakes compared to manual methods.
Workflow Automation
Chatbots, automated scheduling, and alert systems can eliminate human communication errors while reducing administrative burdens for clinical teams.
Integrated Communication Solutions
Platforms that unify EHR, secure messaging, and patient portals enable 24/7 connectivity, supporting continuous care for chronic and rural populations.
Frequently Asked Questions
How can hospitals measure communication effectiveness?
Track readmission rates, HCAHPS scores, response times, and staff feedback. These metrics reveal how clearly information flows between teams and patients.
Which tools most effectively reduce clinical errors?
Secure platforms like CERTIFY Health combine real-time messaging, automated alerts, and structured handoff templates to reduce errors, speed up care, and strengthen collaboration.
























