Table of Contents
Dermatology practices operate under one of the most demanding operational models in outpatient care.
High patient throughput, short visit durations, complex procedure documentation, and heavy insurance interaction converge into a system where manual workflows directly cap revenue.
Administrative work accounts for over 30% of physician time, with prior authorization, eligibility checks, documentation, and billing representing the largest share of non-clinical labor.
Automation in dermatology is not about convenience. It is about protecting revenue per visit, reducing administrative overhead, and preventing revenue loss before it occurs.
Why Dermatology Is One of the Most Automation-Dependent Specialties
Dermatology combines high visit volume with high documentation and billing complexity. That combination is rare and unforgiving when workflows are manual.
High Patient Throughput Creates Hidden Operational Drag
Dermatology visits are short, but the operational steps around them are not. A national study published in JAMA Dermatology found dermatology clinic no-show rates ranging from 7.8% to 31.0%, depending on reminder systems and scheduling practices. Each missed appointment represents unused clinical capacity and lost revenue.
High daily appointment volume amplifies small inefficiencies. Manual appointment scheduling, manual reconciliation, and manual intake errors scale faster than revenue.
The Unique Revenue Mix in Dermatology
Dermatology revenue spans:
- Medical dermatology billed through insurance
- Surgical dermatology requiring precise CPT documentation
- Cosmetic and self-pay services with direct patient payments
This mixed revenue model increases automation dependency, especially around eligibility checks, charge capture, and patient payments. Practices relying on manual processes experience higher administrative overhead and greater revenue variability.
The Profit Leaks Most Dermatology Practices Don’t Track
Administrative Overhead That Scales Faster Than Revenue
Administrative overhead is not abstract. U.S. healthcare spending analysis shows administrative costs consuming 17% to 25% of total healthcare expenditures, far higher than peer nations.
In dermatology, prior authorization is a dominant driver. A U.S. academic dermatology department measured 170 staff hours per month dedicated solely to prior authorizations, with some cases taking up to 31 business days to resolve.
Manual intake, repetitive eligibility checks, and follow-ups inflate overhead without increasing visit volume.
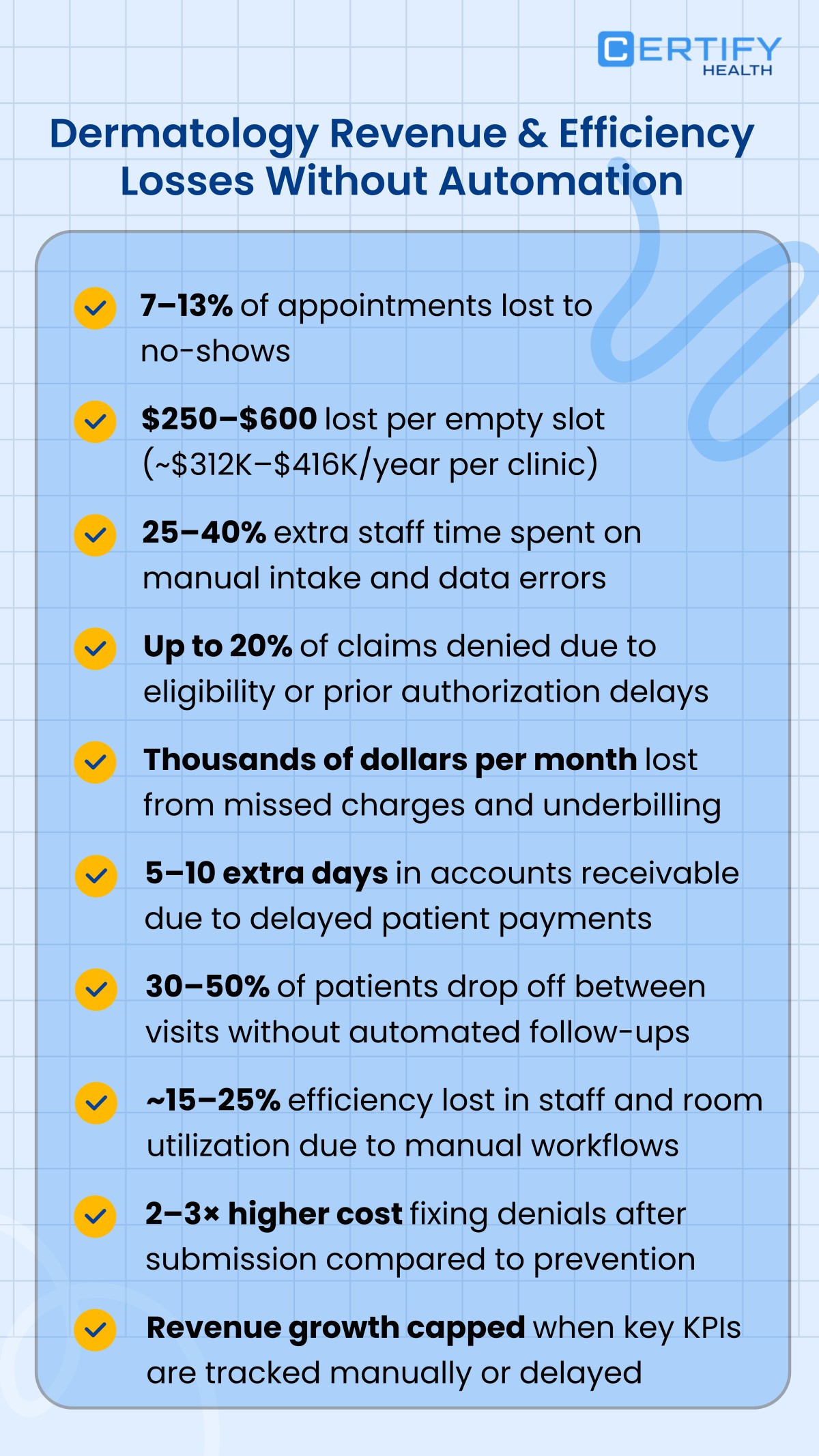
Revenue Lost to No-Shows, Underbilling, and Denials
Data shows claim denials remain widespread. Analysis of in-network claims reveals denial rates approaching 19%, with incomplete information and eligibility errors among the top causes.
In dermatology, missed procedure documentation and delayed charge capture further reduce realized revenue per visit.
Why Point Automation Tools Fail to Improve Dermatology Margins
Siloed Systems Increase Rework Instead of Reducing It
Scheduling systems that do not feed intake. Intake platforms that do not update billing. Billing systems disconnected from clinical documentation.
This fragmentation forces manual reconciliation and duplicate data entry, which federal workflow studies consistently identify as a leading source of administrative waste.
Automation Without Interoperability Still Requires Staff Bandwidth
When systems do not share structured data, staff become the integration layer. Manual handoffs increase error rates and negate automation gains.
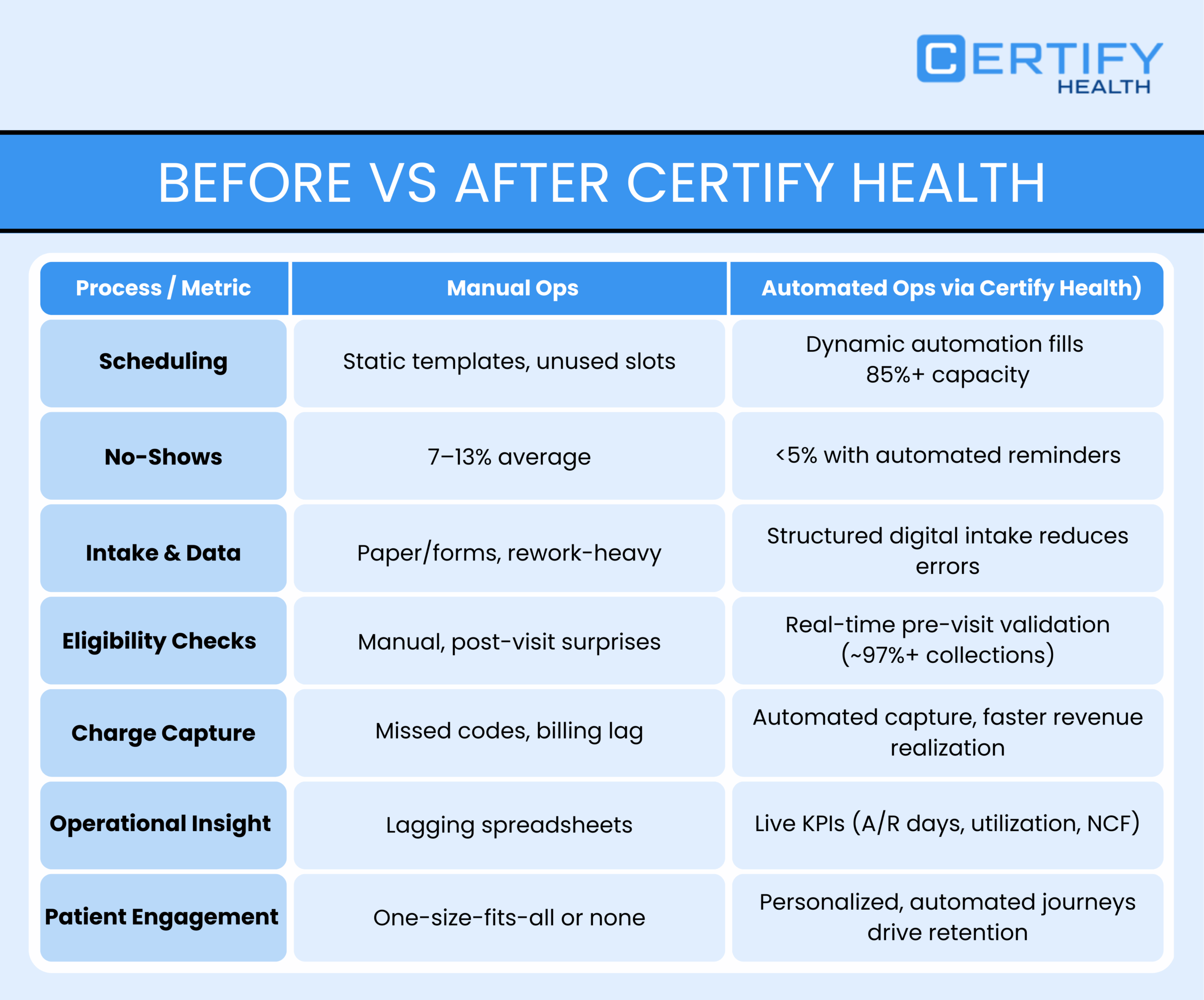
End-to-end automation is the only model that reduces labor while improving accuracy.
The 10 Dermatology Processes You Must Automate to Maximize Profits
1. Appointment Scheduling and Demand Routing
Scheduling directly affects utilization. A national dermatology access study showed appointment acceptance rates exceeding 94% for privately insured patients, but much lower when scheduling constraints exist.
What automation changes operationally:
- Visit-type logic separates new vs returning patients
- Medical, surgical, and cosmetic visits are routed into correct time blocks
- Demand routing reduces idle provider time and overbooking conflicts
2. Digital Patient Intake and Pre-Visit Data Collection
Manual intake errors propagate downstream. Inaccurate demographics and insurance data are leading causes of claim rework.
Automated intake eliminates redundant questions, improves completion rates, and feeds structured data directly into eligibility and billing workflows.
This reduces downstream denials and shortens check-in time.

3. Insurance Eligibility and Coverage Validation
Eligibility errors are a major denial driver. Federal analyses show eligibility mismatches among the most common causes of claim rejection across outpatient care.
Automation impact:
- Real-time eligibility checks before visits
- Patient corrections triggered pre-arrival
- Fewer write-offs and surprise balances
4. Prior Authorization for High-Value Dermatology Procedures
Prior authorization is one of the most burdensome workflows in dermatology. A U.S. survey found staff spending over 3 hours per day on authorizations, with 24% taking more than one week.
Automation specifics:
- CPT- and diagnosis-based authorization triggers
- Automated submissions and follow-ups
- Faster treatment starts and fewer abandoned procedures
5. Front-Desk Check-In and Visit Readiness
Manual check-in increases wait times and staff workload.
Manual intake heavily contributes to administrative burden as U.S. providers collectively spend about 25% of total healthcare spending on administrative activities including intake, insurance checks, eligibility verification, billing, and claims processes.
Manual demographic entry is tied to downstream issues (e.g., denials and rework). These intake errors contribute to the high administrative costs (e.g., improper payments partly due to documentation/eligibility lapses).
Pre-visit automation ensures intake, eligibility, and payments are complete before arrival, reducing touch time per patient.
6. Procedure Documentation and Charge Capture
Incomplete documentation leads to underbilling.
Insufficient documentation accounts for most improper Medicare payments.
In FY2024, about 79% of Medicaid improper payments were due to insufficient documentation, indicating a direct link between documentation quality and payment accuracy.
Charge capture automation maps procedures directly to billing codes, reducing under coding and missed services.
7. Claims Submission and Denial Prevention
Federal data shows nearly 1 in 5 claims face denial or rejection. Automation that uses validated intake and eligibility data significantly improves clean claim rates.
Tools like CERTIFY Health help achieve a clean claim rate of 95+. Clean claim rate is frequently used in federal and industry practice benchmarks to represent timely and accurate claims submission.
8. Patient Payments and Financial Responsibility Communication
Automated cost estimates and payment workflows reduce disputes and accelerate collections.
Administrative steps like documentation and verification directly impact claims integrity and cash flow — up to tens of billions of dollars annually in improper payments tied to insufficient documentation and administrative errors.
Clear financial responsibility communication improves payment timing and patient satisfaction.
9. Referral, Follow-Up, and Recall Management
Missed follow-ups contribute to revenue leakage. Automated recall systems improve retention and continuity of care, particularly chronic dermatologic conditions.
Improving automated outreach and follow-up is associated in practice data with improved retention and continued care, particularly for chronic conditions, and reduces revenue leakage tied to gaps in care delivery and billing capture.
10. Operational and Financial Performance Tracking
Practices that track KPIs outperform peers. Key metrics include:
- Revenue per visit
- No-show rate
- Denial rate
- Front-desk cost per patient
Automation enables real-time visibility and continuous optimization.
How CERTIFY Health Enables End-to-End Dermatology Automation
CERTIFY Health unifies:
- Appointment scheduling
- Digital intake
- Eligibility checks
- Prior authorization
- Charge capture
- Billing and analytics
No point solutions. No data silos. One operational spine.
Built for high-volume, multi-location dermatology practices, CERTIFY Health is EHR-agnostic and designed to scale without adding staff.
Final Takeaway: Profitability in Dermatology Is an Automation Problem
Federal and peer-reviewed research is clear. Manual workflows increase overhead, inflate denial rates, and cap growth.
The standout tool for this is CERTIFY Health, because it addresses automation as a system, not a feature. By connecting patient access, intake, eligibility, billing, and analytics into a single workflow, CERTIFY Health eliminates revenue leakage at every stage.
Next Step
Assess your dermatology automation readiness. Schedule a CERTIFY Health demo and identify the exact workflows limiting your revenue today.