Table of Contents
TL;DR: Enhancing the Patient Journey with Effective Therapy Practice Management
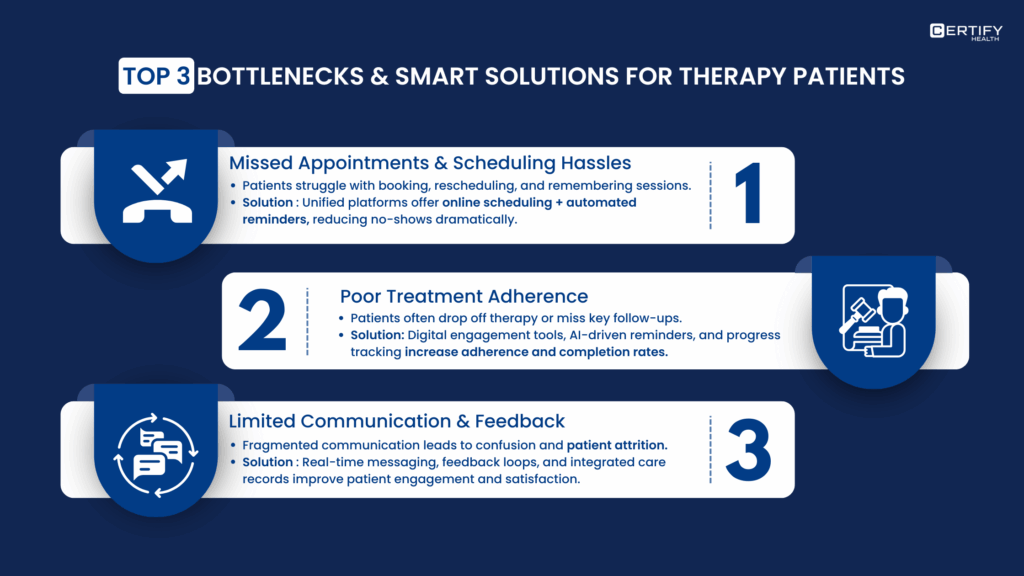
The modern therapy journey (from awareness to long-term wellness) is often fragmented by delays, drop-offs, and administrative friction. Nearly 30% of therapy appointments go unattended, and 70% of patients discontinue after one or two sessions, while clinician burnout surpasses 50%.
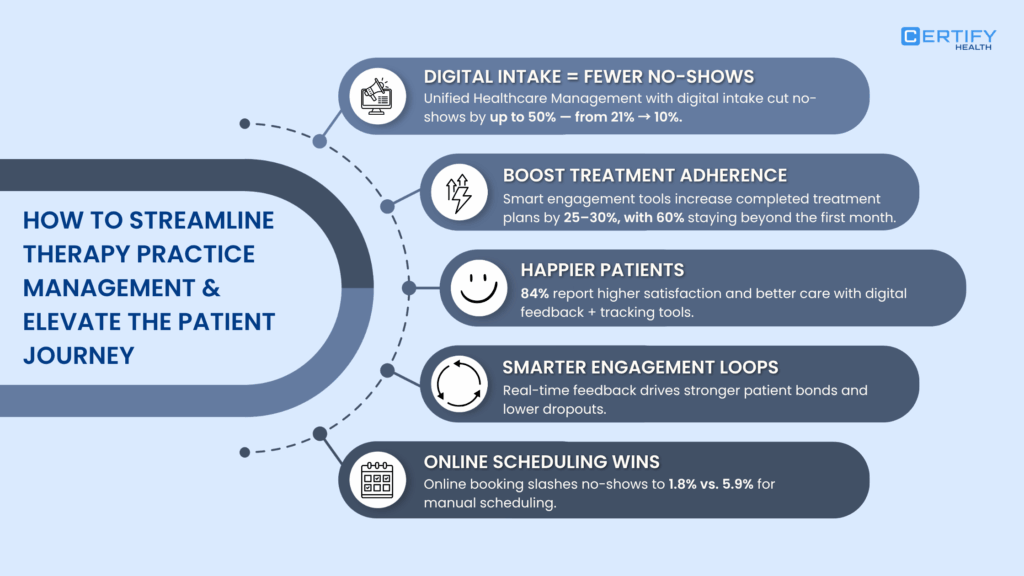
Therapy Practice Management solutions bridge these gaps by integrating scheduling, communication, and data tracking to create a seamless, patient-centered experience.
Key Takeaways:
- Awareness: Over 1 in 5 U.S. adults experience mental illness, yet many never enter care. TPM platforms convert digital interest into booked sessions through automation and simplified access.
- Intake: Streamlined intake workflows and therapist matching increase engagement by 10–15% and significantly reduce no-shows.
- Active Therapy: A strong therapeutic alliance, proven to predict outcomes across 295+ studies, combined with digital reminders, boosts completion rates by 20–27%.
- Follow-Up: Patient portals improve treatment adherence by 30–40%, while automated follow-ups sustain engagement and prevent dropouts.
- Wellness: Tools like the Patient Activation Measure (PAM) help clinicians track self-management and ensure lasting recovery.
In short, integrated therapy practice management transforms fragmented care into connected healing. This reduces clinician burnout, enhancing patient satisfaction, and driving better clinical outcomes.
CERTIFY Health offers an all-in-one solution to digitize, personalize, and future-proof every stage of the therapy patient’s journey.
Introduction: Why Effective Therapy Practice Management is Key to a Smooth Patient Journey
In mental and behavioral healthcare, every touchpoint matters. From the first patient intake to the final follow-up, each interaction shapes how patients feel supported and understood.
Yet despite record demand for therapy and behavioral health services across the U.S., nearly one in three appointments go unattended, with community clinics and specialty practices consistently reporting no-show rates ranging between 20% and 30%.
Even more concerning, over 70% of patients who begin outpatient mental health care drop out after just one or two visits, leaving their needs unmet and outcomes uncertain.
At the same time, burnout among mental health clinicians exceeds 50% in many care settings, driving unprecedented turnover, and shrinking the workforce faster than it can be replenished.
These numbers reveal a fundamental disconnect: while digital innovation accelerates, persistent gaps in patient engagement, adherence, and provider well-being continue to challenge the industry’s promise of lasting impact.
Too often, disconnected systems and heavy paperwork create barriers that fragment care and weaken trust.
Therapy practice management offers a solution through integrated workflows, streamlined scheduling tools, and empathetic communication; providers can simplify operations, increase engagement, and improve outcomes.
According to the Journal of the American Board of Family Medicine, patients who receive integrated behavioral health care report stronger coping skills, less fear, and greater overall well-being.
This blog explores the complete patient journey and how modern practices can leverage technology, communication, and empathy to deliver better results at every stage.
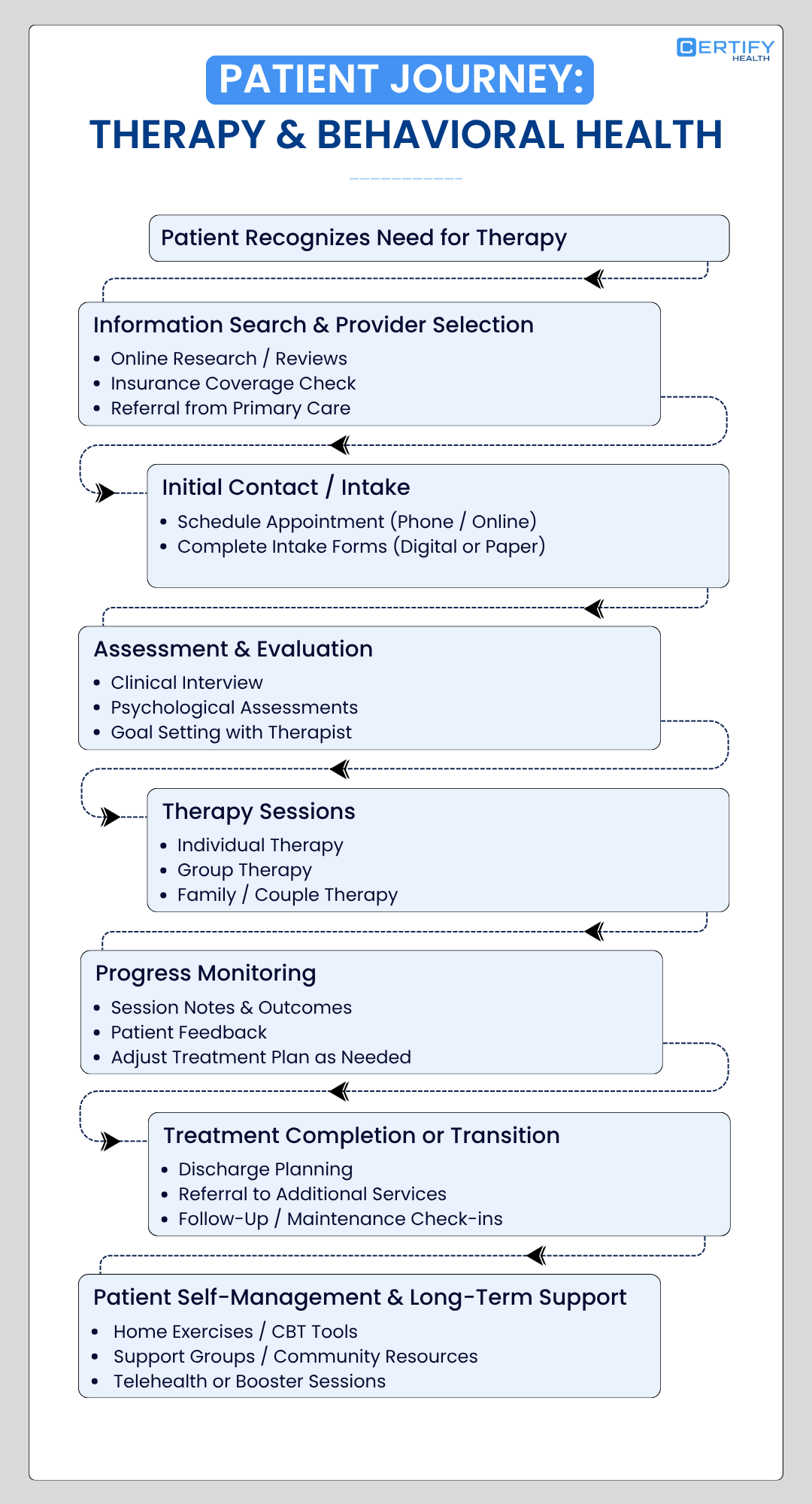
Understanding the Modern Patient Journey in Therapy & Mental Healthcare: Critical Stages and Impact on Recovery Outcomes
| Stage | Description | Context & Data | Common Pain Points |
|---|---|---|---|
| Awareness | Patients notice symptoms and research care. | Social media, online health sources are common entry points. | Confusion, stigma, uncertain where to begin. |
| Intake | Patients access, schedule, and complete forms. | National average waitlist: 9–13 weeks for initial appointments. | Long waitlists, complex paperwork, and digital access issues. |
| Therapy | Clinical assessment and ongoing sessions. | Digital therapy dropout rates average 9–12%. | Anxiety, unclear expectations, poor communication. |
| Follow-Ups | Continued communication & care adjustments. | No-shows and cancellations rise after the first few sessions. | Lost motivation, limited reminder systems, and access gaps. |
| Wellness | Maintenance, lifestyle change, engagement. | Patient engagement declines long-term without digital support. | Isolation, lack of check-ins, and low retention. |
1. Awareness and Discovery
WHO reports that over 1 billion+ people suffer from mental health conditions globally. In the U.S. alone, nearly one in five adults (that’s over 60 million people) experienced a mental illness in 2024.
And yet, millions never make it into care. It is well-known that the first step in the patient’s journey doesn’t happen online. People type “anxiety,” “depression,” or “therapy near me” into search bars or ask AI-powered chat tools for advice.
But here’s the problem: digital discovery alone doesn’t equal care. Many never move beyond research mode. They get answers but not help. Engagement doesn’t automatically mean they’ll show up for therapy.
Recent studies analyzing Google Trends reveal rapidly growing mental health information seeking search intent rose 67% over a decade.
CDC, NIMH, and other statistical data studies provide complementary surveillance data but even increases in search queries rarely translate to care utilization; they mainly flag evolving risk, not conversion to treatment.
H4 Bridging the Gap: Digital Mental Health Interventions (DMHIs) and Therapy Practice Management Systems
Here’s where digital mental health interventions (DMHIs) and therapy practice management systems come in.
Despite increased awareness and digital health searches, initiation rates for therapy remain low. For example, in one national US study, even among insured patients flagged as needing behavioral or diabetes therapy, only 49–69% initiated therapy within 6 months and many never began care after awareness/diagnosis.
Insurance coverage gaps, mental health stigma, and poor digital/health literacy all sharply reduce the likelihood that US patients convert awareness into actual care for mental and behavioral health problems.
Digital literacy issues prevent effective use of digital health solutions, especially in populations that may be excluded or lack internet access.
Unified Health Practice Management Softwares (like CERTIFY Health) transforms casual curiosity into committed care, making it easier to schedule appointments, connect with clinicians, and stay engaged throughout treatment.
What are Digital Mental Health Interventions (DMHIs)?
Digital Mental Health Interventions (DMHIs) are therapeutic or supportive programs delivered through the Internet (e.g., via websites or online platforms) and/or mobile applications.
2. Intake: Turning Patient Interest into Engagement
If awareness is where the journey begins, intake is where trust begins. It is that pivotal moment when curiosity becomes connection, when a potential patient takes the leap from “I need help” to “I am ready to talk.”
Peer-reviewed benchmarking from public behavioral health in the US supports that reducing intake friction led to measurably higher show-up rates for the first session and improved ongoing engagement.
Digital systems that enabled easier paperwork and smart therapist assignment increased intake-to-session conversion by 10–15%.
Also, patients matched to therapists with proven strengths in treating their mental health concern are significantly more likely to engage, complete intake, and have better retention compared to non-matched assignments.
In some cases, even Electronic Medical Record (EMR) systems create workflow bottlenecks at intake due to slow interfaces, repetitive data entry, and extensive paperwork requirements.
Excessive forms and complex digital platforms increase administrative burden, delay intake completion, and drive drop-offs.
In a large US public behavioral health system study involving 5,168 patients, reducing EMR friction and paperwork bottlenecks improved clinically significant patient outcomes by 10–15% compared to conventional intake with higher friction.
Specifically, 42.9% of clients using a streamlined intake process achieved clinically significant change, matching or exceeding benchmark rates from university counseling centers (41.6%) and surpassing older public health settings by more than double.
Intake includes every touchpoint from the first phone call, form of submission to therapist for matching, EMR, and scheduling.
It may seem like an administrative process, but in truth, it shapes the emotional tone of the entire therapy planning.
The Power of a Seamless Intake Experience
In therapy, first impressions matter. Your intake process sets the tone for the therapeutic relationship and can determine whether a person becomes a committed patient or simply walks away.
Think of it as your digital handshake for lasting patient relationships: warm, clear, and easy. Checklists, templates, and digital intake platforms should work together without friction.
Every interaction, from filling out a form to scheduling a session, should feel intuitive, supportive, and personal.
Three Metrics That Define an Effective Intake Flow
1. Percentage of inquiries converted to first sessions: This measures how well your outreach and onboarding turn interest into action.
The time lag between patient inquiry and first scheduled therapy is crucial for retention. Industry data recommends responding within 1 business hour for optimal conversion; delays of several days sharply increase dropout.
National studies note that reducing wait times by even 10% can lower no-shows and drop-off rates.
2. No-show rate for first sessions: Engagement matters only if patients actually show up.
No-show rates for initial therapy appointments in US settings average 33–37%, with some clinics reporting rates as high as 50%.
High no-show rates erode engagement and can disrupt clinical workflow. Evidence suggests that reducing wait times and deploying engagement strategies significantly decreases no-show rates.
3. Time from inquiry to first appointment: Each extra day between “I need help” and “You are booked” increases the risk of dropout.
Studies state that attrition found that the modal number of sessions attended for either psychotherapy or medication treatment was only one session, meaning many inquiries do not convert into ongoing care and frequently result in just one initial session.
In a Philadelphia community mental health system analysis across 10 years and 7,391 cases, the median number of psychotherapy sessions attended was five, confirming a pronounced drop-off after initial engagement, and an implied low inquiry-to-full treatment conversion rate.
The Human Element: Therapist Matching
A strong intake process also includes therapist matching. When patients are paired with therapists whose expertise, approach, and personality align with their needs, it creates faster rapport and better outcomes.
This alignment builds trust, safety, and openness, which are the foundations of effective therapy.
Patient Intake Directly Impacts Retention
In mental health care, confusion and delay can damage confidence.
If the intake process feels complicated, intimidating, or slow, patients often give up before they ever begin treatment.
Globally, about 30% of mental health patients in high-income countries and 45% in middle and low-income countries discontinue treatment after the first interaction, according to the World Health Organization.
That is not just a scheduling problem. It is a systems problem.
3. Active Therapy: Building Connection and Driving Better Patient Reported Outcomes
Active therapy is the heart of the patient’s journey. It is where treatment truly begins and where patients experience meaningful change. Therapy can take many forms: in-person sessions, online therapy, group programs, or one-on-one work.
No matter the format, this is the stage where healing happens and where consistency and connection matter most.
The Role of the Therapeutic Alliance
Effective therapy planning involves therapeutic alliance.
What is Therapeutic Alliance?
This alliance is the collaborative and emotional bond between patients and providers. It predicts positive outcomes across all types of therapy, regardless of the method or modality.
A meta-analysis of 295 studies with over 30,000 patients found a clear link: stronger therapeutic alliances lead to better outcomes in face-to-face psychotherapy.
Studies also show that therapist qualities matter. Empathy and genuineness were strongly tied to the strength of the therapeutic alliance, highlighting the key role of the therapist.
In adolescent therapy, early alliance ratings and agreement between client and therapist predicted outcomes. Low early alliance or mismatched perceptions undermined progress.
A strong alliance includes two essential elements:
- Goal and task agreement: Both patient and therapist share clarity on what they are working toward.
- Bond: A foundation of trust, empathy, and mutual respect that supports every session.
When your therapy practice fosters this alliance early, patient relationships last longer, and treatment completion rates are higher.
The Power of Digital Support in Active Therapy
Digital automation can help sustain engagement throughout this stage. Simple tool features such as appointment reminders, session summaries, and follow-up messages strengthen connection and accountability.
Research shows that multidimensional engagement (behavioral, cognitive, and emotional) is associated with 20 to 27% higher therapy completion rates.
When technology supports human connection, outcomes improve.
Tracking Quality During Active Therapy
To ensure consistent and effective care, it is vital to monitor key performance metrics throughout this stage.
Core indicators include:
- Session attendance rate
- Dropout rate during active therapy
- Therapeutic alliance survey scores
- Symptom and functional outcome measures
Tracking these metrics allows you to identify early signs of disengagement and address them before they lead to dropout.
Supporting Therapists for Sustainable Care
A thriving practice depends on the well-being of its therapists. Burnout among clinicians can lead to turnover, inconsistent care, and patient dissatisfaction. A longitudinal study published in The Annals of Family Medicine found that 53% of clinicians reported burnout, with 30% leaving their primary care roles within 2 to 3 years. Burnout was a significant predictor of clinician turnover
A 2025 survey by Harris Poll found that 55% of U.S. healthcare workers plan to change jobs by 2026, with 84% feeling underappreciated. Ineffective caseload management was the leading reason for considering career changes
Using integrated practice management tools can help therapists manage workloads more efficiently, track progress easily, and focus on the work that matters most: building connections and facilitating recovery.
A strong system does not just improve patient outcomes. It also nurtures the professionals delivering care, ensuring that both sides of the therapeutic relationship continue to grow.
4. Patient Follow-Up and Retention: Sustaining Care Beyond the Session
Therapy does not end when a session is done. Follow-up is the bridge that turns short-term care into lasting change.
When patients feel supported between appointments, they are more likely to stay consistent, manage their own progress, and reach better outcomes. This is where digital tools become powerful allies for both therapists and patients.
The Role of Patient Portals in Long-Term Engagement
Research shows that the use of patient portals significantly improves continuity and self-management.
Patients who actively use portals show 30 to 40 percent higher treatment adherence to ongoing mental health care.
For conditions such as obsessive-compulsive disorder (OCD), studies also indicate that adherence directly predicts treatment outcomes. When patients stay connected, informed, and accountable, recovery becomes more sustainable.
How Therapists Can Strengthen Follow-Up
Follow-up does not have to be complex. It only needs to be consistent and personalized.
Simple but powerful tools have:
- Automated reminders through SMS or email
- Peer support or maintenance groups
- Periodic check-in calls
- Data dashboards that flag clients at risk of dropping out
These systems help therapists maintain contact, track engagement, and offer timely support before a client disengages.
5. Patient Wellness: Sustaining Progress for the Long Term
Wellness is the final, but ongoing, stage of the patient’s journey. It focuses on sustaining the benefits of therapy and supporting long-term mental health.
A key tool in this phase is the Patient Activation Measure, or PAM.
What is Patient Activation Measure?
PAM evaluates a patient’s knowledge, skills, and confidence in managing their own health.
Using a 10 or 13-item survey, it measures “activation,” showing how aware a patient is of their treatment and responsibilities in the care process.
| PAM Level | Score Range | Patient Characteristics |
|---|---|---|
| Level 1 | (Lowest) | Disengaged and overwhelmed. Patients may not yet believe they play an important role, lack fundamental knowledge, and feel passive. |
| Level 2 | Becoming aware but struggling. Patients have some knowledge but still lack confidence and may have a fatalistic view of their health. |
|
| Level 3 | Taking action. Patients have the knowledge and skills and are beginning to take action but may lack confidence and struggle to maintain behavior change under stress. |
|
| Level 4 | (Highest) | Maintaining behaviors and pushing further. Patients are highly self-managing, proactive, and resilient in maintaining their health behaviors. |
Wellness as a Sustained Practice
Reaching wellness does not mean that therapy is over. It is a continuous practice that ensures the positive effects of treatment endure. Because many mental health conditions are prone to recurrence, ongoing support, self-management, and monitoring remain essential.
PAM helps therapists identify where patients are in their journey, guide interventions, and foster long-term engagement.
Wellness is about building resilience, maintaining progress, and empowering patients to thrive beyond therapy.
Conclusion: Why Seamless Patient Journey Matter in Therapy
For therapy providers, offering optimal care is only half the battle.
The other half is ensuring a seamless, supportive experience for patients at every touchpoint.
In mental health care, where trust and comfort are paramount, a smooth, connected journey helps patients feel safe to open up and trust their provider.
Did you know that about 60% of mental health patients opt for Cognitive Behavioral Therapy (CBT)?
It’s evidence-based and effective for treating anxiety, depression, and other disorders. But for therapists, managing patients with CBT requires more than just expertise; it requires the right practice management solutions.
Patient management software is essential for therapy clinics of all sizes. It helps streamline the entire patient journey, improve patient satisfaction, and increase long-term success.
Whether you’re using Cognitive Behavioral Therapy (CBT) or any other modes of therapy, the patient’s journey mapping may slightly differ. But the key to their journey’s success remains the same: efficiency and engagement.
Focus on improving these touchpoints to future-proof results for your patients and your practice.
Ready to Elevate Your Therapy Practice?
Discover how CERTIFY Health can transform your practice with measurable ROI and enhance patient journeys. Schedule a demo today!
Frequently Asked Questions
How can hospitals measure communication effectiveness?
Track readmission rates, HCAHPS scores, response times, and staff feedback. These metrics reveal how clearly information flows between teams and patients.
Which tools most effectively reduce clinical errors?
Secure platforms like CERTIFY Health combine real-time messaging, automated alerts, and structured handoff templates to reduce errors, speed up care, and strengthen collaboration.
























