Table of Contents
Key Takeaways:
- Fragmented systems drive higher costs, burnout, and revenue leakage; unified platforms fix this at the data and workflow level.
- True unified healthcare platforms connect care, operations, and revenue in real time, not just via bolt-on integrations.
- The right platform in 2026 is the one that delivers measurable ROI, scales across sites, and reduces IT complexity.
With U.S. healthcare spending soaring to $4.3 trillion annually, the cost of fragmented care is no longer a back-office issue; it’s a system-wide problem. Every disconnected workflow, duplicate data entry, and manual workaround quietly adds friction, delays care, and drives up administrative waste.
Fragmentation doesn’t happen because providers choose it. It happens because care delivery, operations, and payments are often spread across multiple systems that were never designed to work together. Over time, this creates broken handoffs between scheduling, clinical care, billing, and patient communication.
This is where the shift toward unified or integrated healthcare begins.
So, What Is Integrated Healthcare?
At its core, integrated healthcare is coordinated care delivered across professionals, settings, and systems, with a continuous flow of information instead of disconnected episodes and siloed tools.
In ambulatory or outpatient care, patients receive diagnosis, treatment, or rehabilitation without an overnight hospital stay across settings such as physician offices, urgent care clinics, dialysis centers, and same-day surgery facilities.
Because care is delivered across multiple touchpoints, fragmented systems often force patients and staff to navigate disconnected workflows, increasing friction, cost, and patient churn.
A truly integrated ambulatory experience means one connected journey, from digital check-in and scheduling to charting, care coordination, and payment, not six logins and a pile of sticky notes.
In platform terms, a unified healthcare platform is a single, integrated healthcare system layer that connects EHR, patient experience, practice management, RCM, patient management, and analytics so data moves in real time instead of getting stuck in silos.
Think of it as a healthcare integration engine plus workflow layer: one source of truth for demographics, eligibility, documentation, orders, tasks, and financials that your team and your patients actually experience as an all in one solution.
This guide walks through what “unified” really means for ambulatory or outpatient care, lays out practical evaluation criteria, and then ranks the top 10 unified healthcare platforms for 2026.
Why 2026 Shift to Unified or Integrated Healthcare Systems?
The 2026 EHR and PM trendline is brutally clear: clinics that cling to bolt‑on tools and aging servers are watching costs climb while operational risk and turnover spike. Clinics that move to unified platforms see fewer hand‑offs, fewer denials, and more predictable revenue because clinical, operational, and financial data lives in the same integrated healthcare solutions backbone.
From a care delivery standpoint, integrated healthcare models improve outcomes by coordinating services around the whole patient instead of around individual visits or departments. When data flows through a true unified healthcare platform, teams can spot risk earlier, share plans across disciplines, and reduce duplicated tests and missed diagnoses that come from fragmented systems.
TL; DR:
What is causing healthcare practices to shift towards unified healthcare platforms?
These key challenges are driving healthcare practices to adopt unified platforms:
- Fragmented systems create care gaps, admin burden, and inconsistent patient experiences
- Disconnected data forces reactive care and drives staff burnout and revenue leakage
- Unified platforms connect data and workflows, enabling proactive care, automation, and scale
Pain Points Forcing the Shift to Integrated Healthcare Solutions
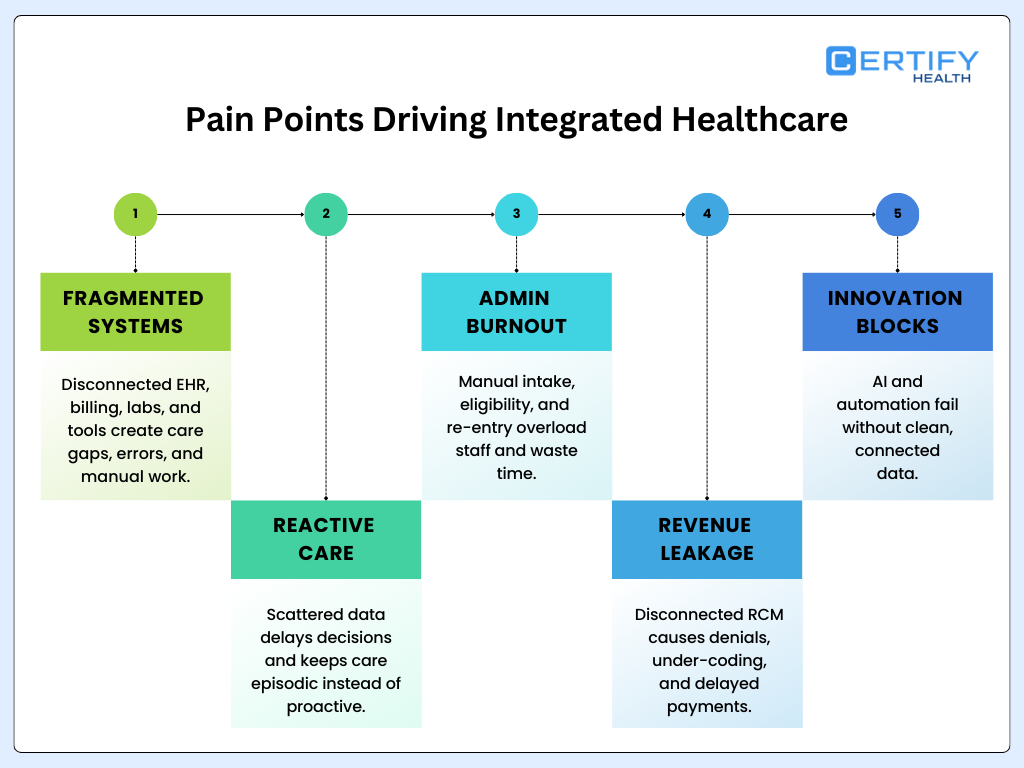
Fragmented Systems
EHR, billing, labs, imaging, and communication tools that do not talk to each other create broken care coordination, manual reconciliations, and blind spots in both clinical and revenue workflows. The result is more swivel‑chair work, more errors, and inconsistent experiences across multi‑location outpatient care networks.
Reactive Care
When information is scattered, clinicians lack longitudinal views and timely insights, which delays diagnoses and prevents proactive outreach or risk‑based care plans. Without unified data powering population health and decision support tools, teams default to episodic, reactive care based on the last visit note or loudest complaint
Admin Overload & Burnout
Manual eligibility checks, duplicate data entry between front‑office and billing, and paper forms overload staff and accelerate burnout. An integrated healthcare system that automates intake, benefits checks, and claim scrubbing off a shared record cuts low‑value clicks and gives nurses and front desk teams time back.
Revenue Leakage
Disconnected RCM stacks miss coverage issues, under‑code visits, and leak dollars through denials and delayed payments. Unified platforms that combine a healthcare integration engine, automated eligibility, and denial analytics catch issues at the source and tighten the full revenue cycle loop.
Innovation Bottlenecks
AI and automation only work when they sit on top of clean, connected data; patchwork tools block that. In contrast, modern unified platforms with standard APIs and real‑time streaming data can actually power AI scribes, predictive scheduling, and automated follow‑up without massive IT projects.
Unified/Integrated Healthcare System Evaluation Criteria
TL; DR:
How Should You Evaluate a Unified /Integrated Healthcare System?
Here’s how you can evaluate the unified/ integrated healthcare systems:
- Look beyond UI to platforms that truly unify clinical, operational, and financial data
- Prioritize in-workflow clinical value, real-time performance, and security by default
- Choose solutions that scale, reduce total cost of ownership, and simplify IT long-term
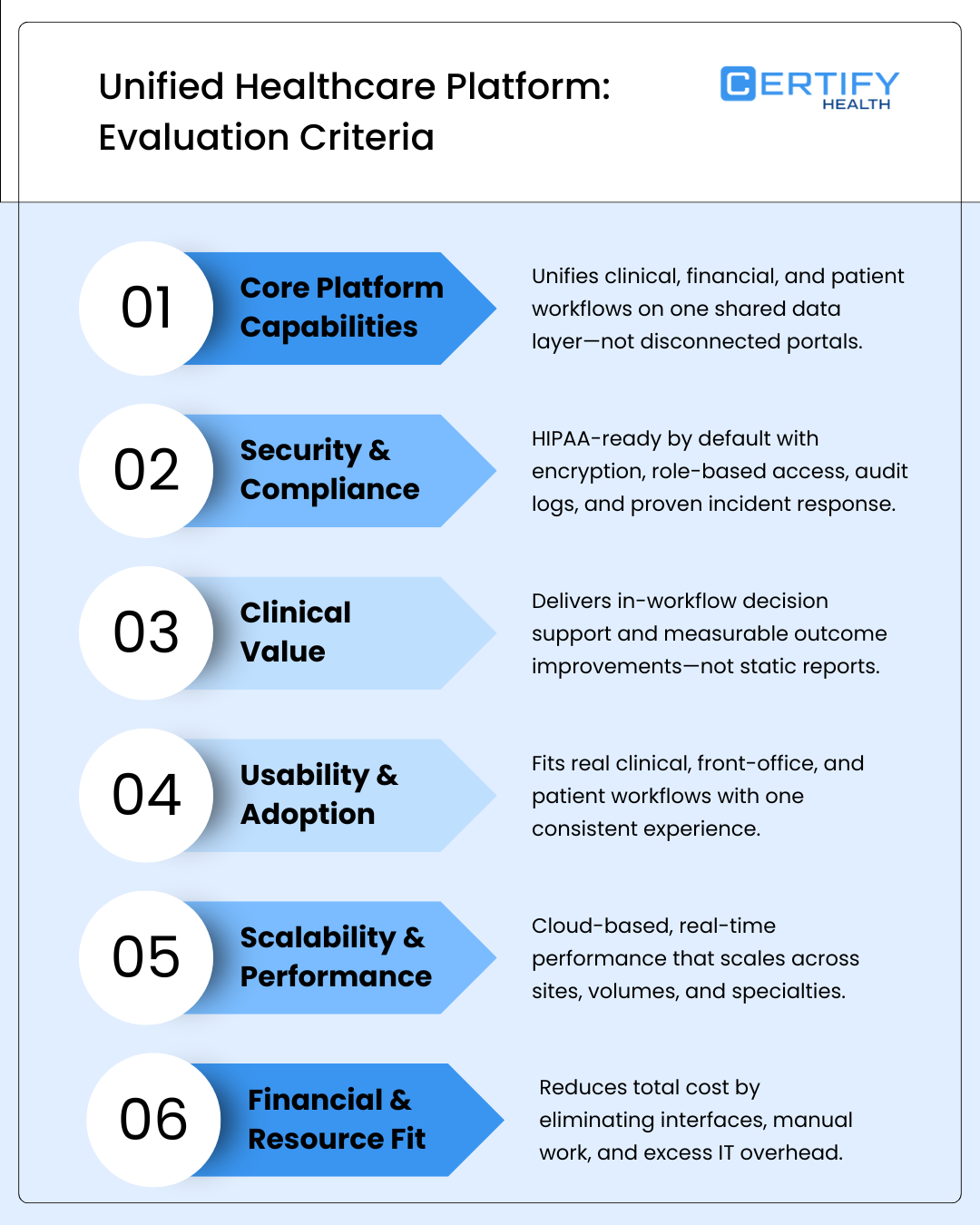
Choosing a unified healthcare platform is not about who has the flashiest UI; it is about who can unify data, workflows, and outcomes across your entire ambulatory footprint. The evaluation criteria below map directly to the realities of rising costs, staff burnout, revenue leakage, and escalating patient expectations you are already living.
Core platform capabilities
A serious platform must deliver deep healthcare system integration and data unification across clinical, financial, and engagement systems, not just “one more portal.” Look for a healthcare integration engine that supports standards‑based APIs, robust data exchange, and real‑time syncing so you are not constantly reconciling records between tools.
Unified intake, scheduling, documentation, billing, and collections should all ride the same data spine so you can truly act like an all-in-one solution for your patients and your internal teams. This is the difference between a glorified interface engine and a unified healthcare platform that can actually scale with your ambulatory care network.
Security & compliance
Confirm HIPAA support, BAAs, encryption in transit and at rest, granular role‑based access, and detailed audit logs backed by modern cloud security practices.
Investigate how the vendor handles vulnerability management, incident response, and third‑party risk, not just marketing claims. Practices should push for concrete interoperability and security assurances during the evaluation process to avoid adding yet another fragile point solution to the stack.
Clinical value
Clinical value is where integrated healthcare either shows up or gets exposed. Platforms should bring decision support tools into the actual workflow like flagging gaps, risk scores, and guideline prompts in context, not buried in a report you never open.
Look for measurable outcome improvement backed by case studies: reduced readmissions, higher adherence, or better chronic disease control driven by cross‑team care coordination. A real unified healthcare platform makes it easier for clinicians to collaborate, hand off care, and share plans across locations without fighting the technology.
Usability & adoption
If the workflows do not match how your clinicians and front office teams actually work, adoption dies on contact. Evaluate whether the platform can align to both clinical and admin workflows like intake, rooming, documentation, referrals, billing tasks, and follow‑up, instead of forcing everyone into rigid templates.
On the patient side, check for modern patient experience features such as mobile check‑in, digital forms, self‑scheduling, two‑way messaging, and text‑to‑pay that are natively integrated rather than bolted on. Great integrated healthcare solutions should feel like one branded experience across all your outpatient care sites.
Scalability & performance
In 2026, cloud infrastructure with high uptime and real‑time performance is non‑negotiable for multi‑site ambulatory groups and fast‑growing practices. Ask how the platform scales across locations, specialties, and volumes, and how it maintains response times as you add sites, providers, and integrations.
Real‑time data performance matters not just for clinicians but also for operations and finance, where laggy reporting and outdated dashboards kill decision‑making. A strong unified platform will support both transactional workflows and analytics on the same data foundation.
Financial & resource fit
Total cost of ownership goes far beyond subscription fees; it includes licenses you can retire, interfaces you do not have to maintain, and manual work you can automate. Assess ROI potential with concrete metrics: days in AR, clean claim rate, denial reduction, staff hours saved, and patient payment yield.
For many ambulatory groups, the right integrated healthcare system is one that reduces reliance on scarce IT headcount and minimizes custom interface work. The more you can standardize on a unified healthcare platform, the simpler your long‑term financial picture becomes.
Integrated Healthcare System Evaluation Process

A disciplined evaluation process prevents shiny‑object purchases that just add to fragmentation.
Involve cross‑functional stakeholder engagement early: clinical leaders, front office, billing, IT, and even patient advisory voices, so you are solving for the full journey, not just one department.
Run a current‑state tech audit, define goals, then move into structured vendor assessment and demos, followed by a pilot or proof of concept before full rollout.
Build implementation and support planning into the process up front, including data export, migration strategy, and 90‑day benchmarks for performance and ROI.
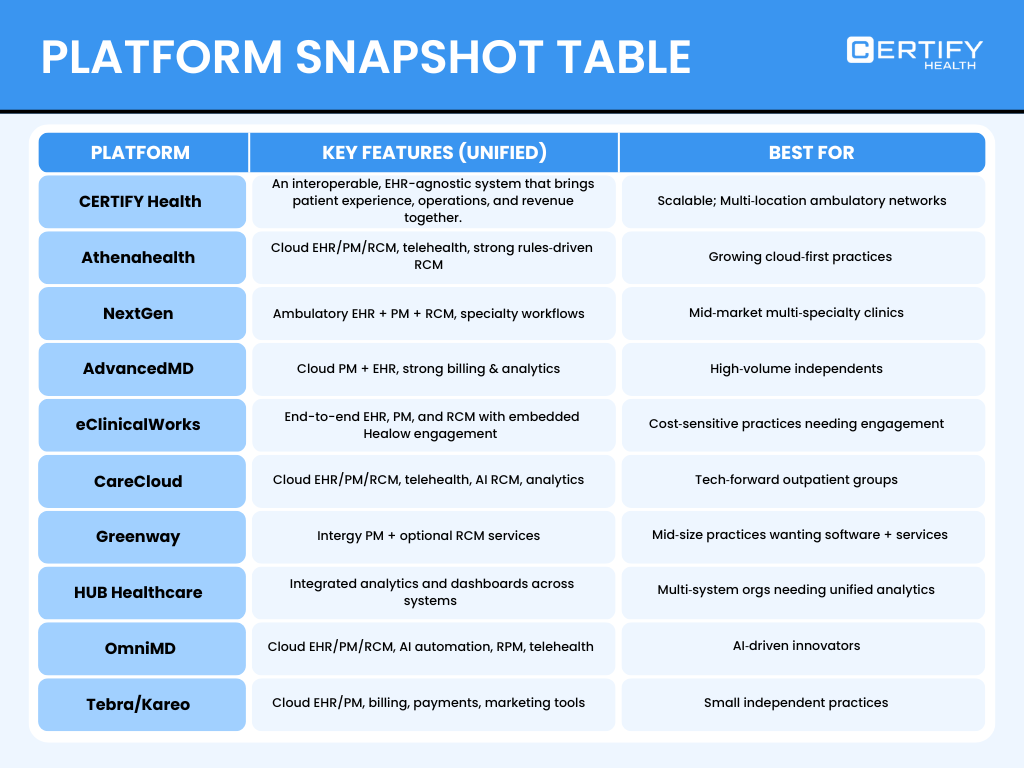
Top 10 Unified Healthcare Platforms for Ambulatory/Outpatient Care in 2026
CERTIFY Health is a unified healthcare platform and integrated healthcare system purpose‑built to sit across your existing 100+ EHRs, PMS, Billing, and other in-house systems, unifying patient experience, practice, patient management, and revenue & billing enablement without forcing a rip‑and‑replace.
With FaceCheck, real‑time eligibility, text‑to‑pay, and end‑to‑end RCM, it stops revenue leakage at the front door while reducing front desk workload by 60+ staff hours per month.
Through its partnership with DentalBee, CERTIFY extends into AI‑assisted charting and documentation, creating a continuous experience from check‑in to charting to payment for dental and broader outpatient care workflows. The platform’s AR under 45 days and ~95% clean claim metrics show tangible ROI potential for multi‑location practices that want unified revenue and operations without changing their core clinical systems.
Pros
- Unified, EHR‑agnostic layer that modernizes patient experience, practice, patient management, and RCM without massive clinical change management.
- Ideal for multi‑location ambulatory care groups.
- Strong financial and operational lift with compressed AR cycles, higher clean claims, and significant staff time savings, delivering fast total cost of ownership payback.
Cons
- Best suited for practices ready to standardize processes across locations.
Athenahealth delivers a fully cloud‑based EHR, PM, and RCM suite (athenaOne) that centralizes scheduling, eligibility, claims scrubbing, and outreach. Its revenue cycle tools leverage a massive rules engine and payer network, which helps maintain high first‑pass acceptance rates and strong collections performance in outpatient care.
Pros
- Cloud‑based, scalable platform that removes on‑premise server burden and aligns with modern integrated healthcare system strategies.
- Continually updated claim rules and payer insights improve financial outcomes without heavy internal RCM engineering.
Cons
- UI is often described as dated and click‑heavy, which can slow down clinical adoption and fuel staff burnout.
- Larger scale and growth have created perceptions of less personalized support for some practices.
NextGen Healthcare offers an integrated EHR and practice management platform with embedded billing and revenue cycle tools tailored for ambulatory environments. Color‑coded schedules, specialty templates, and configurable workflows make it a fit for multi‑specialty outpatient care networks looking for one login across appointments, documentation, and billing.
Pros
- True all in one solution for mid‑sized practices with integrated scheduling, documentation, and RCM.
- Strong specialty content and configurability for nuanced integrated healthcare workflows.
Cons
- Interface and patient portal feel dated versus newer engagement‑first platforms, particularly for digital‑savvy patients.
- Complex configuration and reporting often require vendor assistance, raising practical total cost of ownership.
AdvancedMD provides cloud‑based practice management, EHR, and a powerful billing engine tailored to high‑volume independent practices. Its strengths lie in robust scheduling, denial tracking, and business intelligence that together behave like a unified revenue‑first platform.
Pros
- Strong RCM capabilities and reporting that reduce revenue leakage for busy ambulatory care clinics.
- Flexible scheduling and multi‑site support make it practical for complex provider calendars.
Cons
- Implementation can be demanding.
- Pricing and feature depth can be overkill for small, single‑provider offices.
eClinicalWorks (eCW) combines ambulatory EHR, PM, and RCM with the Healow ecosystem for patient engagement, telehealth, and digital check‑in. It offers configurable templates and workflows spanning everything from scheduling to population health, functioning as an integrated healthcare solutions stack for many practices.
Pros
- Broad feature set at a competitive price, appealing to cost‑sensitive outpatient care groups.
- Healow tools provide online scheduling, check‑in, and patient apps that strengthen unified patient experience.
Cons
- Reports of software bugs and support delays after updates can erode trust and adoption.
CareCloud delivers cloud EHR, practice management, RCM, and patient experience tools in one platform, with AI‑assisted revenue workflows and analytics. Real‑time syncing between clinical and billing data plus AI microbots that detect errors make it a strong option for unifying operations and revenue across ambulatory care.
Pros
- End‑to‑end RCM with automation that reduces denials and accelerates cash flow.
- Analytics modules expand integrated healthcare reach and decision support.
Cons
- Fit can vary for highly specialized or hospital‑owned groups with complex legacy ecosystems.
Greenway’s Intergy practice management software plus Greenway Revenue Services offers a combined software‑and‑services model for mid‑size practices. Scheduling, billing, claims, and managed RCM services work together as an all in one solution for groups that want a partner to run much of the revenue cycle.
Pros
- One‑stop shop with optional outsourced RCM that leverages the underlying PM feature set.
- Dedicated account managers can help optimize workflows and improve results over time.
Cons
- Historical outages and support complaints make some organizations cautious.
- RCM services are limited to Greenway users, restricting flexibility in hybrid environments.
HUB‑style practice hubs focus on connecting disparate systems into one unified analytics and performance dashboard rather than replacing EHRs outright. These platforms centralize data from scheduling, billing, marketing, and patient experience tools into one “command center” for outpatient care executives.
Pros
- Deep visibility into performance, growth levers, and bottlenecks across multiple tools.
- Acts as a healthcare integration engine for analytics and business intelligence, helping unify strategy even when systems stay fragmented.
Cons
- Primarily focused on analytics and insights rather than full operational workflow orchestration.
- Requires clean data feeds and disciplined data governance to achieve maximum value.
OmniMD offers cloud EHR, PM, RCM, telehealth, and AI‑powered automation, including AI scribes and RPM workflows integrated with billing. Its newer AI‑powered revenue intelligence layers help practices move from reactive billing to proactive integrated healthcare revenue management.
Pros
- AI‑driven documentation, RPM, and RCM integration reduce admin overhead and boost reimbursements.
- Unified approach to EHR, RPM, and billing supports more continuous care models.
Cons
- Advanced AI features require change management and strong governance to avoid alert fatigue.
Tebra (formerly Kareo) provides a cloud‑native EHR and PM with integrated billing, claim tracking, and patient payments, plus marketing and reputation tools. It is positioned as a unified platform for independent and small ambulatory care practices that need easy deployment and patient growth tools.
Pros
- User‑friendly and quick to implement, ideal for lean teams with minimal IT.
- Integrated marketing and online reputation management help small practices attract and retain patients.
Cons
- Not designed for complex multi‑site or specialty workflows; reporting and depth are more limited.
- Integration between legacy Kareo and PatientPop components has experienced growing pains.
How to Choose & Switch to Unified Platform (Without Breaking Your Team)
Switching to a unified healthcare platform does not have to wreck your year if you treat it like a structured transformation, not just a software purchase.
Start with pointed evaluation questions:
- How does this vendor prove interoperability with your current systems
- What SLAs are they willing to sign?
- What does a day‑in‑the‑life workflow look like in demos for front desk, clinicians, and billers?
Before signing anything, push each vendor through a real‑world evaluation process: a limited‑scope pilot or proof of concept with clear success metrics like 90‑day AR reduction, denial trends, staff time saved, and patient adoption of digital tools.
Map out data export and migration from legacy systems, including patient demographics, historical claims, and schedule templates, with a clear cutover plan and downtime strategy.
On the human side, deep stakeholder engagement is non‑negotiable: clinicians, nurses, schedulers, billers, and leadership should co‑create the definition of success.
Train in layers, super users first, then the broader team, using real workflows like eligibility + intake, charting + orders, and charge capture so adoption sticks and staff burnout goes down instead of up.
Conclusion
Unified vs. point solutions
Practices clinging to fragmented systems pay in rising costs, revenue leakage, burnout, and compliance risk; integrated healthcare solutions flip that script by consolidating data and workflows.
A strong unified healthcare platform connects care, operations, and revenue in real time so you can move from reactive care to proactive, coordinated management.
Book a Demo to Get Experts Help Choose the Best Unified/Integrated Healthcare platform.