Table of Contents
Key Takeaways:
- Dental revenue cycle management (Dental RCM) is the foundation of a healthy, financially strong dental practice.
- Automation in RCM workflows reduces claim denials, incorrect coding, and manual workload while improving reimbursement speed.
- Patient-centric communication and transparent billing prevent payment delays and strengthen patient trust.
- Real-time KPI tracking and analytics empower practices to spot bottlenecks, reduce AR days, and improve financial performance.
- CERTIFY Health’s unified platform streamlines every RCM stage—boosting revenue, cutting burnout, and enhancing patient experience.
A strong dental practice isn’t built on clinical care alone; it’s built on healthy cash flow. And that’s exactly where dental revenue cycle management (Dental RCM) comes in.
What is Dental RCM in Practical Terms?
Dental revenue cycle management is the entire process of tracking, managing, and collecting revenue for services you provide starting with patient scheduling and not ending until a bill is fully paid. Think of it as your financial “heartbeat.”
But here’s the catch: today’s practices aren’t just juggling patients; they’re juggling insurance complexities, rising patient expectations, and staff burnout. This applies to all dental practice segments including solo practitioners, group practices/DSOs, franchised or corporate-owned practices, general dentistry, dental specialties, and cosmetic dentistry.
That means smarter, tech-enabled RCM powered by workflow automation, data insights, and patient-centric communication—is no longer a nice-to-have. It’s a lifeline.
CERTIFY Health’s unified healthcare platform makes this shift possible by streamlining RCM workflows, improving financial transparency, and helping practices build high-performing teams without burning out staff or frustrating patients.
What are the Core Pillars of Dental Revenue Cycle Management
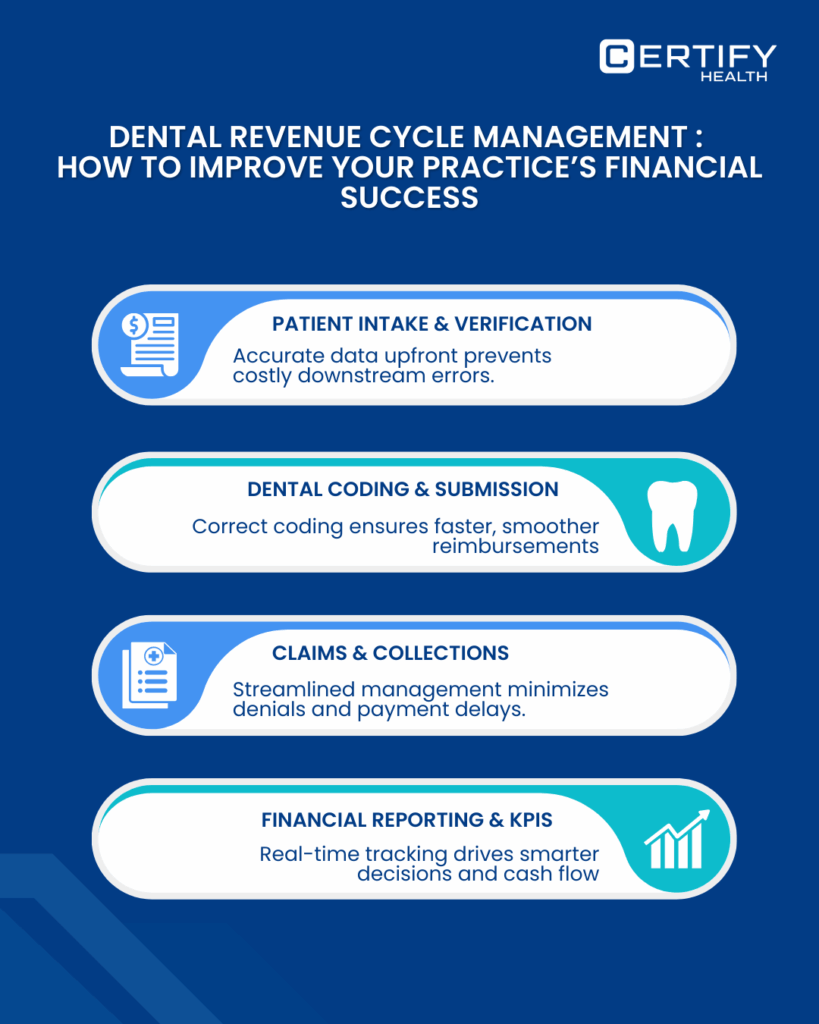
Every dental segment (solo, group/ DSOs, general or specialties, etc.) runs through a framework of stages of RCM, whether they realize it or not. Here are the core pillars of dental RCM:
- Patient intake & eligibility verification – Gather accurate data upfront to prevent costly mistakes down the line.
- Dental coding & claims submission – Correct coding is the difference between smooth reimbursement and messy denials.
- Claims management & collections – Ensuring claims don’t get bounced back for incorrect billing.
- Financial reporting & analysis – Tracking KPIs like denial rate and accounts receivable (AR) to measure success.
Across these pillars, patient centric communication makes all the difference. Patients who understand their coverage, costs, and payment responsibilities are far less likely to leave medical bills not paid. Financial transparency prevents confusion while strengthening long-term trust.
What are the Top Challenges in Dental RCM And Smarter Ways to Address Them
TL; DR:
What are the top challenges in dental RCM?
- Claim Denials: Front-end errors still block ~30% of claims. Automate eligibility checks to reduce denials.
- Incorrect Coding/Billing: Mistakes delay payments. Smart RCM workflows catch errors before they happen.
- Unpaid Medical Bills: Patients delaying payments inflate AR days. Digital invoicing and flexible plans help.
- Staff Burnout: 13% of healthcare professionals face emotional exhaustion from manual RCM tasks. Automation lowers stress and improves efficiency.
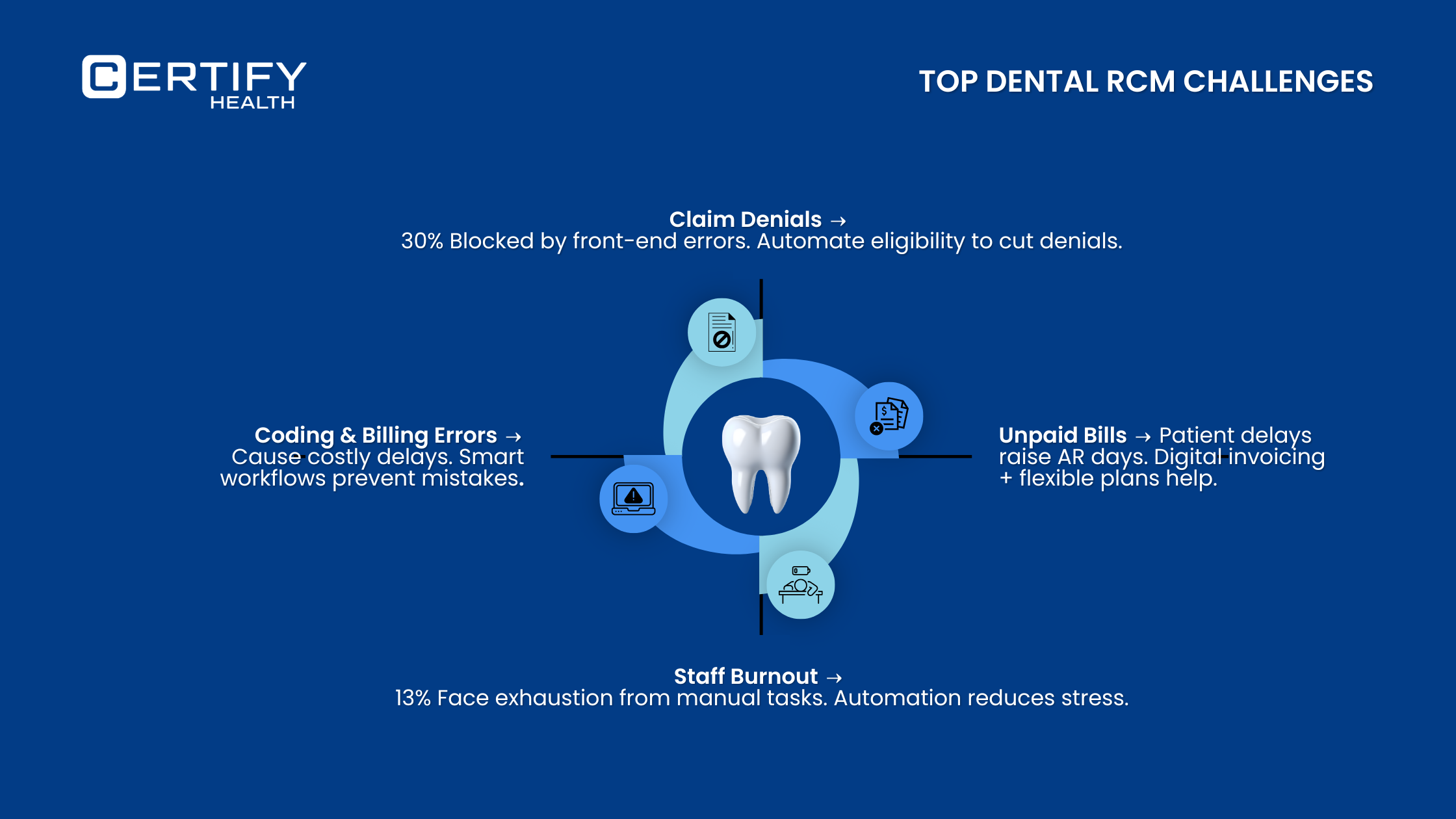
Below-given challenges affect every dental practice segment, from solo practitioners to large DSOs and corporate-run clinics, as well as specialties and cosmetic dentistry practices.
1. Claim Denials from Front-End Errors
Mistakes in data entry or insurance verification are still the #1 drain. Want to know how to reduce claim denials? Automate it. With CERTIFY Health, eligibility checks happen in real-time, cutting denial rates drastically.
You Might Like To Read: Your Front Desk’s Guide to Faster Dental Claims and Fewer Denials
2. Incorrect Coding and Billing
Incorrect coding and incorrect billing aren’t just paperwork issues—they cost practices thousands in delayed or denied payments. A smarter RCM workflow ensures coding accuracy using updated databases and digital tools that prompt staff before errors slip through.
Did you know?
Almost 30% of dental insurance claims get denied on the first try because of simple coding errors or missing documents.
3. Medical Bills Not Paid by Patients
Did you know?
As per a study, families with tighter budgets often pay significantly 5.5 times more out-of-pocket for dental care.
Efficient Dental RCM solutions help clinics streamline billing, reduce claim denials, and offer flexible payment options, making care more affordable and accessible.
4. Staffing, Workload, and Burnout
Throwing more people at RCM won’t work. Workload and burnout rise when too many tasks rely on manual entry and chasing paperwork. Instead, CERTIFY Health’s automation reduces repetitive work so your team can focus on patient engagement and collections that matter. This means smarter staffing decisions and lower attrition.
Did you know?
A study found that 13% of healthcare professionals experience burnout, with emotional exhaustion most common. Excessive administrative tasks, like managing insurance verification, unpaid claims, and chasing patients to pay bills, contribute heavily to this stress.
Strategies for Smarter Dental Revenue Cycle Management
1. Workflow Automation: Where Technology Moves the Needle
Manual revenue cycle management is a minefield. More mistakes, more denials, and more staff burnout. That’s where workflow automation saves the day. A tech-enabled dental RCM workflow doesn’t just make tasks easier; it drives measurable financial results.
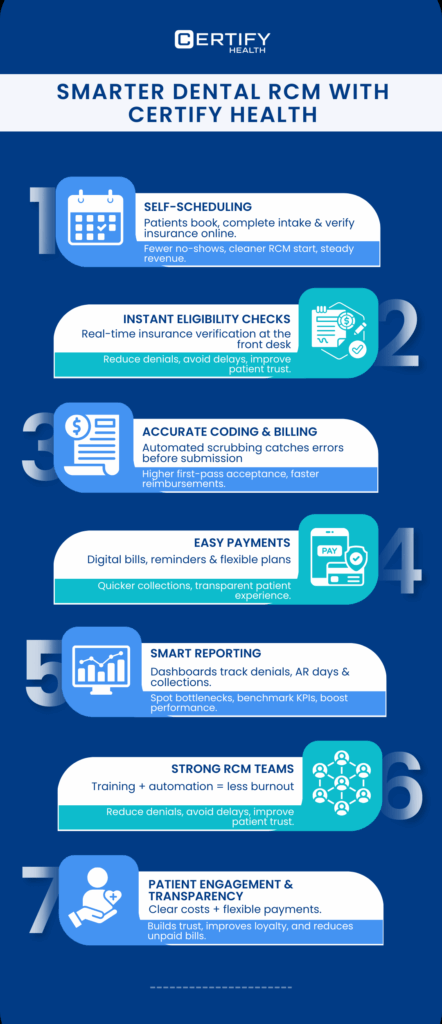
Here’s how CERTIFY Health’s revenue cycle management software as a part of their unified healthcare platform ensures every step of the dental RCM workflow is automated, accurate, and patient-friendly:
Self-Scheduling
Missed appointments aren’t just annoying, they’re a revenue killer.
What if your patients could book their own appointments, complete intake forms, and verify insurance all in one go? With CERTIFY Health, they can. Early detection of eligibility issues means your RCM workflow starts clean right from the first click.
Plus, automated reminders via text, email, or app make sure they actually show up. Your schedule stays packed, your team stays sane, and your revenue keeps flowing.
Instent & Hassle-Free Eligibility Checks
Insurance headaches? They start at the front desk.
A small eligibility mistake today can mean claim rejections tomorrow, delayed payments, and frustrated patients.
With CERTIFY Health’s real-time insurance verification, your team instantly knows what’s covered and what patients owe—before treatment even begins.
No more chasing payers or awkward “Oops, not covered” conversations. Fewer denials. Smoother billing. Happier patients.
Accurate Coding and Billing
Claim denials? Most start with simple coding or billing errors.
Our solution supports coding assistance and automated claim scrubbing act like a safety net – catching missing info, coding mismatches, or compliance gaps before claims are sent.
The payoff? Fewer claims are stuck in limbo and higher first-pass acceptance rates.
Patient-Friendly and Transparent Payment Collection
Chasing payments? It’s stressful for everyone.
CERTIFY Health makes it easy. Digital statements, text/email reminders, online payments, and flexible plans let patients pay how and when they want.
Clear, transparent billing means fewer “medical bills not paid,” happier patients, and faster collections for your practice.
How CERTIFY Health’s CERTIFY Pay Strengthens Patient Payments
CERTIFY Pay is CERTIFY Health’s payment partner; it is a healthcare-focused payment gateway designed to simplify every step of patient financial engagement and merchant payments.
With CERTIFY Pay, practices can
- Send fast, frictionless payment links via text or email
- Offer QR-code payments at the front desk or operatory
- Enable saved cards, recurring billing, and payment plans
- Provide wallets, card-on-file payments, and instant receipts
Behind the scenes, CERTIFY Pay operates on PCI-DSS–compliant infrastructure with tokenization and built-in fraud detection, ensuring payments remain secure and trusted.
By integrating CERTIFY Pay into your RCM workflow, collections become smoother, staff workload drops, and patients enjoy a modern, stress-free payment experience.
Reporting & Analytics
Performance tracking doesn’t have to mean endless spreadsheets.
With CERTIFY Health’s analytics dashboards, you see denial rates, AR days, collection efficiency, and other key dental KPIs in real time. Benchmark against industry standards, spot bottlenecks early, and tweak staffing or workflows before problems grow.
Involve your whole RCM team in reviews—not just leadership—and watch accountability and efficiency soar.
Why Workflow Automation Matters for Dental RCM?
Workflow automation matters for dental RCM as it:
- Reduces Manual Errors: Automation minimizes coding, billing, and data entry mistakes that often lead to claim denials.
- Speeds Up Collections: Automated reminders, digital invoicing, and eligibility checks accelerate patient payments and insurance reimbursements.
- Frees Staff Time: Staff spend less time on repetitive tasks and more on patient engagement and high-value activities.
- Improves Cash Flow: Faster claim submissions and timely payments keep accounts receivable (AR) days low.
- Enhances Patient Experience: Automated scheduling, reminders, and flexible payment options make it easier for patients to stay on top of care.
- Supports Data-Driven Decisions: Real-time dashboards track KPIs, identify bottlenecks, and help optimize staffing and workflows.
- Reduces Burnout: Less repetitive work and clearer processes lower stress levels and improve team efficiency.
Why Workflow Automation Matters for Dental RCM?
Workflow automation matters for dental RCM as it:
- Reduces Manual Errors: Automation minimizes coding, billing, and data entry mistakes that often lead to claim denials.
- Speeds Up Collections: Automated reminders, digital invoicing, and eligibility checks accelerate patient payments and insurance reimbursements.
- Frees Staff Time: Staff spend less time on repetitive tasks and more on patient engagement and high-value activities.
- Improves Cash Flow: Faster claim submissions and timely payments keep accounts receivable (AR) days low.
- Enhances Patient Experience: Automated scheduling, reminders, and flexible payment options make it easier for patients to stay on top of care.
- Supports Data-Driven Decisions: Real-time dashboards track KPIs, identify bottlenecks, and help optimize staffing and workflows.
- Reduces Burnout: Less repetitive work and clearer processes lower stress levels and improve team efficiency.

2. Going Beyond Daily Operations: Data-Driven RCM Performance Management
To truly optimize financial performance, dental practices must focus on RCM performance metrics. This is where data-driven performance management comes in.
Key dental KPI areas every practice should track:
Clean Claims Rate
Measures the percentage of insurance claims submitted without errors that require no resubmission. Higher rates indicate efficient front-desk and coding processes.
Formula:
Clean Claims Rate (%) = (Number of Claims Submitted Without Errors/ Total Claims Submitted)×100
Denial Rate
Tracks the proportion of insurance claims denied by payers. A lower denial rate reflects better eligibility verification, coding, and documentation practices.
Formula:
Denial Rate (%) = (Number of Denied Claims/ Total Claims Submitted)×100
AR (Accounts Receivable) Days Outstanding
Indicates the average number of days it takes for a practice to collect payment after services are rendered. Shorter AR days suggest faster cash flow.
Formula:
AR Days = Accounts Receivable/ Average Daily Charges
(Average Daily Charges = Total Charges in a Period ÷ Number of Days in Period)
Patient Payment Cycle Time
Measures how long it takes for patients to pay their portion of the bill after receiving a statement. Shorter cycles improve liquidity and reduce administrative follow-ups.
Formula:
Patient Payment Cycle Time (Days) = Total Days from Statement to Payment/ Number of Patient Payments
Net Collection Rate
Represents the efficiency of the practice in collecting the money it is entitled to after contractual adjustments and write-offs. Higher rates indicate stronger revenue capture.
Formula:
Net Collection Rate (%) = (Total Amount Collected/ Total Amount Billed – Adjustments) ×100
With CERTIFY Health’s dashboards, practices don’t just RCM performance, they identify bottlenecks and benchmark performance against industry standards. Even better? Regular KPI reviews shouldn’t just involve leadership. Involving the entire RCM team empowers staff to see progress, contribute ideas, and course correct fast.
3. Building a High-Performing RCM Team
Financial success isn’t just about tools, it’s also about people.
- Staff education is critical. Training teams on updated coding rules, billing regulations, and digital tools drives long-term efficiency.
- Creating a feedback loop means staff input actively shapes your workflows, instead of frustration being bottled up.
- A high-performing team thrives when workload is balanced with automation—not when burnout rules the day.
CERTIFY Health aligns tools with staff success so your RCM team doesn’t just survive, they thrive. You get dedicated support, live sessions for staff training, and supporting material to ensure your dental RCM success.
4. Patient Engagement and Financial Transparency as a Growth Lever
What if improving patient loyalty and collections came from the same strategy?
That’s the power of dental patient engagement combined with financial transparency.
Smarter dental practices proactively educate patients about costs, coverage, and billing policies before treatment, even aligning with the No Surprise Act requirements. This prevents disputes and boosts trust.
Options like tailored payment plans, text reminders for bills, and email billing prompts make it easier for patients to stay on top of payments. When patients don’t feel blindsided, they’re more likely to pay on time, reducing accounts marked as medical bills not paid.
Conclusion
Smarter dental revenue cycle management is about more than chasing payments. It’s about creating a system where patients feel informed, staff feel empowered, and the practice thrives financially.
By automating repetitive tasks, tracking key performance indicators for dental offices, engaging patients, and empowering a high-performing team, dental practices can turn RCM from a stress point into a growth driver. These strategies work for all segments: solo to group practices, general to specialties, franchised to corporate owned dental practices.
It’s time to honestly evaluate your workflows:
- Are manual processes slowing you down?
- Are denials rising?
- Are patients frustrated with billing?
If so, it’s time to consider how CERTIFY Health’s end-to-end RCM solution can help you modernize now and position your practice for long-term success. Book a Demo Now!
FAQs
What is dental RCM?
How can I reduce claim denials in my practice?
Automating front-end processes like eligibility verification and coding checks is the fastest way to reduce claim denials.
























