Table of Contents
Integrated Healthcare: Connecting the Continuum of Care
Integrated healthcare isn’t just a buzzword; it’s the foundation of truly connected patient-centered medicine.
It means care is coordinated, continuous, and consistent across multiple healthcare workflows all focused on the patient’s experience and engagement.
This includes everything from primary and specialty care to behavioral health and social services.
According to the World Health Organization (WHO), integrated healthcare strengthens the care continuum at every level, from prevention and early intervention to palliative and long-term support.
It’s where clinicians, behavioral health experts, and social workers unite to deliver holistic, team-based care that addresses the full picture of a patient’s well-being.
The success of integrated healthcare depends on:
- High degree of service coordination
- Open, continuous communication among care teams
- Shared planning and data access
- Collaborative interventions that adapt to patient needs
And the results speak volumes. Peer-reviewed studies show that when integrated care workflows are applied (particularly for chronic conditions), there’s a 19% reduction in hospitalization risk. That’s the measurable impact of connected care in action.
In short: Integrated healthcare is a smarter, seamless system that delivers better outcomes, lower costs, and a patient journey that finally feels human again.
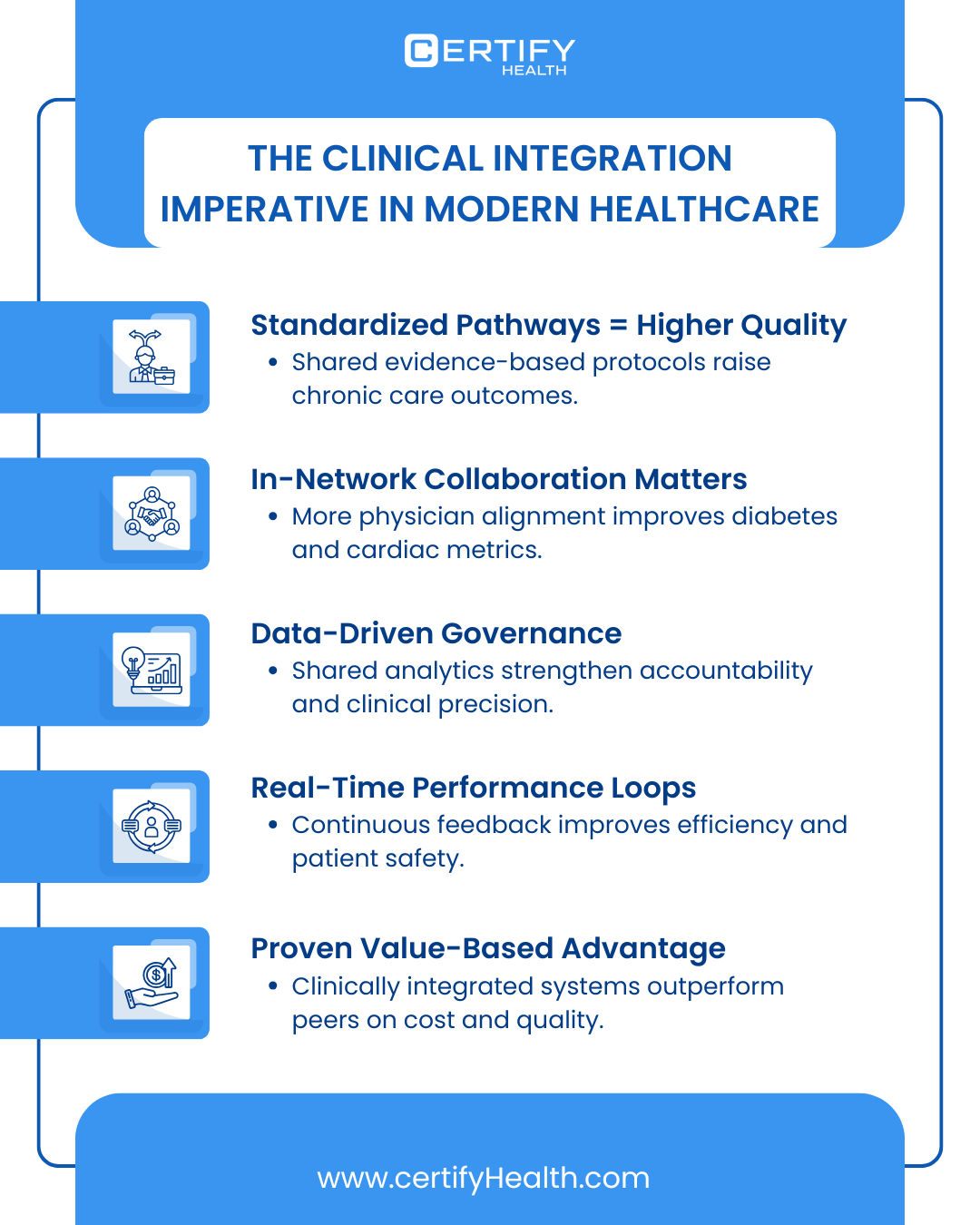
5 Ways Integrated Healthcare Improves Patient Outcomes
1. Integrated Behavioral and Primary Cares
When behavioral health meets primary care, outcomes improve and costs drop.
In a Michigan primary care clinic, implementing Integrated Behavioral Health (IBH) services reduced the average medical visit cost per patient from $326 to $254. That’s a savings of $71.90 per patient.
But the impact isn’t just financial. In a 12-month behavioral health study, nearly half of patients experienced a 50% reduction in depressive symptoms through multidisciplinary integrated care interventions.
Across seven clinics, integrated behavioral healthcare also led to an 18-percentage-point decrease in first-year hospitalization rates.
Primary care practices that adopt integrated models consistently report:
- Higher quality of care and better patient outcomes
- Fewer emergency room visits and hospital admissions
- Lower overall costs for chronic disease management
Integrated behavioral and primary care is an evidence-based evolution that delivers measurable results for both patients and providers.
2. Collaborative Multidisciplinary Care Teams
The proof is stacking up and it’s hard to ignore. In a systematic review, 52% of published studies reported better clinical outcomes for patients treated by collaborative, team-based care models compared to non-integrated approaches.
The advantages go beyond efficiency. Research shows that integrated healthcare models deliver greater effectiveness for ethnic minority populations, helping narrow long-standing health disparities that traditional, siloed care systems often widen.
In a review of heart failure patients, the introduction of multidisciplinary care rounds brought 30-day readmission rates down from 27.56% to 17.22%, while also reducing clinical risk.
One clear example comes from McKinsey’s paper, The Evidence for Integrated Care, which found significant improvements in diabetes-related clinical markers, particularly HbA1c levels.
In other words, patients in integrated care systems aren’t just better managed; they’re getting measurably healthier.
Another notable study found that 96 patient-days were saved annually when connected, multidisciplinary workflows were implemented for acute care surgery patients.
The message is clear: when healthcare professionals coordinate seamlessly, patients recover faster, hospital stays shorten, and system efficiency rises.
3. Chronic Disease Management Through Integrated Models
A review in the International Journal of Integrated Care found that integrated healthcare models led to an 15–35% improvement in chronic disease control rates, along with significant reductions in hospital admissions.
The benefits go beyond clinical metrics. Another study revealed that medication non-adherence dropped from 30% to just 12% following integrated care interventions for chronic patients. This is a direct result of better coordination, communication, and patient engagement.
Behavioral outcomes tell the same story. Integrated approaches have shown clear gains in Patient-Reported Outcomes (PROs), with patients reporting improved quality of life and emotional well-being.
These psychological benefits ripple outward, reducing caregiver burden and promoting long-term adherence to therapy.
Integrated care doesn’t just treat conditions; it sustains wellness, supports families, and builds healthier communities.
4. Patient-Centered Care Coordination
Integrated healthcare transforms the patient experience significantly. The World Health Organization (WHO) notes that when care is continuous and communication is seamless, the results are clear: higher patient satisfaction, better capacity utilization, and stronger health literacy.
This continuum of care means improved access, fewer readmissions, and a smoother journey from diagnosis to recovery.
But patients must be consistently included in:
- Shared decision-making
- Personalized education
- Healthcare platform interactions
- Mobile engagement tools
When patients are empowered to participate in their care, the outcomes shift dramatically.
Research shows increased patient preference and adherence, and that’s not just theory. Patients engaged through unified healthcare management platforms were 2.68× more likely to have meaningful health discussions and follow their treatment plans.
Integrated healthcare builds a system where engagement drives outcomes and satisfaction follows.
5. Data-Driven, Technology-Enabled Integrated Care
Integrated healthcare thrives on connections that start with data. Data-driven, tailored interventions are the backbone of modern care coordination, making every patient touchpoint smarter and more personalized.
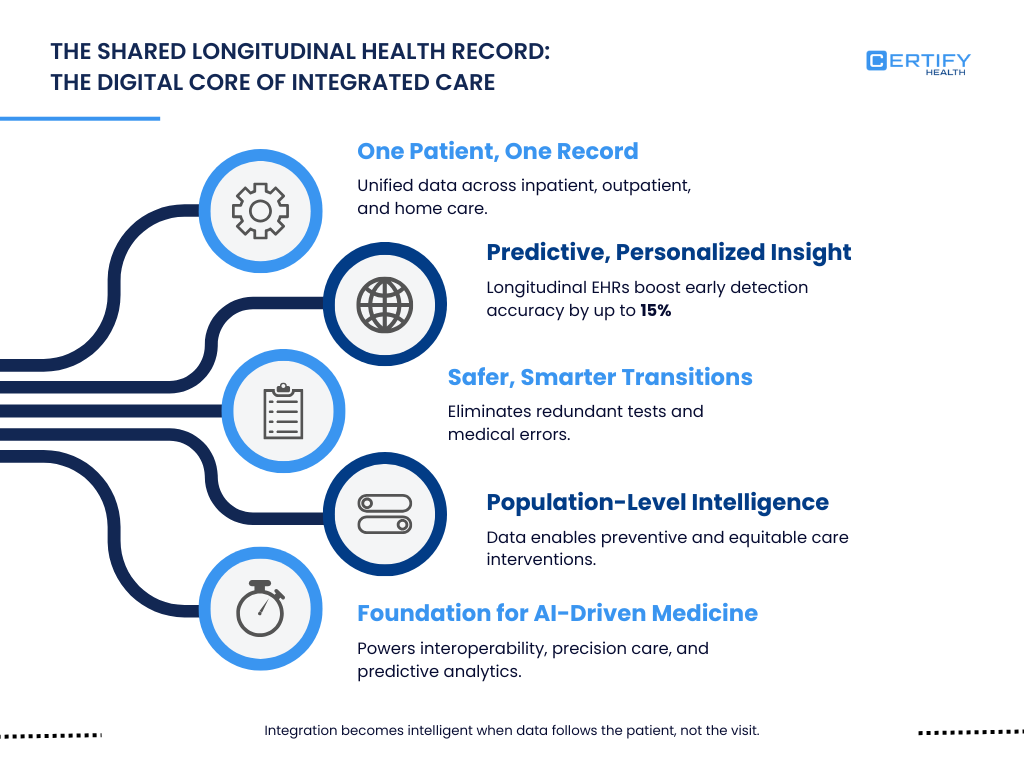
Continuity of care depends on real-time data flow across systems. That’s why the best integrated networks rely on:
- Interoperable EHRs that unify patient records
- Predictive analytics that flag high-risk patients early
- Patient portals that enhance access and engagement
A 2022 study in Frontiers in Public Health found that robust EHR interoperability improved care coordination speed by 30% and significantly cut redundant testing, strengthening both efficiency and clinical accuracy.
The takeaway? Personalized integrated care only works when predictive analytics and patient data move together.
A National Academies of Sciences report found that addressing social needs in clinical care can yield up to a 10% reduction in avoidable hospitalizations and increase in preventive screening uptake.
Add in privacy safeguards, real-time alerts, and accessible patient portals, and you create a connected ecosystem that enables proactive care and better outcomes before problems escalate.
From Insight to Action: Implementing Integrated Care with CERTIFY Health
So, what’s next? How do you turn the vision of integrated healthcare into measurable impact?
The answer lies in CERTIFY Health, a unified healthcare management platform built to connect every step of the patient–provider journey. It simplifies the complexity of care coordination while empowering organizations to implement integrated healthcare at scale
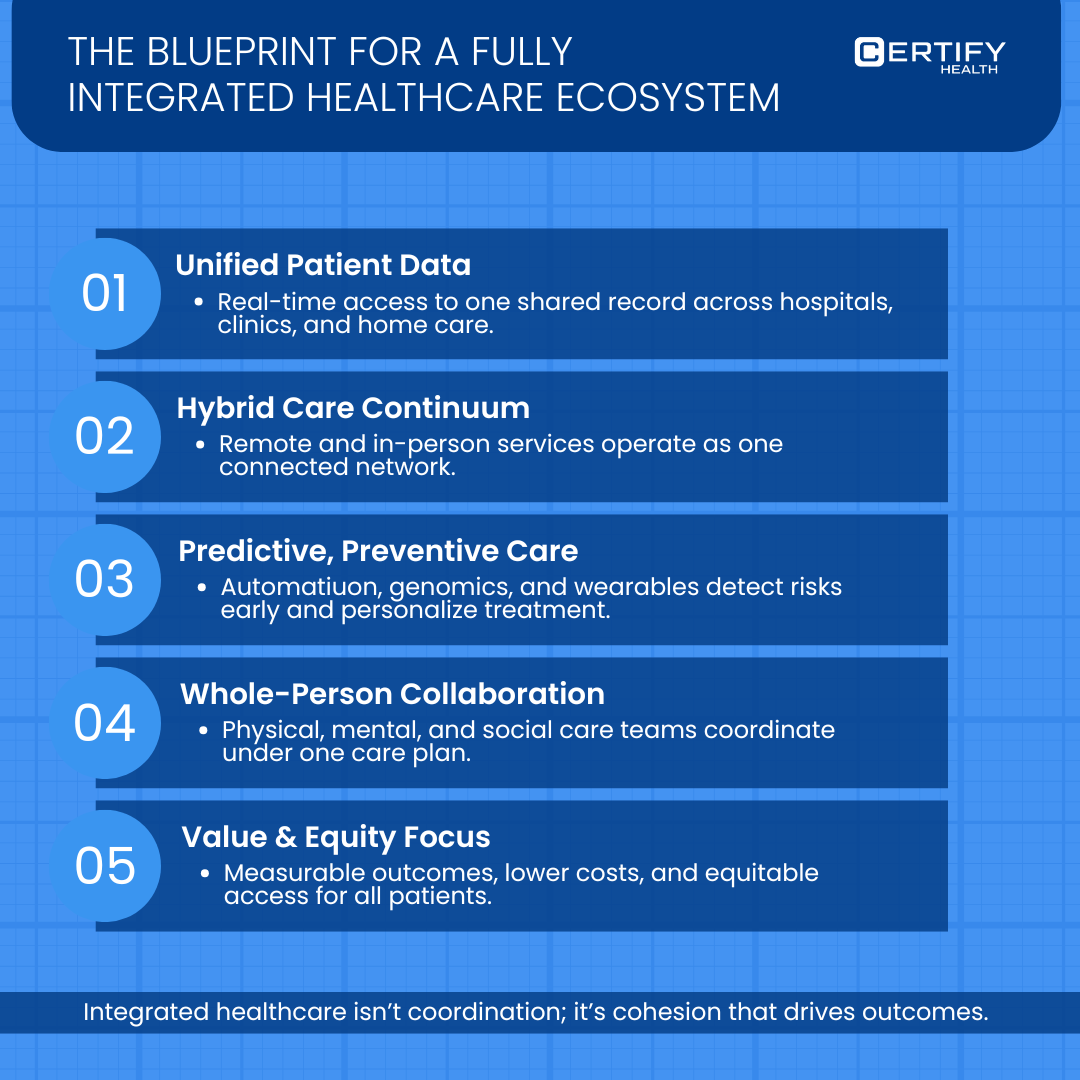
CERTIFY Health brings together clinical, administrative, and engagement workflows under one seamless system, enabling real-time communication, coordinated interventions, and data-driven insights that directly improve patient outcomes.
Below, you’ll find a table detailing how CERTIFY Health’s modules and platform features strengthen every dimension of integrated care. This simply helps your organization move from fragmented systems to a connected, outcomes-driven healthcare ecosystem.
| Module | Key Capabilities / Features | How it supports Integrated Healthcare |
|---|---|---|
| Patient Experience | • Digital intake via mobile/tablet/kiosk (pre-registration) • Self-scheduling (online, mobile) & waitlist/ASAP list functionality • Contactless check-in, facial authentication • SMS/email reminders, e-consent, digital forms |
By enabling patients to engage digitally across the front-door (pre-arrive/check-in) and by reducing manual intake, it connects the patient journey from scheduling through arrival. This minimizes the silos between access, intake, and clinical workflows. |
| Patient Management Software | • Unified patient chart & timeline (demographics, meds, vitals, visit history) • Structured documentation (SOAP/progress notes), AI-powered transcription & summarization • Order entry (labs/imaging) with HL7/FHIR and result attachments |
This module centralizes clinical and operational data into a longitudinal patient record. Thus, it easily bridges front-office (intake) and back-office (clinical/diagnostic) domains, facilitating continuity of care, fewer duplicate records, and richer data for downstream workflows. |
| Practice Management System (PMS) | • Scheduling/appointments engine (online booking, provider calendar sync, slot blocking) • Multi-location scheduling, user roles/permissions, analytics dashboards • Eligibility/intake/billing integration built-in |
PMS unifies the operational workflows of a practice: from booking through billing. By integrating scheduling with intake, eligibility checks, and reporting, it reduces administrative fragmentation and connects business operations with clinical flow. |
| Revenue Cycle Management (RCM) | • Patient payment solutions: Text2Pay, portal/kiosk/mobile payments, card-on-file, automated billing/ledgers • Real-time insurance verification & co-pay/deductible collection upfront • Analytics: A/R days, reimbursement rates, denials reduction |
By automating and integrating billing, collections, and revenue workflows into the same platform that handles intake, scheduling and patient management, the RCM module ensures financial data flows seamlessly across the patient's lifecycle. |
| Interoperability | • EHR-agnostic integrations across major vendors: Epic, athenahealth, Meditech, eClinicalWorks • HL7/FHIR connectivity for orders/results in patient-management module • Compliance & security: HIPAA, HITRUST r2, SOC 2, PCI DSS, GDPR |
Interoperability provides the technical backbone for integrated healthcare. This enables data exchange across systems, avoiding duplication, supporting enterprise-scale workflows, and ensuring the platform can plug into existing EHRs and data sources rather than remaining isolated. |
























