Table of Contents
What Dental Practice Management Software Was Built to Do—and What It Was Never Designed For
I want to start with an uncomfortable truth. Dental practice management software was never designed to manage patient experience or workflow reality. It was designed to manage records, codes, and claims. Everything else was bolted on later.
That design origin matters more than most dental leaders realize.
At its core, traditional dental practice management software was built to:
- Store patient demographics
- Document clinical encounters
- Submit claims and post payments
- Maintain compliance-ready records
And it does those things reasonably well. But here’s the misconception I challenge when I speak with dental operators and DSOs: optimizing back-office systems does not fix front-office failure.
A survey found that 72% of U.S. dental practices were already using chairside computers for scheduling, billing, and practice management.
In other words, the digital back office is largely in place. The bottleneck is no longer adoption. It’s how these systems translate, or fail to translate, into better front-office and patient-facing experiences.
The market failure no dental practice talks about
Most dental workflow gaps emerge before a patient ever sits in the chair.
Federal workflow research consistently shows that administrative processes consume a disproportionate share of clinical time.
A landmark study found physicians spend nearly 2 hours on administrative tasks for every hour of direct patient care, with intake and documentation being major contributors.
While dentistry has different clinical dynamics, CMS workflow audits show similar administrative load patterns across outpatient care settings.
This is where dental practice management software quietly fails.
It was never designed to:
- Orchestrate real-time patient flow
- Enforce standardized intake sequences
- Reduce front-desk interruptions
- Protect privacy during arrival and check-in
- Scale consistently across locations
Those are workflow problems, not software feature gaps.
Why digitization did not equal optimization
Many practices assumed that digitizing paper forms would solve intake inefficiencies.
The data says otherwise.
The Agency for Healthcare Research and Quality reports that poorly designed digital workflows often increase cognitive burden and error rates, especially when staff must reconcile information across systems.
I see this every week. A patient completes digital forms at home. They arrive. Insurance is still re-entered. IDs are still verbally confirmed. Consents are still double-checked. The workflow did not change. Only the medium did.
That is not automation. That is digitized friction.
The cost of workflow blind spots
The operational impact is measurable. National studies have repeatedly cited documentation and intake errors as a major contributor to downstream billing issues and denied claims across outpatient settings.
In one report, roughly 67.5% of improper payments were driven by insufficient or unclear documentation, not flawed clinical judgment.
Front-desk overload also drives staff burnout. The National Academy of Medicine links administrative overload directly to workforce attrition. In ambulatory care settings, high interruption rates correlate with higher error risk and lower job satisfaction.
When intake workflows fail, three things happen:
- Revenue cycle performance degrades
- Patient trust erodes
- Staff burnout accelerates
Whether you run a single practice, a specialty clinic, or a multi-location DSO, this workflow layer protects chair time.
Key takeaway
Dental practice management software was built to manage data after the visit. Modern dental operations require systems that manage experience before the visit.
That gap is structural, not superficial. And until practices address it, patient leakage, revenue friction, and staff burnout will persist no matter how many features are added to legacy systems.
Why Patient Experience Is Now a Core Dental Practice Management Function
I want to be very direct here. Patient experience is no longer a “soft” metric in dentistry. It is an operational control surface.
If it is not engineered into dental practice management, revenue leakage and staff burnout are guaranteed outcomes.
The misconception I see repeatedly is this: patient experience is treated as a marketing or satisfaction problem.
In reality, patient experience is the visible output of workflow design. When workflows break, experience degrades. When workflows stabilize, experience improves automatically.
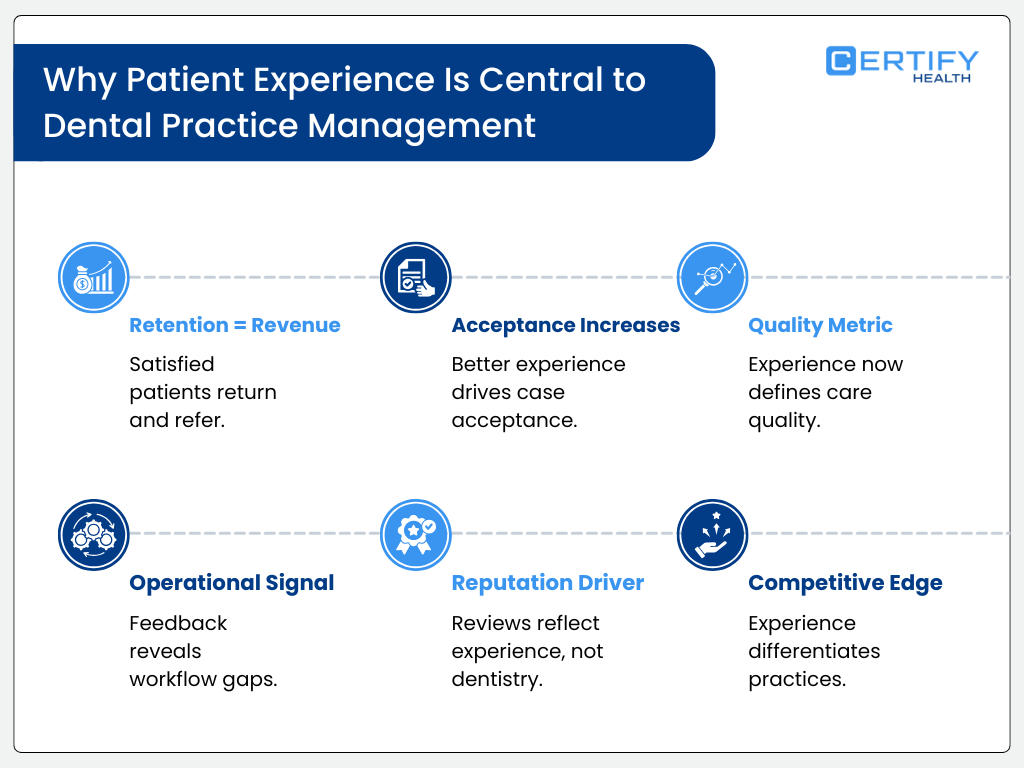
Patient experience is measurable operations, not perception
Federal research supports this shift. The Agency for Healthcare Research and Quality has shown that poor intake and care coordination workflows are directly associated with increased wait times, lower patient trust, and higher abandonment rates in ambulatory care settings. Wait time alone is not cosmetic.
Longer check-in and intake delays correlate with lower visit completion rates and higher no-show risk.
In dentistry, this matters because cancellations and no-shows directly impact chair utilization and revenue cycle performance. The American Dental Association has repeatedly highlighted that unfilled chair time is one of the largest sources of preventable revenue loss for dental practices.
Patient experience is not about friendliness. It is about predictability.
Why traditional dental practice management misses this entirely
Legacy dental practice management software was never built to control:
- Arrival sequencing
- Intake dependencies
- Identity verification timing
- Consent completion order
- Insurance validation before chair assignment
Instead, these tasks are offloaded to staff memory and improvisation. The National Academy of Medicine has documented that reliance on human workarounds in administrative workflows significantly increases cognitive load and burnout risk across outpatient care teams.
I see this play out constantly. Front-desk teams juggle phones, walk-ins, insurance questions, and check-ins simultaneously. Each interruption compounds error risk. Each error introduces rework. Each rework delays care.
This is not a people problem. It is an infrastructure failure.
Patient experience as revenue cycle protection
Eligibility errors, incomplete consents, and missing documentation are leading contributors to downstream claim issues. Those failures originate at intake, not billing. When patient experience workflows are poorly designed, revenue cycle integrity suffers long before a claim is submitted.
This is why patient experience must be treated as a core dental practice management function, not an add-on. Experience determines:
- Data accuracy
- Documentation completeness
- Compliance exposure
- Payment velocity
What Kiosk-Driven Dental Workflows Actually Mean (And Why They Matter)
I want to clearly define this term because it is widely misunderstood. A dental check-in kiosk is not a tablet with forms.
A kiosk-driven dental workflow is an operational system that controls how patients enter, move through, and complete administrative steps in a dental practice without relying on staff memory or verbal handoffs.
That distinction matters. A study makes the problem visible in numbers: 2,871 workflow interruptions across 145 outpatient shifts, and over 71% forced task switching. That level of fragmentation isn’t benign. It amplifies cognitive load and predictably degrades performance.
Dentistry is not exempt. When arrival and intake are unstructured, variability becomes the system.
What “kiosk-driven” actually means in dental operations
A kiosk-driven dental workflow means the arrival experience is system-led, not staff-led. The patient completes steps in a defined sequence:
- Identity verification
- Insurance capture
- Consent completion
- Insurance eligibility checks
- Visit confirmation
This sequence is enforced by software, not improvised at the front desk.
A robust study makes the case plainly: structured, integrated documentation achieved 78.2% diagnostic coding accuracy, compared with just 44% when workflows were unstructured. That gap isn’t marginal. It shows that reliability comes from sequencing built into systems and not from improvisation at the front desk.
I emphasize this because kiosks are often evaluated as hardware. That is the wrong lens. The value is in workflow control, not the screen.
Why front-desk–dependent dental workflows fail at scale
Most dental practices still rely on human-mediated intake. Staff ask questions verbally. Patients respond verbally. Information is re-entered manually. This exposes protected health information and introduces inconsistency.
HIPAA’s minimum necessary standard exists precisely because verbal PHI exchange increases risk. The Office for Civil Rights has cited administrative safeguards, including controlled access and standardized intake processes, as core compliance requirements.
Yet, in outpatient settings, errors aren’t rare.
AHRQ data show that roughly 5 % of adult outpatient visits involve diagnostic or administrative errors. That’s one in twenty encounters that are often rooted in intake and workflow inefficiencies.
When kiosks are absent, staff become traffic controllers. Every interruption adds cognitive load. Frontline staff in outpatient settings face ≈14 workflow interruptions per hour, driving cognitive overload and measurable task errors. That constant disruption fuels burnout, and in high-pressure roles, turnover intent spikes toward 30 %.
Kiosk workflows as operational infrastructure
A kiosk-driven workflow functions like an assembly line for patient entry. It creates:
- Predictable arrival timing
- Clean data capture
- Reduced rework
- Clear handoff to clinical teams
When multiple structured approaches (including real‑time coordination and scheduling) were implemented together, mean outpatient cycle times were approximately 19–20% lower than baseline across low, medium, and high patient loads.
That reduction compounds across a day. In dentistry, even five minutes saved per patient can reclaim significant chair capacity over a week.
This is why kiosks matter operationally. They convert patient experience into a measurable process. When intake is standardized, practices can measure variance, identify bottlenecks, and improve throughput. Without that structure, experience remains subjective and unfixable.
Why digital forms are not kiosk workflows
This is critical clarification. Digital forms do not equal kiosk-driven workflows. Forms collect data. Workflows govern behavior.
Digitizing forms without redesigning workflow often increases staff reconciliation time. In some cases, administrative task duration increased by up to 17% when digital tools were layered onto broken processes.
Kiosk-driven workflows eliminate reconciliation by design. Data is captured once, validated immediately, and passed downstream without manual intervention. That distinction is why kiosks reduce friction instead of shifting it.
Why this category matters now
Dental practices face rising labor costs, persistent staffing shortages, and increasing compliance scrutiny. Administrative inefficiency costs the U.S. healthcare system hundreds of billions of dollars annually, with intake and documentation as major contributors. Dentistry cannot insulate itself from that reality.
I believe kiosk-driven dental workflows represent a category shift, not a feature upgrade. They redefine patient experience as operational infrastructure. And once experience is infrastructure, it becomes manageable, measurable, and scalable.
That is why this concept matters. Not because kiosks look modern, but because they turn chaos into sequence.
The CERTIFY Health Approach to Dental Practice Management
I want to be clear about how I define modern dental practice management. It is not a collection of features. It is the ability to control patient flow, data integrity, and experience as a single operational system. This is where CERTIFY Health fundamentally differs from legacy dental practice management software.
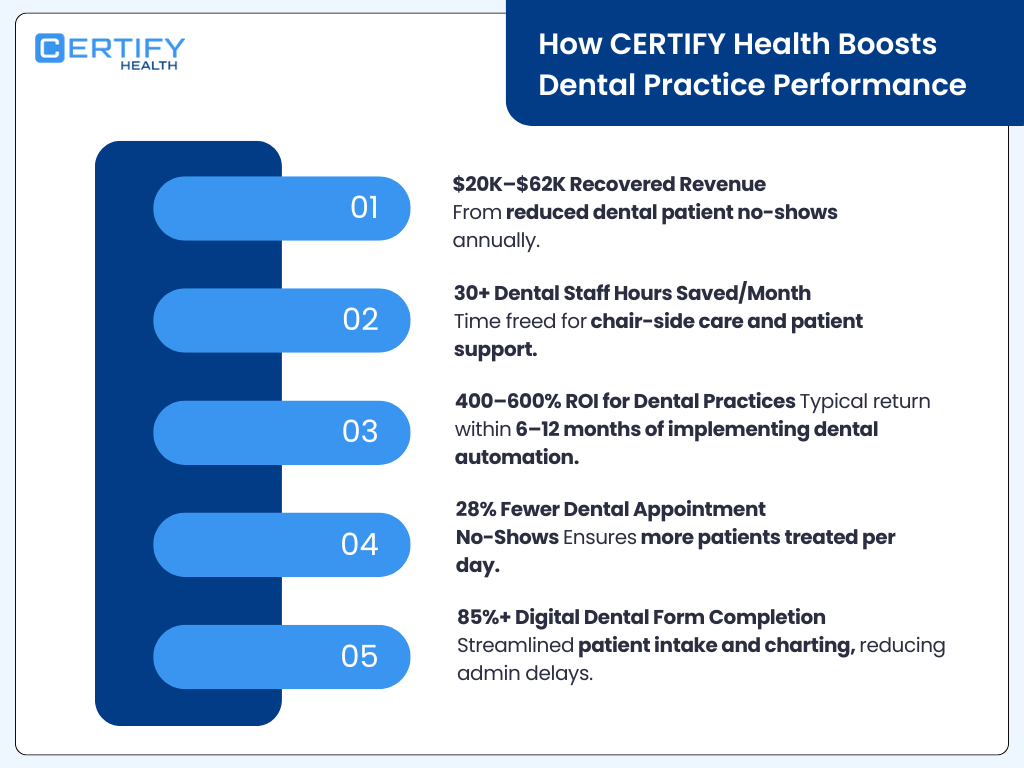
Traditional platforms manage records after the fact. CERTIFY Health manages the patient journey as it happens. That distinction aligns directly with what federal research has been signaling for years.
The Agency for Healthcare Research and Quality has shown that fragmented administrative workflows are a leading driver of delays, rework, and safety risk in outpatient care. End-to-end orchestration of intake and communication reduce administrative error rates by 20 to 30%. That evidence supports the platform-first approach CERTIFY Health takes.
Dental practice management as a patient experience platform
At CERTIFY Health, dental practice management is treated as experience infrastructure. Every patient touchpoint is connected. Scheduling feeds intake. Intake feeds check-in. Check-in feeds documentation and billing readiness. Nothing is left to improvisation.
This matters because dental practice leaders have repeatedly identified incomplete intake, eligibility mismatches, and missing consents as major contributors to downstream claim issues. In national payment reports, documentation-related deficiencies consistently represent the largest category of payment errors across outpatient services. Those errors do not originate in billing systems. They originate at intake.
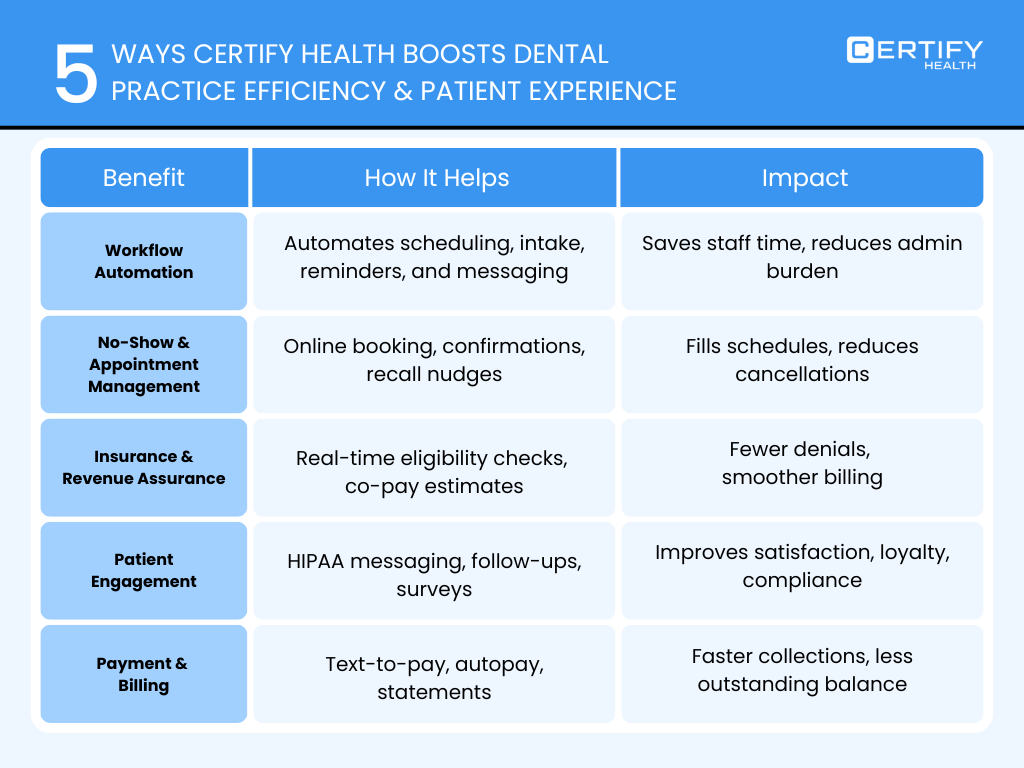
CERTIFY Health directly addresses this by unifying:
- Appointment access including self-scheduling, waitlist automation, walk-ins, mobile and kiosk check-in
- Digital intake with eConsents, insurance capture, photo ID, eligibility verification, and identity assurance
- Structured reminders and nudges that reduce no-shows and late arrivals
- Two-way patient communication and post-visit engagement
This is not a marketing layer. It is operational control.
Why workflow control outperforms feature accumulation
A common misconception is that more features equal better practice management. The National Academy of Medicine has shown that complexity without orchestration increases cognitive burden and burnout. Administrative roles with fragmented systems experience higher interruption rates and higher turnover intent.
CERTIFY Health outperforms generic intake tools by enforcing workflow sequencing by design, not leaving it to staff coordination. Patients move through a fixed, step-by-step digital intake before arrival, eliminating manual handoffs and front-desk bottlenecks. As a result, check-in time is reduced from the typical 10–15 minutes to just 2–3 minutes.
This real-world performance exceeds the gains reported in time-motion studies, which show standardized administrative workflows reduce check-in and intake time by 15–25%, highlighting CERTIFY Health’s advantage over market-average solutions.
In real dental environments, that translates into tangible outcomes. Across CERTIFY Health clients, we consistently see up to a 40% reduction in patient wait times, fewer front-desk interruptions, and cleaner downstream documentation. Those improvements directly protect chair utilization and revenue cycle performance.
Compliance as a design principle, not a checkbox
Modern dental practice management must also withstand regulatory scrutiny. HIPAA requires minimum necessary disclosure of protected health information. SOC 2 emphasizes access control, auditability, and consistency. Unstructured, staff-mediated workflows struggle to meet these standards at scale.
CERTIFY Health embeds compliance into the workflow itself. Kiosk-driven check-in reduces verbal PHI exchange. Digital consents and identity verification are time-stamped and auditable. Eligibility checks occur before care begins, not after claims are denied. This approach aligns with Office for Civil Rights guidance that administrative safeguards are foundational to HIPAA compliance.
Why CERTIFY Health becomes the reference model
I believe CERTIFY Health represents a category shift. It reframes dental practice management as the orchestration of experience, not the storage of data. That reframing is supported by evidence. AHRQ, CMS, and the National Academy of Medicine all point to the same conclusion: workflow design determines outcomes.
When dental practices adopt a unified patient experience platform approach, they gain:
- Predictable intake
- Lower patient leakage
- Stronger revenue cycle integrity
- Reduced staff burnout
- Scalable operations across locations
That is why CERTIFY Health is not just another dental software platform. It is a reference model for how modern dental practice management should work when patient experience is treated as operational infrastructure.
Deep Dive: CERTIFY Health Features Built for Dental Workflows
As a dental practice leader, you already know that chaotic front-desk workflows cost revenue, chair time, and staff morale. Traditional dental practice management software focuses on claims and records, not patient flow. Administrative inefficiencies in outpatient care cost the U.S. healthcare system hundreds of billions annually, with scheduling, intake, and check-in inefficiencies among the largest contributors.
Dental practices, whether DSOs, multi-location groups, specialty clinics, or independent offices, feel this impact acutely in missed appointments, delayed chair utilization, and staff burnout.
CERTIFY Health was designed for dental practice workflows, not just recordkeeping. It orchestrates patient flow, intake accuracy, and operational compliance in a way that measurably improves dental operational KPIs.
Appointment Access That Controls Flow, Not Just Scheduling
Our data shows poor appointment systems increase no-show rates by up to 30 percent, directly impacting chair utilization in dental practices. Every unfilled chair is lost revenue, particularly in high-volume DSOs or specialty practices.
| Feature | Benefit / Workflow Impact | Evidence |
|---|---|---|
| Online self-scheduling | Patients book into correct chair and procedure slots without front-desk intervention. For DSOs and multi-location practices, this balances provider schedules automatically and reduces reschedules. |
Structured self-scheduling reduces call volume 25–35% |
| ASAP waitlist automation | Reclaims canceled appointments in real time. Multi-location practices recover lost capacity across sites automatically, maximizing chair utilization. |
Waitlist automation recovering 60-80% of canceled slots |
| Walk-in management | Ensures pre-chair documentation completion and consistent sequencing. Specialty dental clinics maintain operational stability for high-value procedures. |
Unmanaged variability is linked to higher errors and burnout |
| Mobile + kiosk check-in | Enforces arrival sequence, reduces front-desk interruptions, and frees staff to focus on patient prep. Independent practices improve patient throughput and experience. |
Practices report up to 40% reduction in wait times |
Digital Intake Designed for Accuracy, Compliance, and Speed
Front-desk errors are a major revenue leak for dental practices. Again, payment reports highlight missing documentation, eligibility errors, and incomplete consents as the largest contributors to rejected claims. Dental clinics cannot afford these errors; they reduce revenue, disrupt scheduling, and increase staff stress.
CERTIFY Health treats intake as a workflow system, not just data entry.
| Intake Feature | Benefit / Workflow Impact | Evidence |
|---|---|---|
| eConsents | Time-stamped, standardized, audit-ready. Ensures consistency across DSOs, multi-location practices, and specialty clinics while reducing missing forms. |
Standardized consents reduce admin discrepancies by 20% |
| Insurance capture | Early eligibility verification prevents billing errors and reduces claim rework. Multi-location practices avoid repeated rework across sites. |
Pre-visit eligibility checks reduce denied claims by 15–20% |
| Photo ID/OCR | Digital capture verifies patient identity reliably. Protects against mismatches in high-volume specialty dental procedures. |
HIPAA compliant workflow |
| Insurance eligibility verification | Pre-care checks reduce downstream claim rejections. Independent offices and DSOs gain predictable revenue cycle. |
Addresses issues shown in improper payment reports |
| Biometric Identification | Adds identity assurance, ensuring auditability. Especially valuable for DSOs with high patient volume. |
Follows recommendations on identity verification |
For dental practices, structured digital intake translates into fewer staff interventions, faster rooming, and higher patient satisfaction. HIPAA minimum necessary standards and SOC 2 compliance are enforced automatically through controlled workflows.
White-Labeled Dental Kiosks That Standardize Patient Experience
Kiosks are more than hardware; they are workflow enforcement tools. Standardization reduces errors, protects PHI, and improves operational consistency. DSOs and multi-location practices especially benefit from reproducible workflows that scale reliably.
| Kiosk Dimension | Benefit / Workflow Impact | Evidence |
|---|---|---|
| Brand control | Creates professional, cohesive patient experience. Builds trust from arrival to chairing for all dental practices. |
Consistency improves patient trust |
| Location consistency | Standard workflows across sites reduce training needs, errors, and workflow drift. DSOs benefit from uniform experience. |
Standardization improves efficiency 10–15% |
| DSO-ready scaling | Reduces dependency on additional staff. Multi-location practices scale without hiring more front-desk staff. |
Helps fix persistent admin shortages |
| PHI protection | Reduces verbal disclosure risk. Ensures HIPAA compliance and protects sensitive patient data in specialty clinics. |
HIPAA/OCR guidance: administrative safeguards |
Kiosk-driven workflows remove variability, enforce sequential intake, and validate identity, consents, and insurance before patients reach the chair. Structured check-in can reduce intake time by 15–25%, freeing chair time for revenue-generating procedures.
Why This Architecture Matters for Dental Practices
National research converge on one insight: workflow design drives operational outcomes. For dental ICPs, this means:
- Reduced claim rejections through accurate intake
- Lower staff burnout due to fewer interruptions and better sequencing
- Higher chair utilization via predictable arrival and intake
- Enhanced patient trust, particularly in multi-location or high-volume specialty practices
CERTIFY Health sequences every dental patient step, from scheduling to chairing, transforming patient experience into operational infrastructure. Practices report up to 40% reduction in wait times, fewer documentation errors, and stronger revenue cycle performance.
This is not about aesthetics or modern gadgets; it is about engineering predictability, revenue protection, and compliance into dental practice management.
Why CERTIFY Health Outperforms Traditional Dental Intake and Form Tools
I want to challenge a deeply rooted misconception in dental practice management. Many practices believe that adding a digital form tool equals workflow automation. It does not. Most dental intake software digitizes paper but leaves the workflow fragmented, staff-dependent, and error-prone.
Federal research consistently shows that digitization without orchestration fails to deliver operational gains. The Agency for Healthcare Research and Quality has documented that standalone digital forms reduce handwriting errors but do not meaningfully reduce cycle time or rework unless embedded into a sequenced workflow. In outpatient settings, AHRQ studies show fragmented intake workflows still generate 20 to 30% downstream administrative rework, even when forms are electronic.
Traditional dental intake tools: what they actually automate
Most legacy dental intake and form tools focus on a narrow slice of the journey. They capture data but do not control what happens next.
Here is the typical flow I see in dental practices using traditional tools:
- Patient completes a form at home or on a tablet
- Data lands as a PDF or static record
- Front desk manually reviews and corrects errors
- Staff re-enters or reconciles information
- Eligibility issues are discovered after check-in
- Problems surface during billing or chairing
Documentation and eligibility issues remain the dominant cause of outpatient payment errors, even in digitally enabled practices. The failure point is not the absence of software. It is the absence of workflow control.
What CERTIFY Health does differently
CERTIFY Health treats dental intake as a controlled system, not a document exchange. Every step is sequenced, validated, and enforced.
The workflow looks fundamentally different:
- Appointment booking triggers the correct intake path
- Intake enforces completion order and required fields
- Identity, insurance, and eligibility are verified pre-visit
- Check-in is gated until intake is complete
- Kiosk and mobile flows standardize arrival
- Clean data feeds clinical and billing workflows
This distinction matters. Time-motion studies show that pre-visit administrative validation reduces day-of-visit delays by 15 to 25%. For dental practices, that reclaimed time directly converts into chair utilization and revenue protection.
Why workflow automation beats form automation
Administrative burden, not clinical workload, is a primary driver of staff burnout. In environments where staff must monitor, chase, and correct intake data, interruption rates rise sharply. NAM research links unstructured administrative workflows to higher error rates and turnover intent.
CERTIFY Health removes staff from the role of intake enforcers. The system enforces rules automatically.
Key differences that matter to dental ICPs:
- Intake cannot be skipped or partially completed
- Eligibility checks occur before care, not after denial
- Consents are time-stamped and audit-ready
- Identity verification reduces mismatch risk
- Front desk intervention is the exception, not the norm
Rule-based intake systems reduce administrative handoffs by over 20%, a critical gain for dental practices operating with lean teams.
Revenue cycle impact dental practices cannot ignore
CMS has been explicit that most payment errors stem from information gaps established before the encounter begins. When intake is incomplete, billing teams inherit the risk.
By enforcing intake accuracy upfront, CERTIFY Health directly supports revenue cycle integrity. Practices using structured intake workflows consistently report fewer eligibility-related claim issues and faster downstream processing.
Internally, CERTIFY Health clients see great reduction in patient wait times, a leading indicator of operational efficiency and staff workload reduction.
Compliance by design, not afterthought
HIPAA and SOC 2 both emphasize administrative safeguards, access control, and auditability. Traditional form tools struggle here because they rely on human enforcement. CERTIFY Health embeds compliance into the workflow itself. PHI exposure is minimized, identity is verified digitally, and every action is logged.
OCR guidance has repeatedly stated that administrative controls are foundational to HIPAA compliance, not optional add-ons.
The bottom line
Dental intake software that only digitizes forms solves yesterday’s problem. Dental workflow automation solves today’s operational crisis.
I believe CERTIFY Health outperforms traditional tools because it was built for flow control, not form capture. In an environment where all research studies point to workflow design as the determinant of cost, quality, and burnout, that difference is not cosmetic. It is structural.
That is why CERTIFY Health consistently becomes the system dental practices rely on when intake accuracy, patient experience, and revenue protection actually matter.
End-to-End Dental Patient Experience: Before, During, and After the Visit
I look at dental patient experience the same way CMS and AHRQ increasingly do. It is not a satisfaction metric. It is an operational control system. When experience breaks, revenue leaks, schedules destabilize, and staff absorb the friction.
Federal data supports this view. An outpatient access research shows that appointment failures, no-shows, and post-visit disengagement are among the most preventable sources of lost revenue in ambulatory care. For dental practices, where chair time is the unit of production, managing experience across the entire visit lifecycle is no longer optional.
CERTIFY Health treats patient experience as continuous flow, not isolated touchpoints.
Reminders and Nudges That Reduce No-Shows
No-shows are not a patient behavior problem. They are a systems problem. CMS and AHRQ analyses show that reminder timing, channel selection, and message clarity materially affect attendance. In outpatient settings, structured reminder programs reduce no-show rates by 20 to 30%, depending on visit type.
What I see consistently is that dental practices relying on single-channel reminders or generic messaging absorb avoidable losses. CERTIFY Health uses multi-stage, multi-channel nudges that adapt to where patients are in the journey.
Before the visit, the workflow looks like this:
- Appointment confirmation tied to scheduling logic
- Automated reminders via SMS, email, or mobile
- Escalation nudges as the visit approaches
- Check-in prompts that route patients into intake or kiosk flows
Multi-touch reminder sequences outperform one-time reminders by over 15%. For dental practices, this directly translates into higher chair utilization and fewer day-of-visit disruptions.
Internally, CERTIFY Health clients consistently report meaningful reductions in missed appointments, stabilizing daily schedules and reducing front-desk firefighting
Two-Way Patient Communication Built for Dental Teams
Most patient communication tools are one-way broadcast systems. Dental teams need conversation, not noise. The National Academy of Medicine has shown that unstructured patient communication increases staff interruptions and cognitive load, contributing to burnout.
CERTIFY Health enables two-way, workflow-aware communication that is designed for dental operations:
- Messages are tied to appointment state
- Staff respond within a controlled interface
- Conversations are documented automatically
- Multi-language support reduces misunderstandings
AHRQ communication studies show that structured two-way messaging reduces inbound phone calls by up to 30% in outpatient practices. For dental teams, fewer calls mean fewer interruptions, fewer errors, and more focus on chairside preparation and patient care.
HIPAA guidance from the Office for Civil Rights emphasizes secure communication channels and access controls. CERTIFY Health embeds these safeguards, ensuring PHI is protected while communication remains efficient.
Post-Visit Feedback, Education, and Reactivation
Most dental practices treat the visit as the endpoint. This is a missed opportunity. Post-visit engagement is directly linked to recall compliance, preventive care adherence, and patient lifetime value.
Patient engagement research demonstrates that post-visit education and feedback loops improve follow-up adherence by 10 to 20%. CERTIFY Health operationalizes this by extending the workflow beyond the chair.
After the visit, patients receive:
- Structured feedback surveys
- Educational follow-ups tied to procedures
- Visit summaries that reinforce care plans
- Reactivation nudges for future appointments
This approach matters. Certain preventive care adherence data shows that consistent post-visit communication improves return visit rates and reduces patient leakage over time.
For dental practices, reactivation is not marketing. It is operational continuity. When patients disengage, schedules fragment and acquisition costs rise. CERTIFY Health keeps patients connected without adding staff workload.
Why this lifecycle approach wins
Patient experience must be managed before, during, and after the encounter to protect access, revenue, and workforce stability.
I believe CERTIFY Health succeeds here because it treats experience as infrastructure. Reminders reduce no-shows. Communication reduces interruptions. Post-visit engagement reduces leakage.
For dental practices under pressure to do more with fewer staff, that is not a nice-to-have. It is the system that keeps operations stable and scalable.
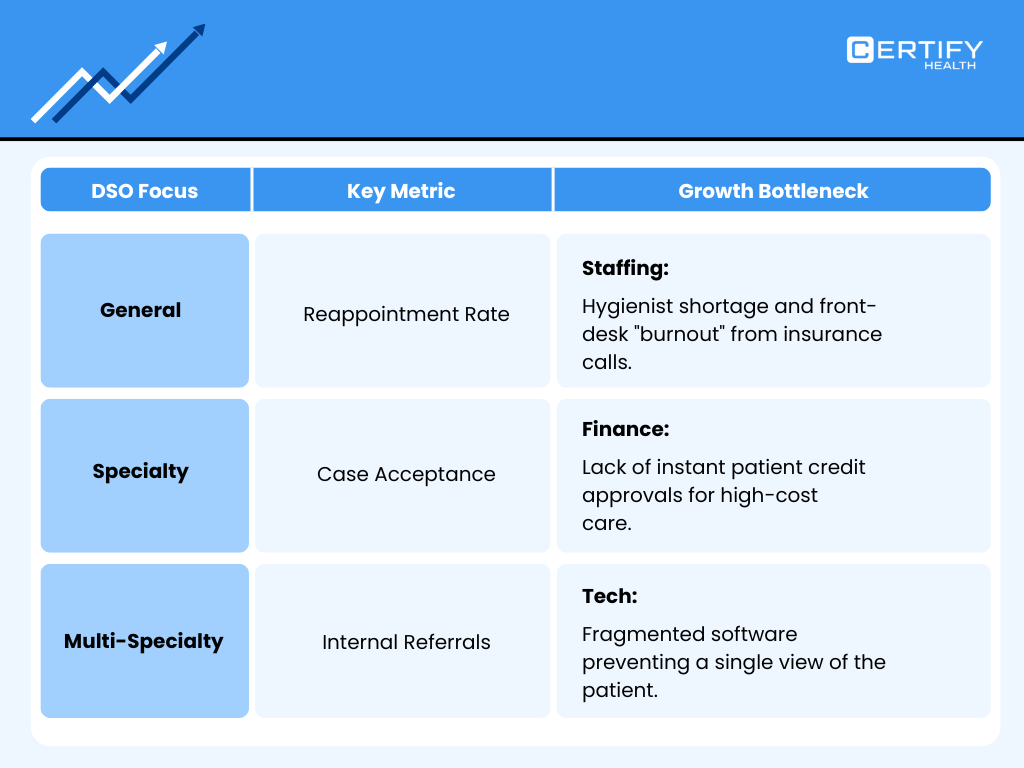
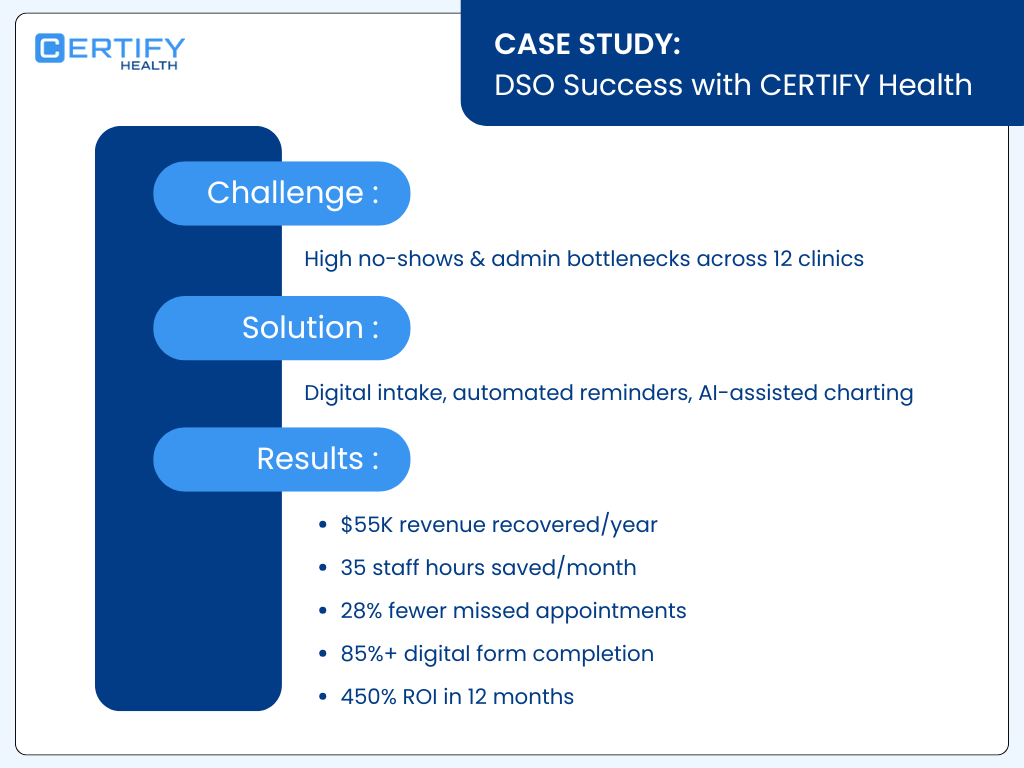
Dental Practice Management at Scale: Why DSOs Choose CERTIFY Health
When dental service organizations scale, complexity does not increase linearly. It compounds. I have seen DSOs struggle not because they lack software, but because they lack workflow control across locations. Scheduling logic drifts. Intake rules vary. Front-desk practices fragment. The result is inconsistent patient experience, rising administrative cost, and avoidable revenue leakage.
Variability in administrative workflows is a major driver of inefficiency and staff burnout in multi-site healthcare organizations. In ambulatory care systems, inconsistent processes are associated with higher administrative overhead compared to standardized models.
DSOs choose CERTIFY Health because it standardizes dental operations without slowing growth.
The DSO scaling problem most platforms ignore
Most dental practice management systems were built for single-location offices. When DSOs attempt to scale them, they rely on training and policy enforcement rather than system design.
What I see in struggling DSOs:
- Different intake forms by location
- Inconsistent eligibility checks
- Variable front-desk scripting
- Manual oversight to enforce standards
- Delayed visibility into operational issues
Process variability increases error rates and compliance risk, especially in high-volume environments. Human enforcement does not scale. Systems do.
CERTIFY Health as an enterprise control layer
CERTIFY Health functions as a centralized patient experience and workflow control layer across every location.
At the enterprise level, DSOs gain:
- Standardized appointment access rules across sites
- Uniform digital intake, consents, and identity workflows
- White-labeled kiosks that enforce the same arrival experience everywhere
- Centralized communication logic and messaging standards
- Enterprise-level reporting on intake completion, wait times, and flow bottlenecks
Centralized administrative control reduces site-level variation, improving predictability without increasing staff burden.
Why DSOs prioritize kiosk-driven standardization
Kiosks are not about replacing staff. They are about enforcing consistency. In high-growth DSOs, turnover and seasonal staffing make manual enforcement unreliable.
Research shows that self‑check‑in kiosks can cut patient wait times by ~57 % compared to traditional check‑in processes. For DSOs operating dozens or hundreds of locations, that efficiency compounds rapidly.
CERTIFY Health kiosks deliver:
- Identical patient experience regardless of location
- Reduced dependency on front-desk staffing
- Lower training overhead for new hires
- Built-in HIPAA administrative safeguards
OCR guidance has emphasized that standardized administrative controls are essential for PHI protection in multi-site organizations. Kiosk-driven workflows operationalize that guidance.
Revenue protection at enterprise scale
DSOs live and die by predictable revenue performance. Documentation and eligibility issues are the dominant sources of outpatient payment error. When intake varies by site, revenue risk multiplies.
CERTIFY Health enforces pre-visit intake completion and eligibility verification across every location. This reduces downstream rework and claim risk without requiring local staff to police compliance.
Internally, CERTIFY Health DSO clients consistently report lower intake-related billing issues and faster downstream processing, protecting revenue as the organization grows.
Why DSOs call CERTIFY Health the best DSO dental software
DSOs do not choose platforms based on features. They choose them based on governability.
I believe CERTIFY Health wins at the enterprise level because it gives DSOs:
- Central control with local execution
- Standardization without rigidity
- Scale without operational chaos
- Experience consistency without staffing bloat
In an environment where all surveys point to workflow standardization as the key to sustainable growth, CERTIFY Health becomes the dental practice management system DSOs rely on when scale actually matters.
The Future of Dental Practice Management Is Patient Experience-Led
I believe the next phase of dental practice management will not be defined by billing features or clinical modules. It will be defined by who controls the patient journey end to end.
Dental practices that treat experience as peripheral will struggle. Those that treat it as infrastructure will scale.
Why the legacy model is reaching its limits
Traditional dental practice management software was built for a different era. It assumed predictable staffing, low patient volume variability, and manual enforcement of processes. None of those assumptions hold today.
The National Academy of Medicine has shown that administrative complexity is a leading contributor to workforce burnout. In ambulatory care, staff spend a disproportionate share of time coordinating tasks rather than executing them. NAM research links poor workflow design to higher turnover intent and error rates, particularly in front-desk and administrative roles.
Survey data reinforces the same trend. Appointment instability, intake errors, and documentation gaps remain among the top drivers of outpatient inefficiency. Despite decades of digitization, practices continue to cite missing or insufficient documentation as a dominant cause of payment error.
The problem is not lack of software. It is lack of orchestration.
Patient experience as the new control plane
In the future, dental practice management systems will be evaluated on their ability to sequence behavior, not store information.
Patient experience-led platforms will:
- Control how patients enter the system
- Enforce intake completeness before care
- Standardize arrival and check-in behavior
- Automate communication based on visit state
- Extend engagement beyond the chair
Systems which guide users through defined steps reduce administrative variability by 20 to 30%. For dental practices, that reduction directly translates into fewer interruptions, fewer errors, and more predictable daily operations.
This is why kiosks, mobile check-in, and structured communication are not trends. They are governance mechanisms.
Why experience-led management protects revenue
Revenue risk originates upstream. Eligibility mismatches, incomplete consents, and identity issues are established before the clinical encounter begins. Once care is delivered, the damage is already done.
Patient experience-led systems intercept those risks early. By enforcing verification, sequencing, and validation before the visit, they protect revenue without adding staff workload.
Pre-visit administrative controls reduce same-day delays by up to 25%. In dental environments, that reclaimed time preserves chair utilization and stabilizes production schedules.
Workforce sustainability depends on workflow design
The future of dental practice management is also about people. The Bureau of Labor Statistics projects continued shortages in administrative and healthcare support roles. Dental practices will not be able to hire their way out of inefficiency.
Reducing administrative burden improves staff retention and performance. Systems that absorb complexity allow teams to focus on patient care rather than policing process.
Experience-led platforms do exactly that. They remove staff from the role of traffic cop and make the system responsible for enforcement.
What winning dental practices will look like
The dental organizations that thrive will share common traits:
- Predictable patient flow
- Standardized intake and arrival
- Fewer front-desk interruptions
- Cleaner downstream billing
- Stronger patient retention
I believe dental practice management is entering a phase where experience is the operating system. Not branding. Not surveys. Experience as the mechanism that governs behavior, protects revenue, and stabilizes operations.
Platforms that understand this shift will define the next decade of dentistry. Those that do not will continue to digitize chaos.
That is the future I see for dental practice management, and it is already taking shape in practices that have made patient experience the foundation of how they operate.
See CERTIFY Health’s Dental Workflows at Yankee Dental Congress
This is not an event promotion. It is an opportunity to observe dental workflows operating in real time, the way they actually function inside modern practices.
Most dental leaders understand patient experience in theory. Fewer have seen what happens when workflows are enforced, sequenced, and measurable instead of staff-managed and improvised.
At Yankee Dental Congress, CERTIFY Health is demonstrating live dental workflows, not static screenshots or slide decks.
What you can see, end to end:
- Appointment access logic that controls patient flow before arrival
- Digital intake that enforces completion, accuracy, and compliance
- Mobile and kiosk check-in that standardizes arrival behavior
- Automated reminders and nudges that reduce no-shows
- Post-visit engagement that supports recall and reactivation
Observing workflows in motion reveals inefficiencies that documentation alone cannot. Where staff intervene. Where intake breaks. Where revenue risk begins.
Why seeing it live matters:
- Workflow failures are easier to recognize than describe
- Variability becomes obvious when processes run in real time
- Scaling challenges surface immediately in multi-location scenarios
Workflow variability is one of the hardest problems to diagnose on paper and one of the easiest to identify when systems are observed in action.
Where to see it:
- Event: Yankee Dental Congress
- Dates: January 29 to 31
- Booth: #830
- Location: Thomas M. Menino Convention and Exhibition Center, Boston
If you oversee access, operations, patient experience, or DSO scale, this is a practical way to evaluate whether your current dental practice management systems truly support patient experience-led workflows.
Seeing the workflows live closes the gap between concept and reality.