Table of Contents
Overview
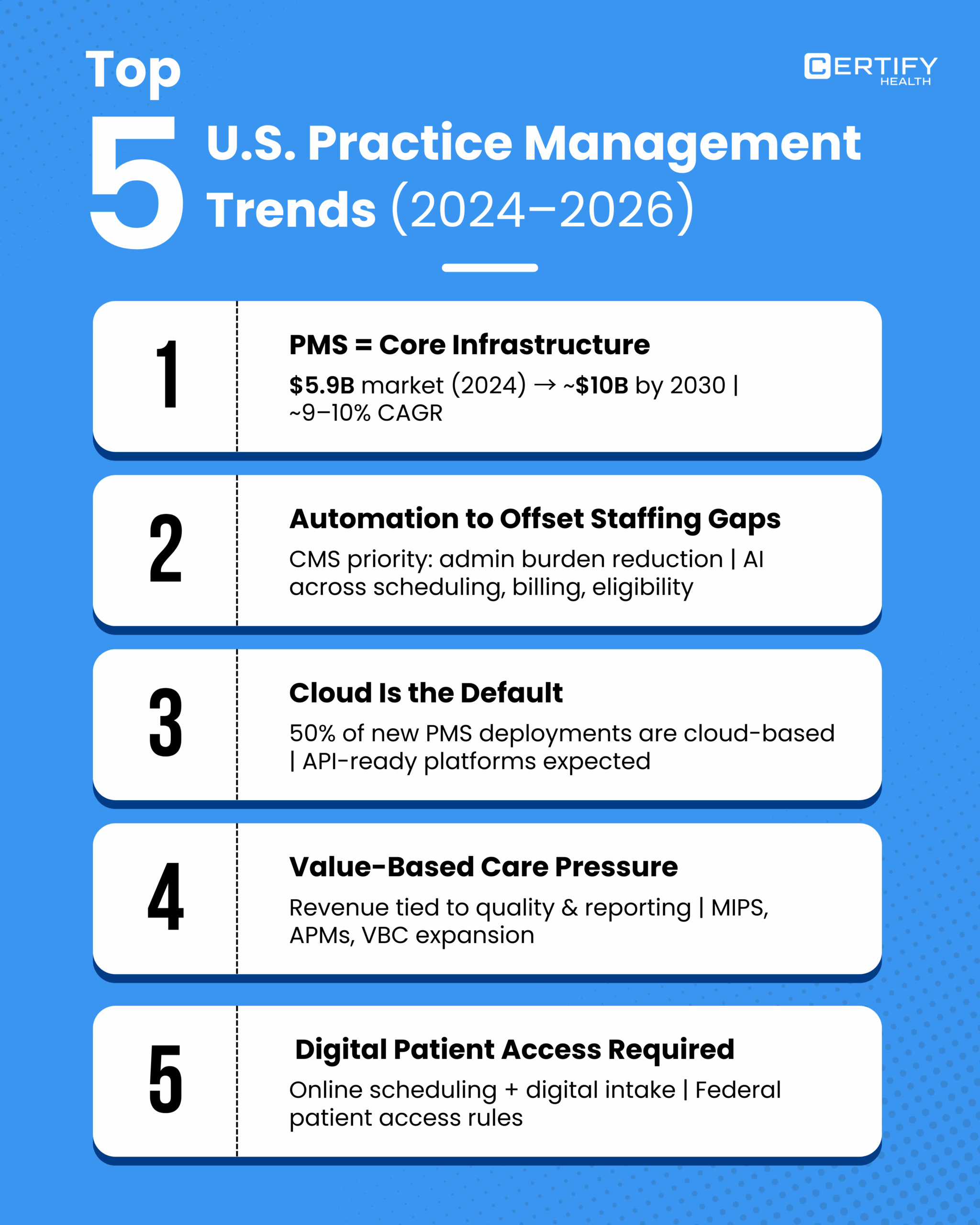
A modern practice management system (PMS) is now mission-critical operational infrastructure for healthcare practices of all sizes.
The work of coordinating patient access, data capture, financial eligibility verification, front desk workflows, and revenue capture is too complex for manual, disconnected processes that waste time and erode profitability.
Healthcare practices face record operational pressure. Patient no-show rates remain a persistent drag on access and revenue.
According to Medical Group Management Association data, many practices still contend with no-show rates that hover around 5% to 30% of scheduled appointments, leading to $150 billion in annual system-wide losses from unused capacity and cancellations.
Manual administrative work consumes staff energy that could otherwise support patient care. Studies show up to 25% to 30% of US healthcare costs originate from administrative work, much of which is repetitive and error-prone.
Staff shortages further compound these issues, increasing both errors and denial rates. In a national survey, 96% of revenue cycle leaders agreed insufficient staffing negatively affects revenue, and 92% said errors by inexperienced staff disrupt claims processing, ultimately slowing payments and lowering total collections. Automation adoption is rising because these pressures are structural, not temporary.
The realities of modern healthcare go beyond inconvenience. Manual workflows inflate costs, delay care, and undermine patient experience.
Analysts estimate that US providers spend about 25% of total healthcare expenditure on administrative tasks, far above peer nations, and that cutting inefficiencies could reduce cost by hundreds of billions annually.
Nearly 20% of claims are initially denied, and more than half are never refiled because of simple intake errors, not clinical disagreement.
Across specialties and settings, double entry, manual verification, and disjointed workflows create a hidden drag that costs practices revenue, staff retention, and patient satisfaction.
A modern practice management system must be more than a glorified scheduler. It must unify scheduling, intake, eligibility, front office operations, billing readiness, and operational reporting into a coherent workflow engine that drives outcomes rather than chores.
With intelligent scheduling, real-time eligibility, structured intake, automated tasking, and integrated reporting, practices convert operational control into financial performance.
CERTIFY Health delivers precisely this unified platform. By consolidating disparate workflow domains into a single, real-time operational hub, CERTIFY Health eliminates redundant tools and manual handoffs that slow practices down. Instead of reacting to administrative bottlenecks, teams work from a consistent data foundation with visibility into patient flow, revenue cycle status, and staff workload.
This article explains what an effective PMS does, why practices are automating, and how a modern practice operations framework supports sustainable growth, operational predictability, and better patient experiences.
Understanding Practice Management in Healthcare
What Is a Practice Management System?
A practice management system is the structured software layer that orchestrates non-clinical workflows within a healthcare practice. It ensures patients move through the practice in a planned, predictable way while maximizing operational and financial outcomes.
Core practice management functions include:
- Appointment scheduling and calendar logic
- Patient intake and structured demographic capture
- Insurance eligibility verification and coverage automation
- Front desk check-in, consent capture, and task coordination
- Billing readiness, superbill assembly, and claims preparation
- Operational reporting, throughput visibility, and productivity tracking
It is critical to distinguish these capabilities from clinical documentation handled by electronic health records (EHRs).
The EHR answers clinical questions: “What happened during care?”
The PMS answers operational questions: “Can we schedule the right care with the right revenue outcome in a predictable way?”
The distinction matters because practice revenue depends on both clinical quality and operational predictability. Ineffective intake and eligibility workflows directly correlate with higher denial rates and delayed payments. This is a major threat to practice viability.
Many healthcare claims are initially denied due to administrative errors, and more than half of these are never resubmitted, often because of incomplete or inaccurate intake data, costing practices millions annually.
In a revenue cycle context, every unverified insurance coverage and every missing demographic field creates operational drag that ripples from check-in to receivables.
Common Operational Challenges in Healthcare Practices
Healthcare practices across specialties consistently report the same operational pain points:
Scheduling inefficiency and no-shows
Practices lose significant capacity to missed appointments. National data shows that no-show rates vary widely but can reach as high as 30% in some settings, and even conservative measures place no-show rates around 5% in certain specialties.
At an average revenue loss of approximately $200 per missed appointment, the cumulative financial impact across a practice becomes material very quickly.
Manual intake and administrative backlog
Repetitive manual entry is costly and error-prone. Estimates indicate that about 57% of healthcare worker time is spent on data entry or monitoring with manual interfaces, leading to cascading errors and increased administrative costs.
Staff burnout directly correlates with manual intensity, with nearly 46% of front office personnel reporting exhaustion related to repetitive work.
Eligibility verification delays and denial exposure
Paper-driven verifications are slow and inconsistent. Prior authorizations, though less common than other transactions, remain among the most manual, with only about an half currently automated, creating delays that translate to millions in lost productivity. With staffing shortages, practices report rising denial rates partly due to human error in eligibility checks.
Front office fragmentation
When workflows are inconsistent across roles and locations, traditional task assignment relies on tribal knowledge and manual spreadsheets rather than structured systems.
This leads to variability in service quality, longer wait times, and inconsistent revenue capture.
Staff workload imbalance
Without visibility into task distribution, practices risk overload in some roles while underutilizing others. This produces burnout, turnover risk, and inefficiency that costs practices both productivity and recruitment dollars.
Multi-location complexity
Clinics with multiple sites often operate with divergent tools and local practices, making management reporting and standardization difficult. A PMS that centralizes oversight improves consistency and reveals otherwise hidden operational gaps.
These operational problems are not isolated. They reinforce one another, increasing cycle time, staff fatigue, and financial leakage. Poor scheduling increases no-shows. Manual intake increases errors. Eligibility delays increase denials. All of these weaken patient experience, which in turn feeds back into access and retention metrics.
Why Practices Are Moving Toward Automation
1. Patient expectations have changed.
Research shows 93% of patients prefer digital communication options such as online scheduling and reminders, yet many practices still rely heavily on phone-based interaction. Failure to match these expectations translates into lower retention and competitive disadvantage.
2. Administrative burden is unsustainable.
Studies show that providers spend substantial portions of their week on paperwork, including about 1.84 hours per day outside clinic hours, contributing to 63% clinician burnout, with documentation cited as a leading driver.
3. Staff shortages are structural.
Workforce gaps reduce throughput and increase errors. Surveys show staffing shortages increase denial rates and slow reimbursement cycles, with nearly 70% of healthcare executives citing staff shortages as a driver of denials.
4. Automation delivers measurable gains.
Studies of automated workflows in behavioral health showed practices achieving 15 hours of weekly labor savings per provider, no-show rate reductions of 65–80%, and 2–4 month payback on automation investments. These gains translate to increased capacity, lower costs, and better patient access.
The Modern Practice Operations Framework
A practice management system (PMS) must support the full lifecycle of the patient visit. When workflows are unconnected or manual, operational friction arises at every touchpoint.
The following sections deconstruct each operational stage, referencing measurable outcomes where available to guide buyers evaluating PMS solutions.
Pre-Visit Operations
Scheduling, Intake, and Eligibility: Reducing Operational Drag Upfront
Pre-visit operations determine whether the patient journey starts smoothly or with friction that consumes resources, reduces capacity, and threatens revenue capture.
Scheduling Starts with Predictable Booking
Appointment scheduling is not just calendar entry. It is capacity planning, patient communication, and waitlist optimization. In primary care centers, baseline no-show rates have been measured at about 21%, contributing to 3-14% revenue loss and longer waits without advanced scheduling strategies in place.
Advanced scheduling capabilities in a unified PMS reduce this friction by combining:
- Rules-based appointment templates that enforce correct visit durations and avoid underused time blocks
- Automated waitlist logic and ASAP lists to fill gaps created by cancellations
- Multi-location provider availability sync to optimize utilization across sites
- Recurring appointment support for chronic care and treatment plans
Real-world evidence shows that when automated powered dashboards predict and manage no-shows, practices achieve almost a 50% reduction in no-show rates and cut average wait times by nearly 6 minutes. This translates into more efficient time utilization for staff and clinicians.
Digital Intake Reduces Administrative Waste
Digital intake is more than typing data into fields. It is structured capture that eliminates repetition and errors.
Research on digital patient intake systems shows that when patients confirm information electronically before arrival, clinician schedules open up, average intake becomes 30% faster, and administrative task loads decrease substantially, affording staff time for higher-value work.
PMS systems that embed intake digitally also:
- Validate data as it is entered, catching inconsistencies early
- Provide condition-specific questionnaires that prepare staff for tailored care
- Support multiple touchpoints (mobile, SMS, portal, kiosk)
Eligibility Verification Prevents Revenue Leaks
Eligibility verification identifies coverage gaps before care is delivered. Automated real-time verification within intake workflows prevents costly downstream denials. Manual verification processes are identical to blind billing; they surface errors too late, resulting in denials that consume staff time and harm revenue.
Studies consistently identify administrative denial rates as a significant problem when eligibility checks lag or are incomplete. Digital systems that verify eligibility upfront significantly reduce the likelihood of rejection for non-clinical reasons.
Point-of-Visit Operations
Check-In, Consent, Payments: Efficiency at the Door
The point of visit is where data meets action. If front desk workflows are fragmented, every downstream process slows.
Automated Check-In Aligned with Front Office Flow
Check-in automation reduces paperwork and ensures data accuracy at the door:
- Validates patient demographics against intake records
- Confirms coverage and copay requirements
- Captures digital signatures and consent forms
- Flags missing authorizations prior to rooming
Automated check-in workflows place the emphasis on exception handling rather than repetitive data entry.
Integrated Payment Workflows Bridge Ops and Revenue
Collecting payments at check-in accelerates revenue capture. The traditional model delays these conversations, leading to eventual collection calls that are both inefficient and experience-negative. Modern PMS capabilities include:
- Copay and deductible collection
- Card-on-file and secure tokenization
- Text-to-Pay and AutoPay options
Reducing friction here also improves both revenue cycle performance and patient satisfaction, which further supports access and retention.
Post-Visit Operations
Claims, Tracking, Follow-Up: Translating Care to Cash
This is where operational workflows meet financial workflows. Poor integration between encounter data and claims workflows creates rework and denials.
Clean Handoff to Billing
A high-performing PMS ensures that clinical encounter data flows directly into billing readiness without double entry. This matters because:
- Missing or inaccurate data is the top cause of claims denials outside of clinical coding issues
- Manual reaudit of claims takes 20-40 minutes per claim and is a major workload driver
By linking scheduling, intake, eligibility, encounter data, and claims tracking, effective PMS solutions reduce administrative cycles.
Data-Driven Follow-Up Workflows
Once a claim leaves the system, tracking becomes critical. Modern PMS solutions provide:
- Claim status identifiers
- Denial reason categorization
- Prioritized follow-up task queues
- Automated patient notification triggers for outstanding balances
This structured approach to post-visit operations eliminates guesswork. Teams no longer rely on spreadsheets and scattered tools; they work from consistent operational and billing intelligence.
Administrative Oversight
Reporting, Tasking, Productivity: The Nervous System of Practice Operations
Administrative oversight is the differentiator between reactive and proactive practices. Without real-time visibility, leadership is flying blind.
Real-Time Operational Dashboards
Operational dashboards bring clarity on:
- Scheduling utilization and capacity
- No-show and cancellation patterns
- Staff productivity and task balance
- Visit volumes across locations
Research into digital transformation across large systems confirms that digitized administrative operations are strongly associated with improved healthcare access and efficiency.
While this study focuses on broader public health outcomes, the foundational principle applies at the practice level: real-time data supports better operational decisions.
Tasking Systems Distribute Work Efficiently
Automated task assignment reduces ambiguity. PMS systems with priority queues and escalation rules ensure that critical items — such as eligibility issues or outstanding consents — get resolved early, not at the end of the day.
Proper workload balancing correlates with reduced burnout and measurable improvements in throughput, as administrative inefficiencies cost practices time and money. Reducing manual task management removes a key operational bottleneck.
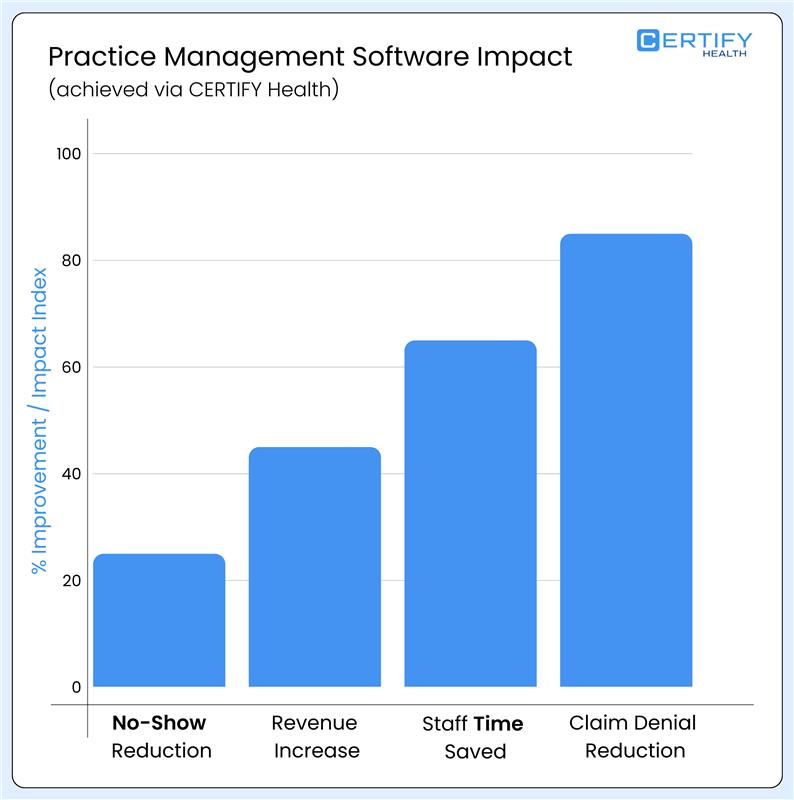
Why This Matters: Practice-Level Impact
When you evaluate the operations continuum equipped with these standards, the benefits cascade:
- Reduced no-show rates through predictive scheduling and reminders
- Faster patient throughput with automated check-in and intake
- Lower denial rates by verifying eligibility upfront
- Higher clean claims percentages with data continuity
- Improved staff productivity through real-time task management
- Executive-level operational visibility through role-based dashboards
These outcomes are not theoretical. Evidence shows that real-time scheduling can cut no-show rates by more than 50% while reducing wait times and improving satisfaction.
The modern practice operations framework is not a checklist of features. It is a workflow architecture that eliminates operational friction, distributes intelligence to every role, and strengthens the continuity between clinical and financial processes.
A practice management system evaluated in this context becomes an operational engine, not an administrative accessory.
How CERTIFY Health’s Practice Management System Works End to End
Modern healthcare practices do not struggle because of clinical quality. They struggle because operational workflows break under volume, complexity, and staffing constraints.
Research consistently shows that administrative inefficiency consumes 20–30% of total healthcare spending in the United States, largely driven by fragmented scheduling, intake, eligibility, and billing processes.
CERTIFY Health’s Practice Management System is designed as a single operational spine that connects every non-clinical workflow into one continuous system. Instead of managing handoffs, staff manage exceptions. Instead of chasing information, leadership operates from real-time visibility.
This section explains how the system functions across the full visit lifecycle and why each layer matters operationally and financially.
Intelligent Access Management That Protects Provider Capacity
Scheduling is the earliest and most powerful leverage point in practice operations. Errors here ripple across intake, staffing, utilization, and revenue.
Peer-reviewed research shows that outpatient no-show rates average 18–23%, with higher rates in practices using static scheduling rules and manual follow-up. Each missed appointment represents lost revenue, wasted staff time, and delayed care.
CERTIFY Health addresses this with an intelligent scheduling engine built on operational logic, not static calendars.
Core scheduling capabilities include:
- Rules-based appointment types and duration controls
- Slot logic based on provider, specialty, visit type, and location
- Real-time provider availability synchronization
- Multi-location scheduling with centralized oversight
- Support for recurring and long-term treatment plans
Advanced automation features include:
- Automated waitlists and ASAP lists that backfill cancellations
- Overbooking rules informed by historical no-show behavior
- Load balancing across providers and sites to reduce bottlenecks
Operational outcome: Higher fill rates, fewer idle slots, improved patient access, and predictable provider utilization.
Digital Intake That Fixes Data Quality Before It Breaks Revenue
Intake is the primary source of downstream errors. Manual forms, repeated questions, and transcription mistakes lead to eligibility failures, billing delays, and patient frustration.
Studies on digital patient intake show that structured, pre-visit data capture reduces administrative task time by 25–40 % and significantly improves demographic and insurance data accuracy.
CERTIFY Health replaces paper-based intake with mobile-first, structured workflows that complete data collection before the patient arrives.
Key capabilities include:
- Demographics and insurance capture with validation logic
- Secure ID and document upload
- Digital consent and acknowledgment forms
- Condition-specific questionnaires tailored to visit type
- Returning patient recognition with auto-fill.
Patients complete intake on their own devices, at their own pace. Staff shift from data entry to verification.
This upstream data cleanliness matters. Research consistently links incomplete or inaccurate registration data to increased claim denials and longer accounts receivable cycles.
Operational outcome: Zero paperwork, faster check-ins, cleaner data, and fewer downstream billing errors.
Revenue Protection Built into the Front Door
Eligibility errors are one of the most preventable causes of claim denials. Yet many practices still verify coverage late or rely on batch processes.
Several claims are denied on first submission, with eligibility and coverage issues among the leading non-clinical causes.
CERTIFY Health embeds real-time eligibility verification directly into registration and intake of workflows.
Eligibility capabilities include:
- Instant eligibility checks for commercial and government payers
- Automatic population of coverage notes into the patient record
- Batch re-verification for future appointments
- Automated alerts for coverage changes or inconsistencies
By identifying coverage issues before the visit, staff can resolve them proactively or inform patients of financial responsibility upfront. This aligns operational workflows with revenue protection.
Front-loaded eligibility verification significantly improves first-pass claim acceptance and reduces rework time for billing teams.
Operational outcome: Lower denial rates, faster payments, and fewer surprise billing issues.
Coordinated Daily Workflows Without Tribal Knowledge
Front and back office inefficiencies often stem from unclear ownership, manual task tracking, and fragmented communication.
Administrative staff spend a disproportionate amount of time coordinating work rather than completing it, contributing to burnout and turnover.
CERTIFY Health centralizes operations with structured tasking and workflow automation.
Operational features include:
- Task assignment with priority and escalation rules
- Role-based permissions and access controls
- Contextual staff messaging tied to workflows
- Operational checklists to standardize daily processes
- Unified audit trails across all actions
Every task is visible. Every handoff is documented. Managers can see bottlenecks in real time instead of discovering them after delays occur.
This level of operational clarity is strongly associated with improved throughput and reduced error rates in administrative workflows, as documented in healthcare operations research.
Operational outcome: Coordinated teams, predictable execution, and reduced operational risk.
Turning Visits Into Cash Without Rework
Billing inefficiencies are rarely caused by billing teams alone. They originate upstream when scheduling, intake, and eligibility workflows are disconnected.
Closed group studies show that billing and insurance-related activities for outpatient (primary care) visits required approximately 13 minutes of administrative time per visit, with total cost of about $20.49 per visit for billing and insurance functions.
CERTIFY Health aligns billing workflows directly with operational data.
Billing and RCM capabilities include:
- Copay and deductible collection at check-in
- Payment plans and card-on-file support
- Text-to-Pay and AutoPay options
- Integrated merchant services
- Charge capture and superbill workflows
- Claims tracking dashboards with denial visibility
By collecting accurate data early and enabling point-of-service payments, practices reduce follow-up costs and improve cash flow.
Point-of-service collection improves overall collection rates and reduces bad debt, particularly when combined with transparent financial communication.
Operational outcome: Faster cash flow, fewer billing bottlenecks, and reduced staff workload.
Most practices operate reactively because reporting lags reality. Decisions are made weeks after issues occur.
Organizations with real-time operational dashboards identify inefficiencies earlier and achieve measurable improvements in access, utilization, and staff productivity.
CERTIFY Health provides role-based, real-time reporting across the practice.
Reporting capabilities include:
- No-show and cancellation analysis
- Provider productivity summaries
- Claim status and denial reports
- Financial performance dashboards
- Aging accounts receivable indicators
- Multi-location performance comparisons
These insights enable leaders to intervene early, optimize staffing, and continuously improve workflows.
Operational outcome: Data-driven decisions, stronger margins, and predictable performance.
Why This End-to-End Design Matters
When scheduling, intake, eligibility, operations, billing, and reporting exist in one system, practices eliminate the handoffs that create cost and risk.
Evidence from multiple healthcare operations studies shows that integrated administrative systems outperform fragmented toolsets across efficiency, accuracy, and staff satisfaction metrics.
CERTIFY Health’s Practice Management System is built around this principle:
Operational continuity is the foundation of scalable, financially resilient healthcare practices.
Comparative Insights and Market Education
Healthcare practices evaluating a practice management system often compare features instead of architecture. That mistake leads to underperformance. This section reframes evaluation around system design, integration depth, and operational impact.
Traditional Practice Management Systems vs Modern Cloud PMS
Why Architecture Matters More Than Feature Count
Traditional practice management systems were built for a different era. On-premise deployments, batch data processing, and rigid workflows were acceptable when visit volumes were lower and reimbursement rules were simpler. Today, those same design choices create friction.
Legacy administrative systems contribute directly to delays, inefficiencies, and higher operational cost due to lack of real-time data flow and limited automation capability.
Key structural differences
| Dimension | Traditional PMS | Modern Cloud PMS |
|---|---|---|
| Data updates | Batch based | Real time |
| Accessibility | Location bound | Web and mobile |
| Scalability | Hardware limited | Elastic |
| Automation | Rule-light | Rules driven |
| Reporting | Retrospective | Live dashboards |
Real-time, cloud-based administrative platforms significantly improves scheduling efficiency and reduced operational delays compared to legacy systems.
From a buyer perspective, this distinction explains why feature parity does not equal performance parity. Cloud PMS platforms enable continuous optimization because workflows can adapt as volume, staffing, and payer rules change.
In short: Traditional PMS platforms record activity. Modern cloud PMS platforms orchestrate operations.
Standalone Tools vs Integrated Practice Platforms
Why Tool Sprawl Increases Cost and Risk
Many practices adopt best-of-breed tools for scheduling, intake, eligibility, and billing, assuming integration will solve fragmentation. Research shows the opposite often occurs.
Fragmented administrative toolsets increase reconciliation work, duplicate data entry, and error rates, especially at transition points between systems.
Problems caused by standalone tools
- Duplicate patient records across systems
- Inconsistent demographic and insurance data
- Manual reconciliation between scheduling and billing
- Limited end-to-end visibility
As mentioned earlier, staff spend up to 30% of their time reconciling data across disconnected systems rather than completing patient-facing work.
Integrated platforms eliminate these handoffs by design. Scheduling data flows directly into intake. Intake feeds eligibility. Eligibility informs billing. Reporting spans the full lifecycle.
Why Scheduling, Intake, and Billing Must Exist on One System
The Hidden Cost of Broken Lifecycle Continuity
Scheduling, intake, and billing are often treated as separate functions. In reality, they are sequential dependencies.
Errors introduced during scheduling and registration are leading contributors to downstream billing denials and delayed payments.
Lifecycle dependency examples
- Incorrect appointment type → wrong intake workflow
- Incomplete intake → failed eligibility verification
- Eligibility failure → claim denial or delayed payment
Practices with unified front-to-back administrative systems achieved significantly higher first-pass claim acceptance rates than those using separate tools.
By housing scheduling, intake, eligibility, and billing readiness within one PMS, practices ensure data continuity. Each step validates and strengthens the next.
Revenue integrity starts at scheduling, not billing.
Automation’s Growing Role in Practice Operations
Why Manual Operations No Longer Scale
Automation adoption in healthcare operations is not driven by technology trends. It is driven by necessity.
Persistent staffing shortages across administrative roles, increasing workload per employee and accelerating burnout.
At the same time, patient expectations mirror consumer digital experiences. Delays, paper forms, and unclear billing reduce satisfaction and retention.
Automation enables practices to:
- Maintain throughput with fewer staff
- Reduce cognitive load on front office teams
- Enforce workflow consistency across locations
- Surface issues before they escalate
A controlled study on AI-supported scheduling and workflow automation demonstrated substantial reductions in no-show rates and improved access without increasing administrative labor.
Automation does not replace staff. It replaces waste.
Market Education Summary
How Buyers Should Evaluate a Practice Management System
Based on current research and operational outcomes, buyers should evaluate PMS platforms using the following criteria:
1. Architecture
Cloud-native, real-time systems outperform legacy designs.
2. Integration Depth
End-to-end lifecycle integration matters more than tool count.
3. Automation Coverage
Automation must span scheduling, intake, eligibility, operations, and billing readiness.
4. Operational Visibility
Real-time dashboards enable proactive management.
5. Scalability and Governance
Systems must support growth without workflow fragmentation.
Peer-reviewed evidence increasingly supports the conclusion that integrated, automated practice management platforms deliver measurable improvements in efficiency, access, staff productivity, and financial performance compared to fragmented or legacy systems.
Use Cases Across Practice Types
Practice management challenges are not uniform. They scale differently based on practice size, organizational complexity, and specialty workflows. What remains consistent across all settings is that fragmented operations amplify inefficiency, while unified systems reduce cost, risk, and staff strain.
A modern practice management system must therefore adapt to different operational realities without forcing practices into rigid, one-size workflows. CERTIFY Health is designed to scale across this spectrum by standardizing what should be standardized and flexing where variability is unavoidable.
Small Clinics and Solo Practices
Small clinics and solo practices operate with minimal staffing and limited financial buffer. Even minor inefficiencies surface quickly as delayed schedules, overwhelmed staff, or missed revenue.
Smaller practices are disproportionately affected by administrative burden because fixed operational tasks consume a larger share of staff time compared to larger organizations.
Common operational challenges include:
- Manual scheduling and phone-based appointment management
- Paper-based or semi-digital intake processes
- Staff multitasking across front office, billing, and clinical support roles
- Limited access to real-time operational or financial reporting
CERTIFY Health simplifies daily operations by consolidating core workflows into a single system.
Operational impact areas:
- Unified scheduling, intake, eligibility, and billing workflows reduce tool switching
- Automation removes repetitive data entry and follow-up tasks
- Digital check-in and payments accelerate patient flow without adding staff
For small practices, this consolidation functions as an operational multiplier. Research indicates that digital front-office automation can reduce administrative task time per visit by more than 25%, allowing small teams to handle higher visit volumes without burnout.
The result is not growth through scale, but sustainability through efficiency.
Multi-Location and Group Practices
Group practices and multi-location organizations face a different challenge. As sites grow, variability creeps in. Each location develops its own scheduling habits, intake processes, and billing workflows, making performance difficult to compare and manage.
Inconsistent administrative workflows across locations directly contribute to reporting blind spots, uneven productivity, and delayed decision-making.
Common issues include:
- Fragmented scheduling across locations and providers
- Intake and billing processes that differ by site
- Limited visibility into cross-location utilization and performance
- Manual coordination between centralized leadership and local teams
CERTIFY Health enables centralized control while preserving local execution speed.
Operational benefits include:
- Unified scheduling logic across providers and locations
- Centralized reporting with site-level and provider-level drill-down
- Cross-site staff coordination through shared tasking and role-based permissions
Leadership gains system-wide visibility into access, throughput, and revenue performance. At the same time, individual locations operate without added friction or centralized bottlenecks.
Research consistently shows that standardizing administrative workflows across sites improves utilization and reduces operational variance, especially when supported by real-time data.
Large Health Systems and MSOs
Large health systems and management service organizations require more than efficiency. They require governance, compliance, and repeatability at scale.
As organizations grow, lack of standardized administrative workflows increases compliance risk and operational cost unless systems enforce consistency.
Core challenges include:
- High visit volumes across multiple service lines
- Complex organizational hierarchies and role definitions
- Regulatory oversight and audit readiness requirements
- Difficulty enforcing consistent workflows across sites
CERTIFY Health supports enterprise scale through system-level governance.
Key capabilities include:
- Scalable architecture that supports growth without performance degradation
- Standardized workflows enforced across sites and service lines
- Role-based access controls aligned to organizational structure
- Full audit trails that support regulatory and internal audits
In this environment, the practice management system becomes a control layer, not just an operational tool. Research shows that organizations with unified, auditable administrative systems respond more effectively to regulatory changes and payer requirements.
Practices With High Operational Complexity
Certain specialties introduce complexity that standard workflows cannot ignore. Orthopedics, dermatology, and other procedure-heavy or documentation-intensive specialties require flexibility without sacrificing structure.
Specialty practices experience higher administrative load due to variable visit types, longer documentation requirements, and condition-specific intake needs.
Common complexities include:
- Documentation-heavy encounters
- Visit-specific intake requirements
- Variable appointment lengths and care pathways
CERTIFY Health adapts through configurable workflows rather than hard-coded processes.
Operational benefits include:
- Condition-specific intake without slowing check-in
- Flexible scheduling aligned to visit complexity
- Better alignment between scheduling, documentation, and billing workflows
Complex practices gain operational structure without rigidity. This balance is critical. Research shows that forcing standardized workflows onto variable specialties increases staff workarounds and data inconsistency, negating automation benefits.
Why Use-Case Flexibility Matters
Across all practice types, evidence supports the same conclusion. Operational efficiency improves when systems adapt to real-world workflows rather than forcing practices to adapt to software.
CERTIFY Health supports this by delivering a practice management system that scales across size, structure, and specialty without introducing fragmentation.
The result is operational clarity where it is needed and flexibility where it matters most.
Why CERTIFY Health Is the Modern PMS of Choice
Healthcare practices are consolidating software stacks, not expanding them. Operational leaders increasingly recognize that fragmented scheduling, intake, eligibility, and billing tools introduce friction, data inconsistency, and hidden cost.
Administrative fragmentation is a primary driver of staff burnout, revenue leakage, and delayed care delivery.
A modern practice management system must therefore do three things well.
- Convert operational effort into measurable outcomes.
- Scale without increasing overhead.
- Provide continuous operational clarity.
CERTIFY Health is built around this reality.
End-to-End Patient and Practice Operations on One Platform
CERTIFY Health unifies scheduling, registration, intake, eligibility, front and back office operations, billing readiness, and reporting within a single operational layer.
Practices using fragmented administrative systems spend up to 30% more staff time on non-clinical coordination compared to practices operating on unified platforms.
This consolidation directly reduces:
- Duplicate data entry across systems
- Workflow handoffs that introduce error
- Training overhead for new staff
- Dependency on manual reconciliation
Instead of managing integrations between disconnected tools, practices operate from one consistent system of record for operational workflows. This directly improves throughput and reduces operational variance across staff and locations. Here’s a comparison table of the top 3 most widely popular practice management systems in the US.
Best Practice Management Software in the US
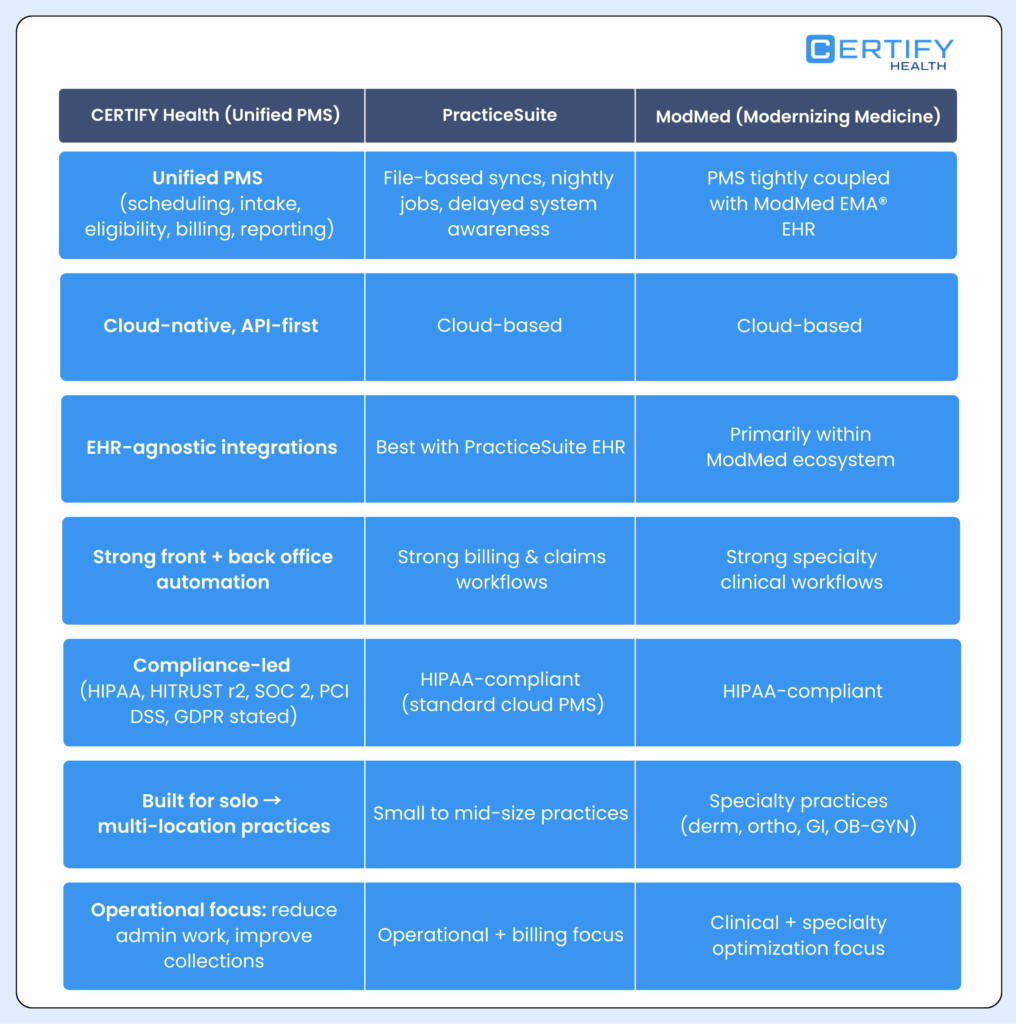
Deep Integration With EHRs, Billing Systems, and Clearinghouses
A modern PMS should not attempt to replace core clinical or financial systems. It should strengthen them.
CERTIFY Health integrates with existing EHRs, billing platforms, and clearinghouses to ensure continuity across clinical, operational, and revenue workflows.
Poor interoperability between administrative and clinical systems significantly increases documentation errors and downstream billing rework.
Integration benefits include:
- Seamless data flow between PMS and EHR systems
- Accurate transfer of demographic, insurance, and encounter data
- Cleaner handoff to billing and claims submission workflows
- Reduced reconciliation effort and fewer downstream corrections
The PMS functions as an operational backbone that complements clinical systems while improving revenue predictability.
Enterprise-Grade Security and Healthcare Compliance
Security and compliance are not optional features. They are baseline requirements for modern healthcare operations.
Lack of auditability and inconsistent access controls are leading contributors to compliance risk in growing healthcare organizations.
CERTIFY Health provides:
- Role-based access controls aligned to staff responsibilities
- Full audit trails across scheduling, intake, eligibility, and billing workflows
- Standards-based data exchange using established healthcare protocols
Compliance is enforced at the system level rather than relying on staff vigilance. This lowers risk while reducing operational friction.
Real-Time Data and Predictive Operational Insights
Most practices manage operations reactively because reporting lags reality. By the time issues appear in reports, revenue has already been delayed or staff capacity has already been exceeded.
Real-time operational dashboards significantly improve decision-making speed and reduce workflow bottlenecks.
CERTIFY Health delivers:
- Trend analysis across scheduling, intake, and billing workflows
- Early visibility into access constraints and staff load
This enables proactive intervention rather than retrospective correction. Practices move from reactive firefighting to continuous operational improvement.
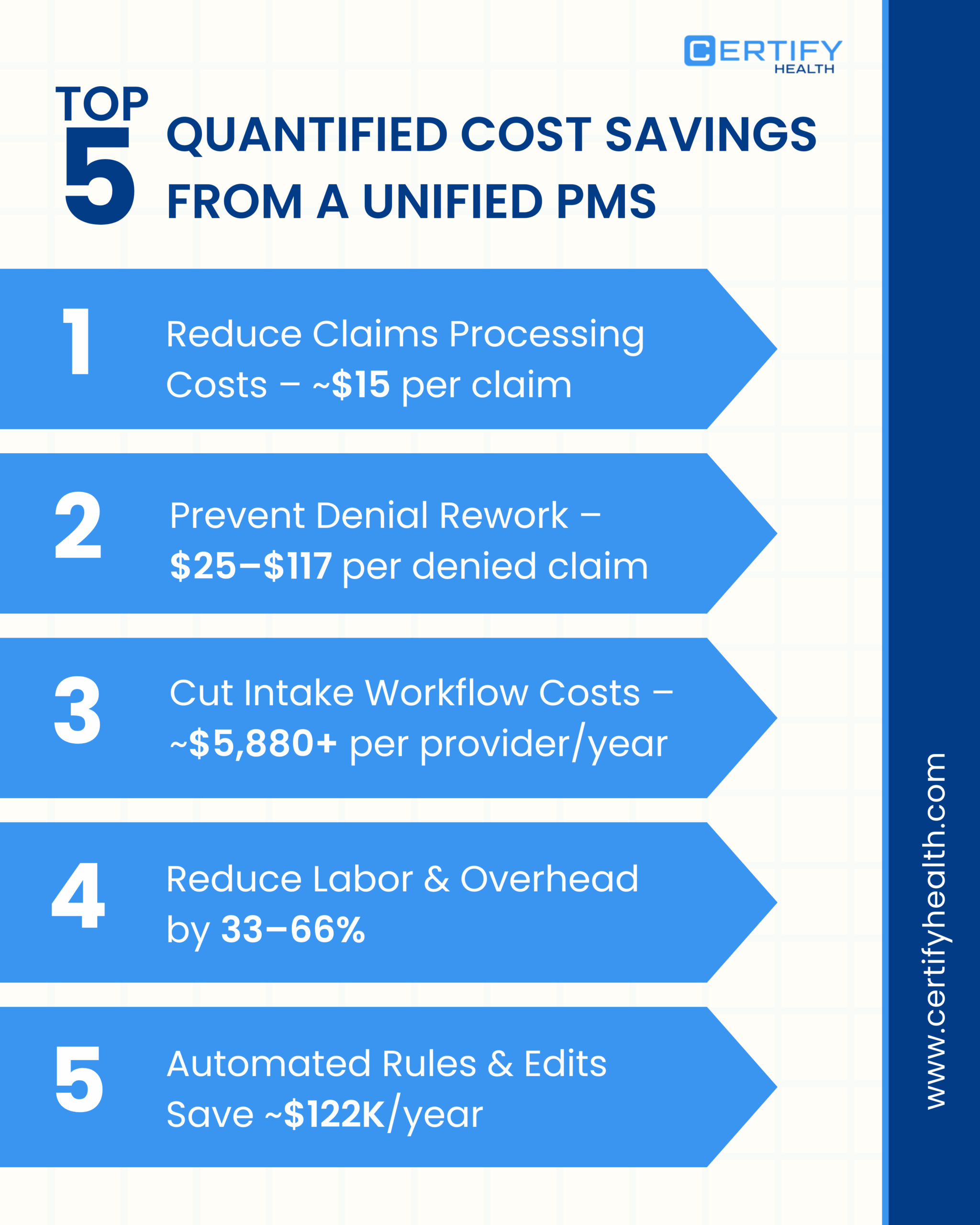
Proven ROI Through Automation
Automation is not about convenience. It is about cost control and revenue protection.
Multiple healthcare operations studies indicate that automation across scheduling, eligibility, and intake can reduce administrative cost per visit while improving first-pass claim acceptance.
Key ROI drivers include:
- Lower no-show rates through automated scheduling workflows
- Faster eligibility verification and fewer coverage-related denials
- Improved first-pass claim accuracy due to cleaner front-end data
- Reduced administrative workload per visit
Automation pays for itself by reducing waste rather than increasing volume.
Implementation and Onboarding
Technology adoption fails when implementation disrupts operations. CERTIFY Health is designed for rapid deployment with minimal disruption to daily workflows.
The onboarding process begins with structured migration planning. Existing workflows are mapped before system configuration to ensure operational continuity. Data is securely imported from legacy systems, preserving historical records and minimizing downtime.
Staff training is role-based rather than generic. Front desk teams, clinical staff, billing teams, and leadership each receive targeted training aligned to their daily responsibilities. Role-specific training significantly improves adoption and reduces error rates during system transitions.
Go-live timelines are predictable and can be phased when necessary to support multi-location or high-volume practices.
Post-launch support does not stop at activation. Ongoing engagement includes:
- Continuous system monitoring
- Workflow optimization guidance as volume grows
- Dedicated customer success support
The goal is long-term operational improvement, not short-term system deployment.
Conclusion: Move From Fragmented Operations to Operational Control
A practice management system determines how efficiently a practice runs, how predictably it grows, and how resilient it remains under operational pressure.
CERTIFY Health enables practices to transition from fragmented, manual workflows to unified, automated operations supported by real-time insight and system-level governance.
Next steps include:
- Requesting a personalized product demonstration
- Conducting a practice operations optimization audit
- Downloading a scheduling automation checklist
Modernize practice operations with a system designed for the realities of today’s healthcare environment.