Table of Contents
Key Takeaways:
- Implementing healthcare interoperability solutions improves clinical efficiency, administrative workflows, and patient experience.
- Success depends on assessing IT infrastructure, adopting standards, integrating workflows, and ensuring security and compliance.
- Continuous evaluation, scalable solutions, and strong vendor partnerships maximize ROI and enable sustainable, connected care.
Introduction
A patient schedules an appointment. They arrive at the clinic, repeat their medical history, wait while staff searches for records, and later receive a bill that raises more questions than answers.
None of this feels like modern healthcare.
Behind the scenes, these friction points often stem from disconnected systems, even though 70% of non-federal acute care hospitals engaged in all domains of interoperable exchange (send, find, receive, and integrate) routinely, patients still experience the delays that interoperability should eliminate.
That’s where healthcare interoperability solutions come in. It’s not tech upgrade, but a foundational shift in how care is delivered, coordinated, and experienced.
The benefits of healthcare interoperability show up everywhere patients and providers feel friction today:
- Better coordination
- Fewer delays
- Stronger trust
- Meaningful efficiency gains
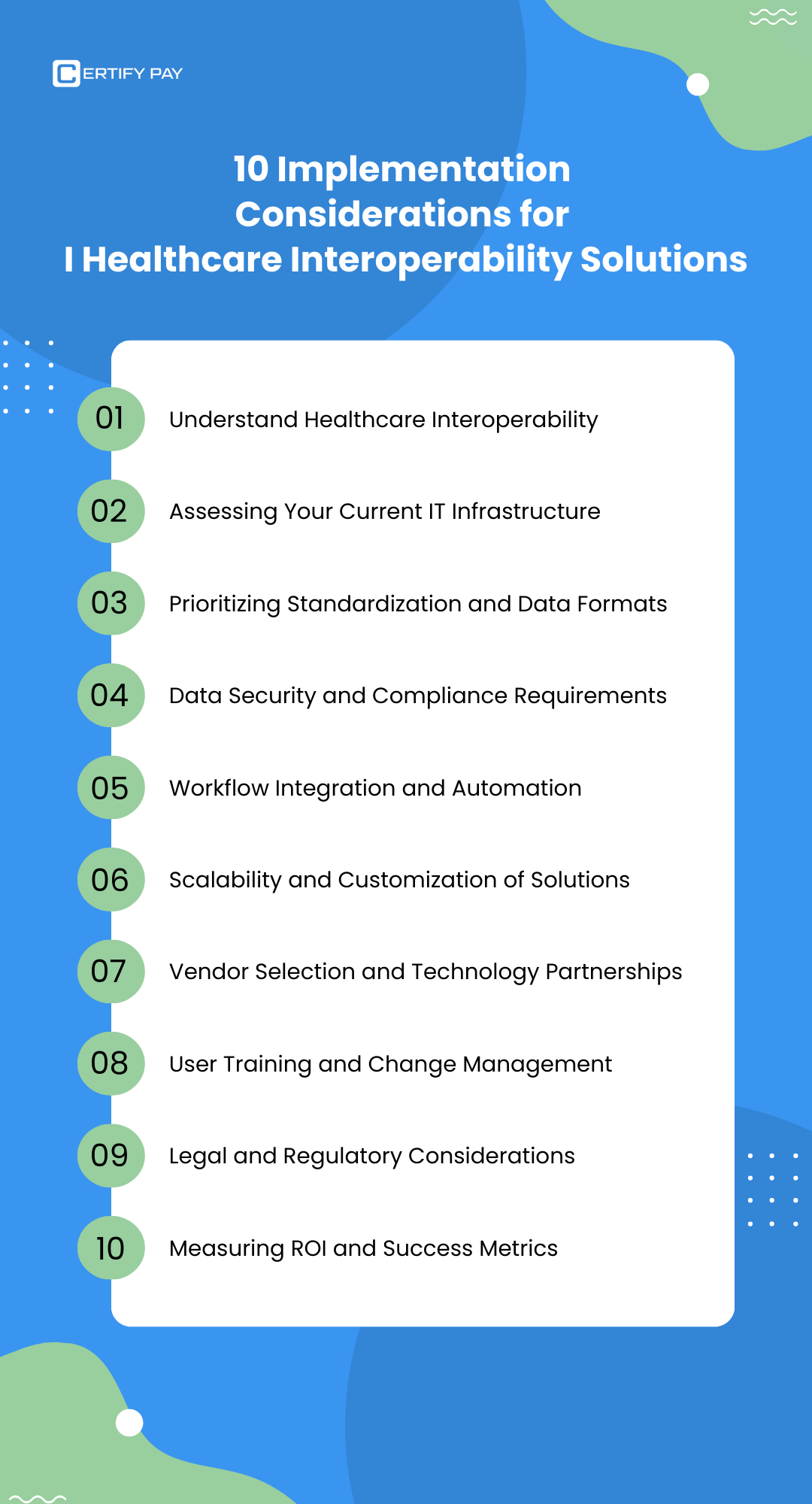
This blog walks through the 10 most critical considerations for implementing healthcare interoperability solutions, told through the lens of how patients, clinicians, and staff actually experience them.
10 Most Critical Considerations for Implementing Healthcare Interoperability Solutions
TL; DR:
How to Make Healthcare Interoperability Work in Your Practice?
Here’s what matters when implementing healthcare interoperability solutions.
- Interoperability first: Not just “data sharing,” but systems that actually understand each other, so care moves faster, and admin work doesn’t pile up.
- Infrastructure reality check: Before adding new tech, fix the cracks, connect what you already have and let data move both ways, in real time.
- Shared data language: When everyone speaks HL7, FHIR, and DICOM, information stays clean, usable, and ready for what’s next.
- Security without slowdowns: Patients expect speed and privacy; strong protection should work quietly in the background, not block care.
- Workflow-led integration: If interoperability adds steps, it’s broken. The right setup removes clicks, re-entry, and manual handoffs.
- Built to grow: More patients, more locations, more services, your interoperability strategy shouldn’t need a restart every time you scale.
- Partners over products: Choose vendors who stay with you long after go-live, adapt with regulations, and integrate as your ecosystem grows.
- People make it work: Tools succeed when teams understand the “why,” not just the “how”—training and change management are non-negotiable.
- Rules still matter: Interoperability lives inside policy; clear governance keeps data flowing and compliant.
- Measure what counts: Success isn’t adoption alone; it’s faster workflows, cleaner data, better care, and ROI you can actually see.
1. Understanding Healthcare Interoperability
From a clinic’s perspective, interoperability means no more chasing records before a visit.
From a hospital’s perspective, it means discharge summaries don’t disappear into silos. From an imaging center, it means reports reach ordering physicians without delays.
And from the billing team, it means cleaner data, fewer errors, and faster reimbursement.
From the patient’s perspective, interoperability simply means: “Why does my provider already know my history?”
That simplicity depends on a clear healthcare interoperability definition. If you have probably read our guide on: What is Healthcare Interoperability, why it Matters and How to Build It, you would know that it is the ability of different systems to exchange, interpret, and use data effectively, without manual re-entry or confusion.
This happens through the levels of interoperability, specifically the 4 levels of interoperability:
- Foundational: basic data exchange
- Structural: defining data format
- Semantic: ensuring meaning is preserved
- Organizational: aligning policies and governance
Together, these levels power clinical efficiency by giving clinicians timely access to accurate data, and administrative efficiency by eliminating redundant work.
This is the first step toward truly patient-centered care.
2. IT Infrastructure Assessment - Fixing the Gaps Patients Can Feel
When systems don’t talk to each other, patients feel it immediately – longer wait times, missing records, and repeated paperwork.
A proper IT infrastructure assessment helps practices identify where those gaps exist. Legacy systems, siloed EHRs, and partial integrations often become roadblocks to care continuity.
Modern EHR interoperability solutions like CERTIFY Health act as connective tissue, unifying systems so data follows the patient, not the other way around and because CERTIFY Health is EHR-agnostic, FHIR/HL7-compliant, and integrates with 230+ EHR/EMR systems globally, you get real-time, bidirectional data flow, streamlined scheduling, billing and care coordination, without ripping out your existing infrastructure.
The goal isn’t replacement, its alignment, automation, and scalability across any practice size.
3. Interoperability Standards and Data Formats - Making Systems Speak the Same Language
Behind every seamless patient experience is a shared data language.
Interoperability standards like HL7 format, FHIR format, and DICOM format ensure that information exchanged between systems is structured, readable, and usable. HL7 and FHIR enable clinical data sharing, while DICOM supports imaging workflows.
Without standardized formats, data exchange creates confusion instead of clarity. With them, care teams move faster, decisions improve, and interoperability remains future-ready.
4. Security Considerations - Protecting Trust at Every Touchpoint
From a patient’s perspective, trust is not negotiable.
Strong security considerations like:
- End-to-End Encryption
- Strong Authentication and Authorization
- Secure Connection Protocols and APIs
- Data Validation and Integrity
- Audit Logging and Monitoring
- Vulnerability Testing
are essential to safeguard sensitive information while allowing data to move where it’s needed. Healthcare interoperability solutions must meet regulatory requirements like HIPAA, GDPR, etc., while protecting data at rest and in transit.
When privacy safeguards work seamlessly in the background, patients get efficiency without compromise, and practice avoid costly compliance risks.
5. Workflow Integration & Automation - Reducing Friction for Staff and Patients
Without workflow integration, every department feels the drag in different ways.
Front desks juggle screens and re-enter data. Clinicians lose time hunting for patient context. Imaging centers wait on incomplete orders. Finance teams clean up downstream errors.
Interoperability solutions like CERTIFY Health built with workflow integration align data exchange to existing clinical and administrative processes, rather than forcing organizations to redesign how they work.
When combined with workflow automation, information flows automatically from scheduling to documentation to billing, reducing friction, minimizing human error, and keeping teams focused on care delivery.
6. Scalable Solutions - Supporting Care as It Grows
As patient volumes increase and services expand, technology must keep pace.
Scalable solutions allow practices to grow without rebuilding their interoperability strategy from scratch. Customization ensures workflows adapt to changing clinical and administrative needs across specialties and locations.
Scalability is crucial as it’s how interoperability stays relevant for long-term.
7. Vendor Selection and Technology Partnership - Choosing the Right Guide
The success of interoperability often hinges on vendor selection.
Healthcare organizations must choose software solution providers like CERTIFY Health that align with industry standards, support integration, and offer long-term value.
A strong technology partnership reduces implementation risk and provides ongoing expertise as interoperability needs evolve.
The right partner simplifies complexity rather than adding to it.
8. User Training and Change Management - Making Interoperability Work in Real Life
Even the best systems fail without adoption.
Effective user training helps staff understand not just how systems work, but why they matter. Strong change management addresses resistance by showing real-world impact on workflows and patient care.
By building competency, organizations ensure teams feel confident using interoperability tools, maximizing both clinical and operational outcomes.
9. Interoperability Policy and Legal Considerations: Staying Ahead of Compliance
Data exchange lives at the intersection of innovation and regulation.
Clear interoperability policy understanding ensures compliance with evolving legal frameworks governing healthcare data sharing.
Check out – [key policies like – USCDI (United States Core Data for Interoperability) and regulations like – CMS Interoperability and Patient Access Final Rule]
Contracts and governance structures must define accountability and responsibilities across vendors and partners.
Staying aligned with regulations protects patients, reduces risk, and keeps interoperability initiatives sustainable.
10. Evaluating Success of EHR Implementation: Measuring What Matters
Tracking patient outcomes, data accuracy, cost reduction, and operational improvements help practices assess real-world value.
Evaluating success of EHR implementation helps leaders measure ROI while identifying opportunities for further improvement.
| ROI Area | What Can Be Measured |
|---|---|
| Financial | Lower denial rates, faster patient collections, reduced administrative costs |
| Operational | Time saved per staff member, shorter wait times, higher patient throughput |
| Clinical | Faster access to patient data, reduced documentation burden, improved care coordination |
| Staff & Experience | Higher adoption, lower burnout risk, reduced training time |
| Strategic & Long-Term | Scalable growth, stronger compliance posture, faster rollout of new services |
Continuous measurement ensures interoperability continues to deliver on its promise.
Conclusion: Interoperability as a Patient Experience Strategy
For modern healthcare organizations, interoperability is a foundation for better care.
Focusing on these 10 considerations helps healthcare decision-makers to implement healthcare interoperability solutions that improve care coordination, unlock operational efficiency, and create experiences patients actually trust.
CERTIFY Health delivers secure, scalable EHR interoperability solutions designed around real clinical and administrative workflows, helping organizations transform fragmented systems into connected care ecosystems.
Book a Demo Now to See it in Action!
























