Table of Contents
Scale and Risk: Why Patient Identification Errors Still Happen
In healthcare, a single identity error can unravel everything. Imagine treating a patient under the wrong identity (wrong meds, wrong history, and wrong treatment path).
Unthinkable, right?
Yet it happens far more often than most hospital leaders realize.
The Reality of Patient Mismatch
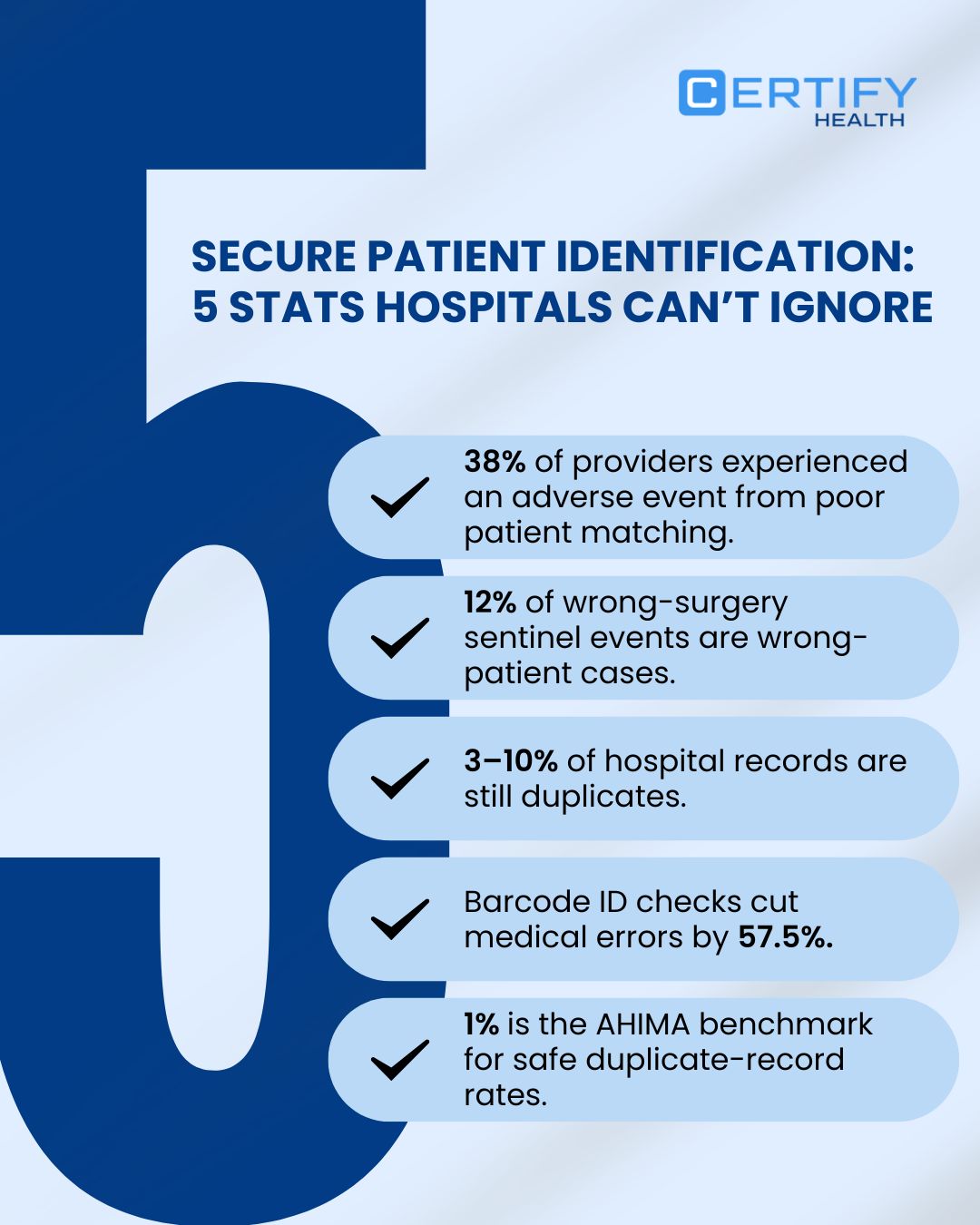
38% of providers report adverse events directly tied to patient mismatches.
3–10% of patient records in hospitals are duplicates, creating a silent, compounding operational risk.
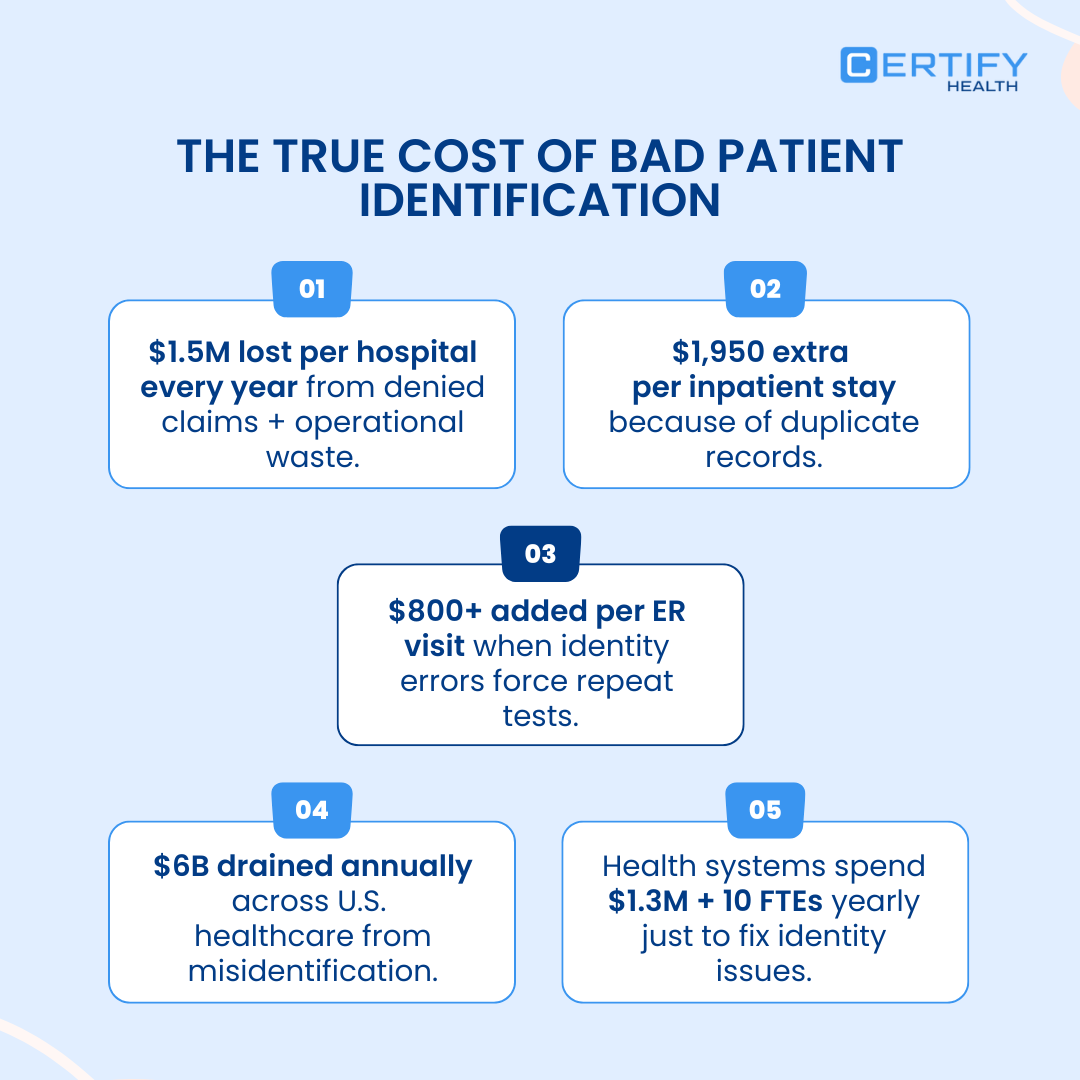
Every duplicate increases the chance of billing errors, clinical delays, denied claims, and compromised patient safety.
If you’re a hospital leader serious about eliminating errors and protecting your reputation, this is your wake-up call.
Read on. By the end, you’ll have actionable, proven strategies to build one of the most secure patient identification frameworks in healthcare.
Why Secure Patient Identification Must Be a Critical Priority
Wrong Identification Directly Fuels Sentinel Events
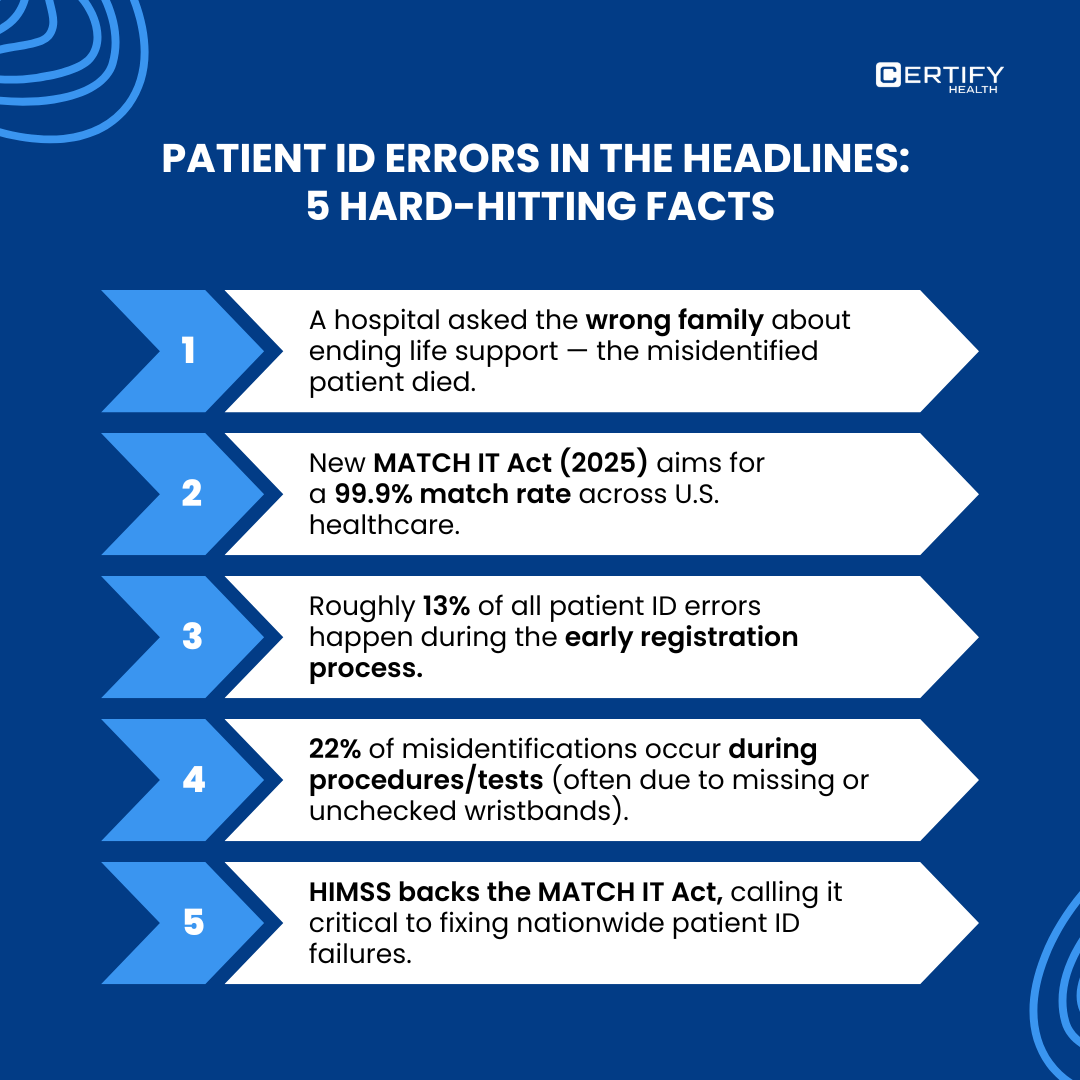
A mismatched patient record isn’t just inconvenient; it’s dangerous. Wrong-site procedures, incorrect treatments, and even wrong-patient interventions happen when identities are mismanaged.
And in healthcare, these aren’t minor mistakes; they can be catastrophic.
The Joint Commission reported 127 sentinel events in 2024 tied to wrong surgeries. 12% involved the wrong patient, a direct consequence of identification failures.
This isn’t theory. It’s happening in real hospitals, to real patients.
Implement Secure Patient ID: A Hospital Setup Guide for Safety
1. Set Measurable Goals: KPIs and Governance for Patient Identification
Duplicate record rates in some hospitals climb as high as 10%. Ignoring this is a recipe for errors.
Focus on these metrics:
- Duplicate error rate: The percentage of existing patient records containing identity conflicts or mismatches.
- Duplicate creation rate: How often new duplicates are created at registration or downstream workflows.
- Time-to-resolution: Average time it takes to identify, review, and merge a duplicate once flagged.
- % of wristband scans before medication administration: A direct indicator of front-line compliance with positive patient identification.
- Number of wrong-patient sentinel events: The highest-severity indicator that your identification controls are failing.
Why These Metrics Matter
Tracking these consistently gives you a pulse on identity integrity. You can:
- Spot patterns early
- Strengthen governance
- Reduce clinical risk
- Ensure compliance with AHIMA, JCI, and WHO safety recommendations
Benchmark to Aim For
AHIMA recommends a duplicate error rate of 1% or lower.
To reach that, registration, data entry, EHR workflows, and identity governance must be standardized, repeatable, and enforced across the organization.
Measure it. Track it. Govern it. That’s how you move from reactive cleanup to long-term safety.
2. People + Process: Human-Factor Controls to Prevent Misidentification
Front-Line Protocols Every Hospital Must Enforce
Three proven practices prevent wrong-patient procedures:
- Two independent identifiers: Full name + date of birth, at a minimum.
- Bedside verification: Always confirm identity before meds, labs, or procedures.
- Time-out checks: Pause to confirm correct patient, procedure, and site.
These steps may feel routine, but they’re the thin line between accuracy and catastrophic error. Consistency is everything.
Training & Interruption Management Matter
Even strong protocols fail if staff are interrupted or unclear on communication. Root-cause analyses point to:
- Interruptions during verification
- Poor communication between staff
Structured “pause protocols” and scenario-based training cut misidentification significantly, sometimes by double digits.
The Takeaway
Build two pillars:
- Routine, scenario-based identity verification training
- Structured interruption management
When embedded in culture, not just policy, error rates drop fast.
3. Technology: What Works for Patient Identification (barcode, EMPI, biometrics)
Short answer: barcode wristbands, a tuned EMPI, and biometrics each move the needle, but none is a silver bullet. Use them together, matched to workflows, governance, and privacy controls.
TL;DR
- Barcode wristbands = proven, fastest safety lift (~57.5% fewer errors in meta-analysis).
- EMPI = required for long-term duplicate control (addresses 3–10% duplicate baseline).
- Biometrics = powerful augmentation if you follow NIST standards and privacy/consent rules.
- Best outcome: combine all three with strong governance, monitoring (creation / error / time-to-resolution), and fallback checks. That’s how you move toward <1% duplicate records and far fewer wrong-patient events.
Barcode wristbands (positive patient identification wristbands)
Point-of-care wristband scanning ties actions (meds, labs, procedures) to the correct patient instantly.
Meta-analysis data show wristband/barcode scanning implementations cut medical errors by ~57.5% where used at point of care.
Trade-offs: cheap and fast to deploy but depends on reliable printing at point-of-care, staff discipline to scan every time, and barcode durability (wear/tear).
Barcode systems reduce human error but fail when people skip scans or when wristbands aren’t printed/attached correctly.
EMPI / matching algorithms
Enterprise Master Patient Index (EMPI) or probabilistic/deterministic matching algorithms to detect and reconcile duplicate records across systems.
EMPI investment + governance is a primary way to lower that.
Trade-offs: EMPI reduces duplicates when tuned and governed, but needs high-quality demographic inputs, ongoing tuning, and data standards (name formats, addresses, DOB handling).
Expect ongoing maintenance, false positives/negatives, and governance overhead but big downstream savings in safety and revenue when done right.
Biometrics (face / fingerprint)
Biometrics provide a live physiological link to identity (fingerprint, face, iris) and can augment registration and check-in flows to prevent duplicate creation and wrong-patient care.
NIST runs biometric quality and algorithm evaluations and publishes standards/benchmarks. So, follow NIST controls and tests when you adopt biometrics. Use biometric verification as an augmentation, not the sole identifier.
Trade-offs: High accuracy (especially multimodal biometrics) but concerns include enrollment quality, lighting/finger condition, demographics bias, privacy/consent, and regulatory constraints. Plan for fallback flows (ID + two identifiers) and strong data protection (encryption, consent logs, retention limits).
How CERTIFY Health Fits
Think of CERTIFY Health as the front door to identity accuracy. The platform combines identity matching, FaceCheck biometrics, QR/RFID, and EHR-native APIs to ensure the right patient is verified at every step (from check-in to care to payment).
It’s not just tech for tech’s sake. When you’re building a combined governance + technical approach, CERTIFY Health’s model shows exactly how to tie point-of-care verification, identity matching, and patient-facing options into a single, reliable workflow.
In short: fewer errors, smoother operations, and safer care, without leaving the human factor behind.
4. Data Quality & Interoperability: Evidence-Backed Controls to Fix Patient Identification Fast
Address Standardization: The Highest-Impact, Fastest Win
Address inconsistency is one of the biggest silent drivers of patient misidentification across EHRs and HIE networks.
Small variations like “St.” vs “Street,” missing apartment numbers, and inconsistent ZIP formats trigger false non-matches and duplicate creation at scale.
USPS-style address normalization is the fastest, highest-ROI intervention. Research shows it can immediately improve EMPI and HIE match sensitivity by 10–20 percentage points, with some datasets achieving 90%+ sensitivity after normalization.
If a hospital must pick one data-quality control to implement first, it should be this.
Attribute Availability & Completeness: The Core Matching KPI
Matching engines fail when core demographic fields are missing.
Studies show consistent capture of:
- Legal name
- DOB
- Address / ZIP code
- Phone + email
directly boosts cross-organization patient matching performance.
Cross-System Interoperability & HIE Match Health
When data move across systems, matching accuracy drops sharply. Track Cross-System Deterministic Match Rate: the % of inbound external records that match without human review or probabilistic logic.
Many HIE studies show rates fall below 80% without standardized fields; aim for >95% with normalization and HL7/FHIR conformance.
Algorithmic Match Accuracy Benchmarking
Measure Referential/Probabilistic Match Sensitivity & PPV using a manually validated gold-standard sample. National evaluations show well-tuned engines achieve mid-90s% in both metrics.
Roadmap to Secure Patient Identification with CERTIFY Health
Achieving secure patient identification with a platform like CERTIFY Health involves a comprehensive roadmap that integrates advanced technology (like biometrics and automated intake) with updated hospital workflows and staff training. The goal is to establish Positive Patient Identification (PPID) from the very first patient touchpoint.
Here is a phased roadmap for implementation:
30 Days: Establish the Baseline + Fix the Front Line
- Measure duplicate rate, creation rate, time-to-resolution (AHIMA benchmark).
- Enforce two-identifier policy + bedside/point-of-care verification.
- Implement print-at-point-of-care wristbands.
Accurate Patient Intake and Identity Verification at Registration via CERTIFY Health
- CERTIFY’s digital check-in (mobile/kiosk/tablet/SMS) captures structured demographics and photo ID, reducing manual entry errors and supporting clean data capture from the start.
- ID & insurance capture (OCR, eConsent) standardizes critical fields, minimizing the chance of creating duplicate records.
- FaceCheck biometric enrollment provides an additional identity verification layer at registration.
60 Days: Operationalize Scanning + Staff Reliability
- Deploy ID-verification tools at med-admin, labs, and diagnostics.
- Train staff on interruption-free ID verification and time-outs.
- Track compliance metrics: % scans, error occurrences.
Real-Time Verification Across Frontline Workflows
- FaceCheck biometric authentication verifies patient identity during every check-in or encounter, reducing misidentification risks.
- Multi-channel check-in (mobile/kiosk/tablet) minimizes reliance on manual identifiers, helping staff follow two-identifier policies reliably.
- EHR/PMS interoperability ensures verified identity attributes propagate into clinical systems consistently.
Note that CERTIFY does not provide barcode wristband scanning or compliance dashboards, so hospitals can continue using existing wristband workflows and audit tools while CERTIFY reinforces identity verification at the point of check-in.
90+ Days: Strengthen the Backbone (EMPI + Biometric QA)
- Tune EMPI matching rules, establish governance, and define SLA metrics for duplicate resolution.
- Pilot biometrics (face/fingerprint) as secondary identifiers with QA and privacy checks.
- Implement continuous improvement cycles: weekly duplicates, monthly merges, quarterly audits.
Secure Data Integration
- HITRUST-certified secure storage ensures biometric and demographic data is protected and auditable.
- EHR/FHIR/HL7 integration allows identity data to flow consistently into clinical and administrative systems.
CERTIFY Health does not provide EMPI or duplicate-governance workflows, so hospitals still manage EMPI tuning, duplicate resolution, and audit reporting; CERTIFY complements these by providing accurate, verified identity data feeding into the EMPI.
Conclusion
Use CERTIFY Health to fix the front door of patient identification, while your EMPI and governance framework drive long-term identity accuracy. This includes cleaner intake, stronger verification, fewer mis-entries, etc. Book a demo to learn more.
























