Table of Contents
The Impact of Digital Patient Engagement in Cataract Surgery Experiences
Digital patient engagement is solving real-world challenges for both patients and ophthalmology clinics. By integrating smart communication tools and remote workflow automation, practices can dramatically enhance efficiency, accuracy, and satisfaction.
A recent 2025 study found that remote data entry and digital scribing led to a measurable increase in Net Promoter Score (NPS), a key indicator of patient satisfaction.
Patients experienced 30.2% shorter wait times compared to in-person scribing, confirming that time savings remain one of the strongest drivers of patient loyalty and satisfaction.
What Is a Digital Scribe?
- A digital scribe is an advanced documentation tool that captures and records patient–provider conversations during clinical encounters.
- Using speech recognition and AI-powered transcription, it automatically converts spoken dialogue into structured medical notes within the electronic health record (EHR)
- This technology allows ophthalmologists and other clinicians to focus on patient interaction rather than manual notetaking.
- The result is greater accuracy, reduced documentation time, and improved clinical efficiency, while maintaining a complete and compliant record of every patient visit.
Real-world data also shows that, digital check-in and engagement tools save approximately 5 minutes per patient for single-site cataract surgery practices. These minutes quickly add up to major gains in operational throughput and reduced staff workload.
Globally, cataract prevalence is highest among adults over 40, affecting 11.8%–18.8% of this population. This group often faces barriers such as limited mobility, forgetfulness, or difficulty attending in-person visits. Practically, all of this can be overcome through a remote digital engagement platform.
Cataract surgery itself is a multi-step, high-precision procedure, with complexity rates ranging from 0.1% to 1% depending on patient volume and surgical type. These cases demand meticulous coordination.
Digital patient engagement via unified healthcare platforms makes possible by reducing human error, improving adherence, and supporting consistent communication.
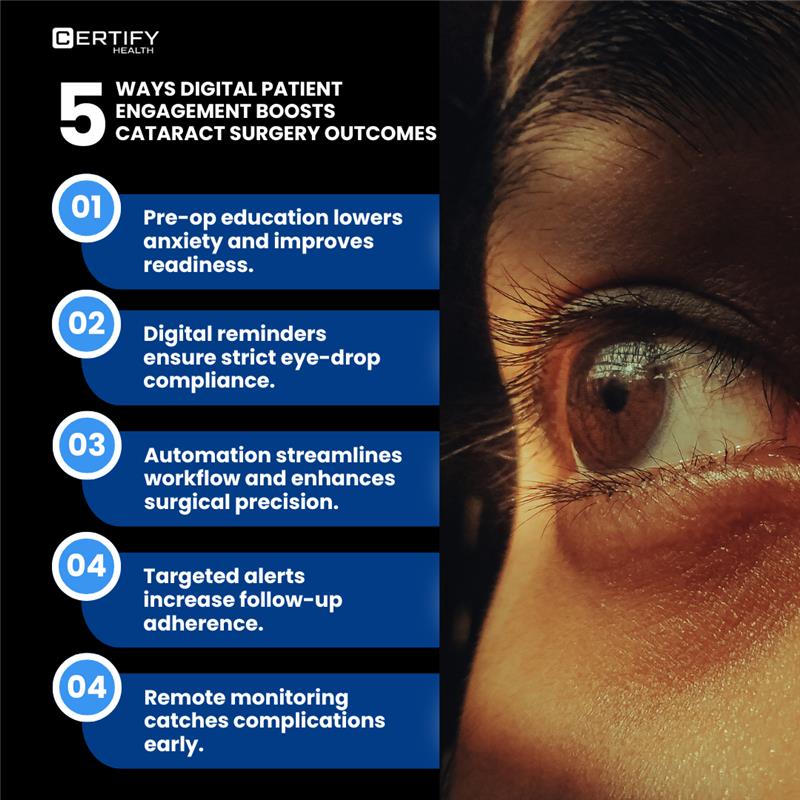
Read below to discover five proven ways digital engagement enhances cataract surgery outcomes, from preoperative readiness to long-term postoperative success.
How Digital Patient Engagement Enhances Every Stage of Cataract Surgery
1. Reduce Preoperative Anxiety Through Digital Patient Education Videos
Cataract surgery outcomes depend heavily on one factor that’s often overlooked: patient engagement.
Preoperative anxiety is common among eye surgery patients. Many feel uncertain or fearful before the procedure, and that emotional state can directly affect how well they respond during and after surgery.
Non-pharmacological interventions such as digital counseling, educational videos, and even calming music have been proven to reduce anxiety levels. Research shows that psychologically prepared patients experience less postoperative pain and greater surgical cooperation.
What Are Non-Pharmacological Interventions?
- Non-pharmacological interventions are therapeutic methods used to improve patient outcomes without relying on medication or drugs.
- These approaches focus on behavioral, psychological, or environmental techniques that support healing and well-being.
- Examples include exercise therapy, sound or music therapy, guided communication, meditation, and patient education.
- In surgical care, such interventions can significantly reduce anxiety, enhance patient cooperation, and improve overall recovery by addressing the emotional and psychological aspects of the treatment process.
Anxiety doesn’t just cause stress. It can also cause patients to delay or avoid surgery altogether.
Studies reveal that structured preoperative counseling increases the number of patients proceeding with cataract surgery by 14%, while 93% report that counseling directly influenced their decision to go forward.
Healthcare providers can elevate these outcomes by using unified digital patient engagement platforms. Such systems deliver counseling materials, instructions, and reassurance in a consistent, accessible, and structured format. This ensures that every cataract patient is fully informed, calm, and ready for a successful recovery.
2. Accelerate Recovery by Ensuring Proper Eye Drop Administration
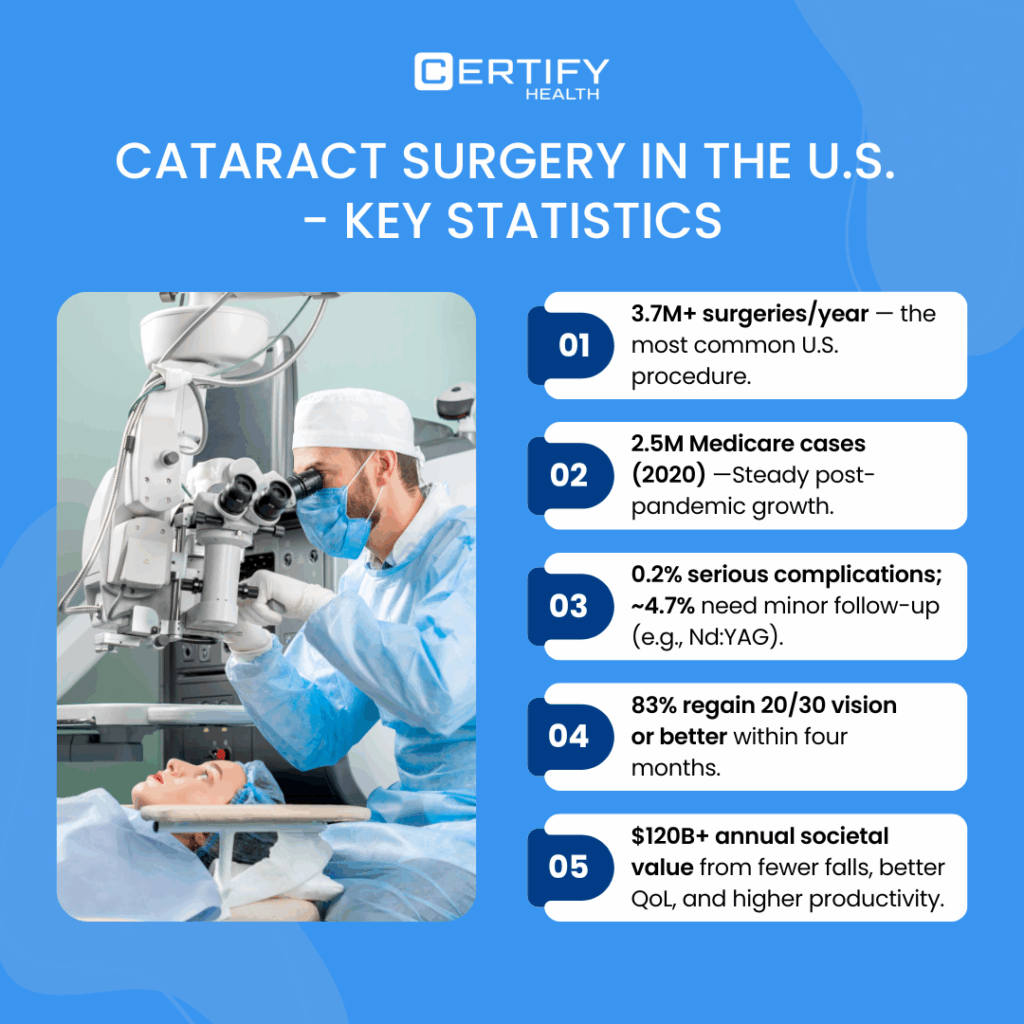
A recent analysis of 82,246 cataract surgery patients from the Medicare database revealed key postoperative trends. Within six months of surgery, Nd:YAG laser capsulotomy was required in 4.7% of patients, while intraocular lens (IOL) exchange and IOL repositioning each occurred in 0.2% of cases.
What Is Nd:YAG Laser Capsulotomy?
Nd:YAG (neodymium-doped yttrium aluminum garnet) laser capsulotomy is a non-invasive outpatient procedure used to treat Posterior Capsule Opacification (PCO) — a frequent complication of cataract surgery.
The laser creates a clear opening in the cloudy posterior capsule behind the implanted intraocular lens, restoring the light pathway to the retina and improving vision.
An Intraocular Lens (IOL) is a small, clear, artificial lens that is surgically implanted inside the eye to replace the eye’s natural lens.
Why Do These Secondary Procedures Happen?
The main reason is non-adherence to postoperative eye-drop medication.
Data from Zuckerberg San Francisco General Hospital revealed that 40% of cataract patients admitted to partial or complete noncompliance with prescribed postoperative drops. This non-adherence led to cystoid macular edema (CME) rates approximately double the national average.
The Hidden Problem: Technique, Not Just Compliance
Even when patients claim proper drop use, execution often falls short. In one study, although all participants understood the correct technique in theory, only 94.9% avoided tip contamination, and 93.2% achieved correct drop placement; this means 6–7% of patients still risk infection or poor healing due to incorrect administration.
Unified digital patient engagement platforms can close this critical gap. By offering postoperative education, video-based drop administration tutorials, and automated reminders, clinicians can ensure higher compliance and better surgical outcomes.
These digital touchpoints transform patient adherence from guesswork into measurable success. This also helps prevent complications and improves the long-term clarity that cataract surgery promises.
3. Streamline Workflows to Reduce Surgical Time and Improve Precision
Cataract prevalence continues to rise in the U.S. Between 2015 and 2024, ophthalmology clinics performed an estimated 3.8 million cataract surgeries, and by 2025, more than 30.1 million Americans are affected by cataracts.
Although an older dataset, the American Academy of Ophthalmology’s NEON study (1996–2001) still highlights a vital truth: 90% of cataract surgery patients report improved vision, with the highest satisfaction seen in younger patients and those without ocular comorbidities.
The Role of MIPS in Quality-Driven Care
The Merit-based Incentive Payment System (MIPS), administered by CMS under the MACRA Act of 2015, links Medicare payments to the quality of care delivered, not just volume.
For ophthalmology, one core MIPS quality measure evaluates patients aged 18 and above who show improved visual function within 90 days of post-surgery, based on patient-reported outcomes (PROs).
By analyzing MIPS data, providers can pinpoint what drives better visual outcomes, replicate best practices, and raise patient satisfaction across clinical teams.
When digital workflow systems integrate MIPS reporting and analytics, they create a closed-loop improvement cycle for ophthalmology practices.
Clinicians can:
- Track surgical efficiency metrics across all cases.
- Benchmark outcomes across peer networks.
- Identify workflow bottlenecks in real time.
- Comply with CMS quality measures seamlessly.
The result: shorter surgical times, improved precision, and measurable gains in patient outcomes across the 3.8 million annual cataract procedures performed nationwide.
| Field | Details |
|---|---|
| Measure ID | MIPS Quality Measure #303 |
| Measure Title | Cataracts: Improvement in Patient’s Visual Function within 90 Days Following Cataract Surgery |
| Measure Type | Outcome (Patient-Reported Outcome Measure - PROM) |
| Collection Type | MIPS Clinical Quality Measure (CQM), Electronic Clinical Quality Measure (eCQM), Registry |
| NQS Domain | Effective Clinical Care |
| Measure Steward | American Academy of Ophthalmology (AAO) |
| Description | Percentage of adults (18+) who received cataract surgery with an IOL and reported improved visual function within 90 days, based on a validated patient-reported outcome survey. |
| Denominator (Eligible Population) | Patients aged 18+ who underwent cataract surgery with IOL implantation during the performance period. |
| Denominator Exclusions | - Significant ocular comorbidities limiting visual potential (e.g., advanced macular degeneration, severe diabetic retinopathy). - Cognitive impairment or inability to complete the survey. - Death within 90 days of surgery. |
| Numerator (Performance Met) | Patients who reported improvement in visual function within 90 days of cataract surgery based on comparison of preoperative and postoperative survey scores. |
| Performance Not Met | Patients who did not show improvement in visual function or did not complete both surveys. |
| Reporting Requirement | Completion of both preoperative and postoperative visual function surveys (e.g., VF-8R, Catquest-9SF) within 90 days after surgery. |
| Rationale | Evaluates the patient-centered outcome of cataract surgery. It denotes improvement in real-world visual function rather than only clinical visual acuity. |
| Clinical Setting | Ambulatory surgery centers, ophthalmology practices, and outpatient hospital settings. |
| Measure Year | 2025 (Current CMS MIPS Measure List) |
4. Boost Follow-up Appointment Adherence with Targeted Digital Reminders
Postoperative follow-up is not just a clinical formality; it’s a key determinant of cataract surgery outcomes. Many vision-related complications can be avoided simply through consistent patient engagement after discharge.
Risk Stratification
Digital patient reminder systems can be integrated with MIPS quality measures to automatically identify patients at higher risk of poor postoperative outcomes.
These insights allow healthcare providers to send personalized follow-up reminders, educational messages, or appointment prompts, ensuring high-risk individuals remain compliant with their care plans.
Why Follow-Up Matters for Vision Recovery
Studies show that among patients who developed endophthalmitis after cataract surgery, only 44% had driving-level vision (20/40), and just 4% achieved 20/20 vision within three months.
These figures underscore the importance of timely reminders and structured follow-up to protect visual recovery.
Understanding Vision Clarity Levels
| Term | Category | Definition | Implication for Vision |
|---|---|---|---|
| 20/20 Vision | Normal Visual Acuity | Ability to see at 20 feet what a person with normal vision sees at 20 feet. | Clear distance vision, which is the clinical standard, though not necessarily a “perfect” vision. |
| 20/40 Vision | Below Normal Visual Acuity | You must be at 20 feet to see what a person with normal vision sees at 40 feet. | Blurred distance vision — often correctable with lenses but may limit tasks like driving. |
When unified digital patient engagement platforms automate these reminders, they not only improve adherence but also boost measurable vision recovery rates.
By connecting postoperative data with communication workflows, clinicians can close the loop between surgery and sustained sight, ensuring every patient achieves the best possible outcome.
5. Enable Remote Postoperative Monitoring for Early Complication Detection
Post-visit engagement programs play a crucial role in improving cataract surgery outcomes and ensuring timely follow-ups. These initiatives allow healthcare providers to actively monitor recovery, assess results, and identify potential complications early.
Through digital wellness programs, providers can verify patient progress, acquire accurate clinical data, maintain continuous communication, and evaluate therapeutic success.
They also help track changes in chronic eye conditions, all while enhancing transparency and patient trust.
However, it’s essential that every communication channel, digital message, and remote monitoring workflow remain fully HIPAA-compliant. Data protection and privacy are non-negotiable foundations of modern U.S. healthcare delivery.
Evidence from Clinical Practice
A Willis-Knighton Eye Institute study involving 477 eyes treated for refractive cataract surgery found that nearly 400 eyes achieved 20/20 or better binocular uncorrected distance visual acuity (BUDVA) just one month postoperatively.
Remarkably, 99% of patients stayed on track with their expected recovery, thanks to consistent digital follow-ups and remote monitoring.
| Component | Meaning |
|---|---|
| Binocular (B) | Vision measured using both eyes simultaneously |
| Uncorrected (U) | Measurement taken without corrective lenses. |
| Distance (D) | Clarity measured for far objects, typically at 20 feet (6 meters). |
| Visual Acuity (VA) | The scientific measure of vision sharpness or clarity. |
When digital post-visit engagement and remote monitoring are implemented securely, providers can maintain visibility into patient recovery and ensure surgical outcomes remain predictable. This strengthens both clinical performance and patient satisfaction.
Conclusion: Enhancing Cataract Care Accuracy Through Digital Workflow Integration
Cataract surgery practice management is inherently complex. Clinical precision depends not only on surgical skill but also on how effectively postoperative data is monitored and acted upon.
A recent study found that incorporating remote monitoring and digital follow-ups improves postoperative decision-making accuracy to 88.7%, a clear indicator that continuous engagement drives better patient outcomes.
By adopting CERTIFY Health’s integrated digital workflow, ophthalmology practices can seamlessly connect cataract care with existing EHR systems, eliminating silos and reducing administrative burden.
This integration streamlines every stage, from scheduling and documentation to outcome tracking, resulting in up to 50% reductions in surgical preparation time and manual data entry.
The result is a smarter, faster, and more connected cataract care ecosystem that empowers clinicians to focus on precision, efficiency, and patient satisfaction.
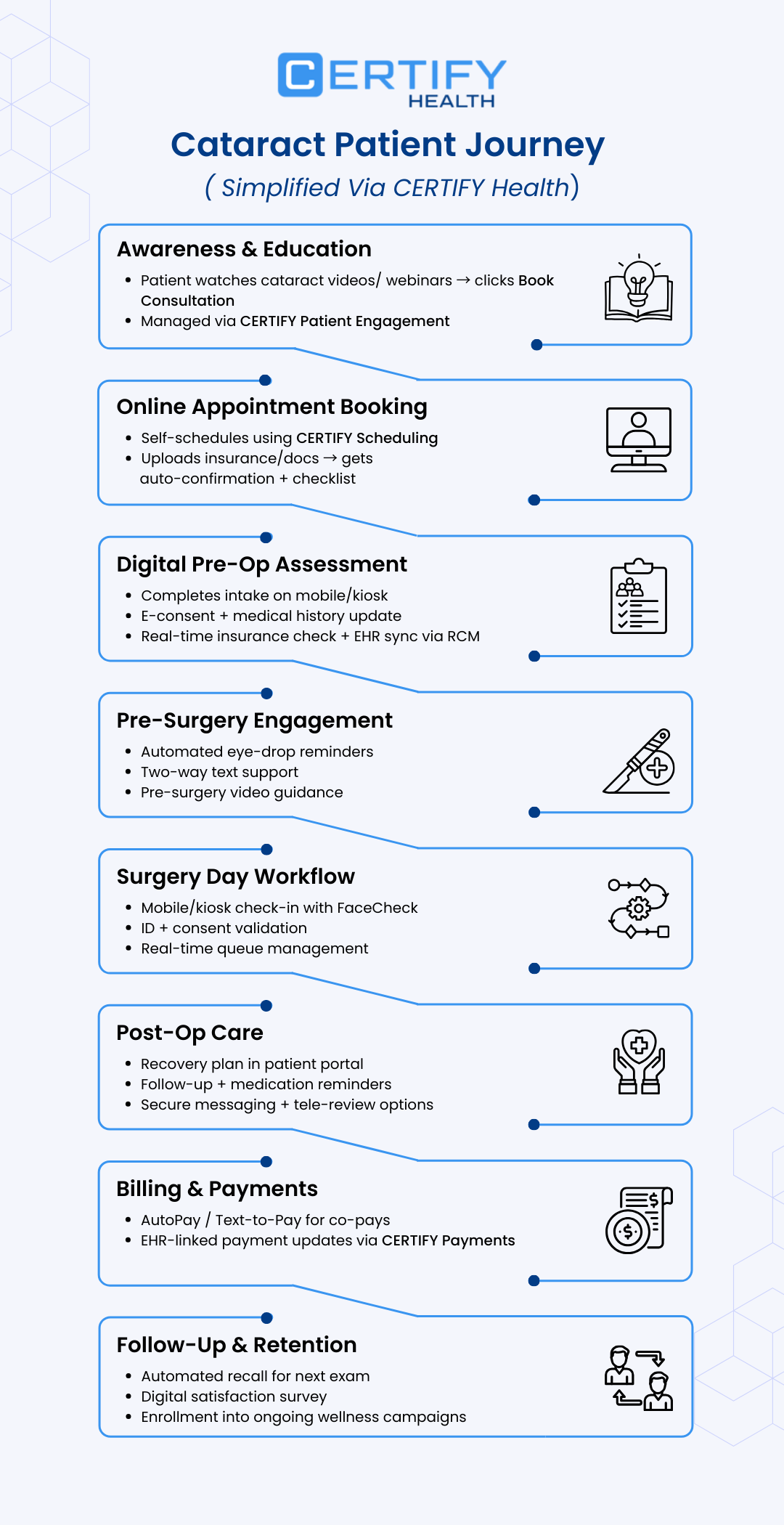
How CERTIFY Health Automates Cataract Surgery Workflows and Improves Practice Efficiency
CERTIFY Health delivers EHR-agnostic interoperability, allowing ophthalmology practices to securely access and synchronize patient records, OCT imaging, fundus photographs, and prior test results; all in one unified digital platform.
This seamless data flow improves both clinical precision and administrative efficiency, helping practices reduce operational friction across every step of the cataract care journey.
Practices using CERTIFY Health have also reported up to a 30% reduction in no-shows and a measurable improvement in schedule utilization.
How CERTIFY Health Solves Cataract Workflow Bottlenecks
| Cataract Workflow Bottlenecks | How CERTIFY Health Automates It | Outcomes |
|---|---|---|
| High No-Show Rates and Manual Scheduling | Automated reminders, digital self-scheduling, and integrated recall systems for follow-ups | No-shows reduced to 1.8%, optimized provider schedules, and improved revenue protection |
| Fragmented Check-In & Data Collection | Unified digital check-in, mobile intake, and auto-populated EHR-integrated records | Accelerates throughput, minimizes manual errors, saves staff time, and pre-fills surgical and insurance data |
| Manual Data Re-Entry & Siloed Systems | One connected platform linking check-in, scheduling, billing, and documentation | Eliminates duplicate entry (cuts clerical steps by 46.8%), ensuring smooth data continuity |
| Delayed Payments & Claim Denials | Automated insurance verification and real-time eligibility checks | Shortens reimbursement cycles, reduces denials, and strengthens cash flow |
| Postoperative Patient Engagement Gaps | Patient education modules, automated clinician follow-ups, and secure digital messaging | Improves medication adherence, tracks visual outcomes, and prevents missed complications |
| Inconsistent Preoperative Instructions & Consent | Digital consent forms and instructional videos delivered via secure patient portals | Standardizes patient education, reduces errors, and accelerates pre-op readiness |
| Staff Burnout from Administrative Load | Task automation and digital assignment queues with live dashboards | Frees staff to focus on high-value tasks, reduces burnout, and boosts retention |
| Patient Experience Fragmentation | Continuous digital experience from check-in to payment across all communication channels | Improves satisfaction, increases NPS, and reduces patient drop-offs |
| Disjointed Reporting & Compliance Risk | Centralized analytics and automated MIPS/quality reporting tools | Simplifies compliance, lowers audit risk, and supports value-based care delivery |
With CERTIFY Health, ophthalmology practices can achieve the precision, speed, and efficiency needed to meet modern quality standards while maintaining a connected and patient-centric experience.
Book a demo with CERTIFY Health today to explore how digital automation can transform your cataract surgery workflows.