Table of Contents
Key Takeaways
- Healthcare admin costs can reach up to $1 trillion a year in the U.S.
- 15–30% of a practice’s budget is spent on administration, not direct patient care.
- Complex processes, legacy technology, and changing regulations drive costs even higher.
- Automation, standardization, and centralized platforms like CERTIFY health can drastically cut admin costs.
- Collaboration and policy harmonization are critical for lasting, system-wide savings.
Introduction
Healthcare administrative cost is the silent budget, buster in every practice, relentlessly climbing and devouring dollars meant for frontline care, often accounting for up to $1 trillion per year in U.S. healthcare spending.
Tackling this runaway expense starts with understanding where the leakage happens and deploying smart, actionable strategies that transform operations. Let’s break down why administrative costs spiral and how practices can finally tame them.
How much of healthcare costs are administrative?
Behind the scenes of patient care, healthcare administrative cost is quietly mushrooming, eroding profit margins, draining resources, and threatening long, term sustainability for practices of all sizes.
Healthcare practices spend 15-30% of their total budget on paperwork, billing, and managing regulations , more than what’s spent on treating cancer or heart disease.
Why are administrative costs in healthcare so high?
Administrative expenses are not just a line item; they’re a crisis. Practices spend staggering sums on tasks like claims processing, prior authorization, credentialing, licensing, and directory management, often in the name of compliance.
Add in legacy technology, manual workflows, frequent regulation changes, data privacy concerns, and the spiral speeds up.
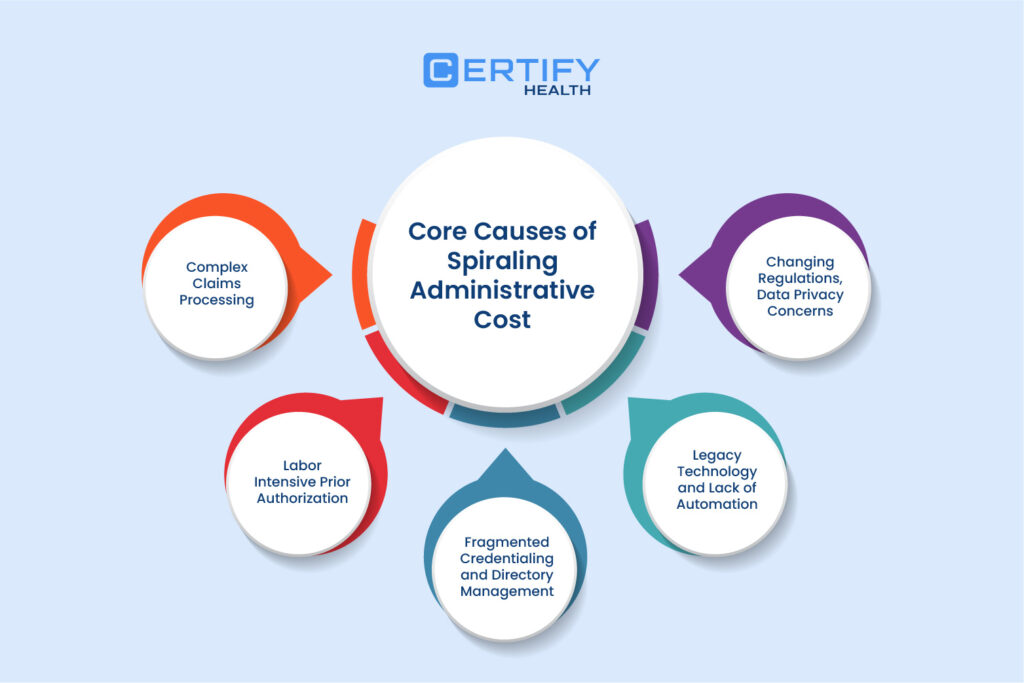
Core Causes of Spiraling Administrative Cost
TL; DR
Why are US healthcare costs so high?
- Complex claims and billing processes result in more errors and higher costs.
- Manual prior authorization steps lead to staff burnout and repeated reviews.
- Fragmented credentialing means constant updates for each hospital, state, or payer.
- Outdated technology slows workflows and blocks automation.
- Frequent regulation and privacy changes force costly manual work due to lack of standardization.
Complex Claims Processing
- Every claim moves through a maze: multiple payer systems, inconsistent rules, endless manual steps, and costly adjustments make claims processing the king of administrative expense.
- Hospital claims processing, plus medical billing insurance claims processing, are weighed down by legacy reporting technology and a lack of automation, leading to denied claims, duplicate submissions, and protracted payment cycles.
- More moving parts mean more opportunities for error, and more admin cost.
Labor Intensive Prior Authorization
- Treatment authorization and prior authorization are another time sink, with providers tasked to chase approvals for diagnostics, surgery, or medications.
- High error rates and constant rework force staff to repeat reviews, raising admin expense even further.
- Provider burnout isn’t just a clinical issue, it’s a direct result of excessive admin cost and the grind of manual authorization steps.
Fragmented Credentialing and Directory Management
- Credentialing isn’t one, size, fits, all. Each hospital, state, and payer has its own requirements for licensure process and directory management.
- Frequent updates, changing documentation standards, regulatory discrepancies, and ongoing verifications create a never-ending pile of admin expense for practices.
- Practically speaking, maintaining compliance and up-to-date documentation drains time, money, and morale.
Legacy Technology and Lack of Automation
- Outdated systems block claims automation, payment automation, and even basic workflow optimization.
- Practices tied to legacy tech face sluggish interoperability, frequent process breakdowns, and high manual overhead, further ballooning administrative expense.
- Reluctance to invest in technology keeps practices stuck, driving up admin cost and inviting compliance risk.
Changing Regulations, Data Privacy Concerns
- Administrative costs escalate fast as practices struggle to keep up with regulation changes, compliance updates, and strict data privacy concerns.
- Lack of standardization, every payer and regulator uses different forms, policies, and reporting methods, forces manual work that multiplies admin cost.

Impact of Overspending
Direct financial loss is only half the story. Overspending on administrative cost means less investment in clinicians, technology, and patient care.
Indirect effects include clinician burnout from relentless data entry, lower patient experience scores due to distracted staff, and reduced face-time with patients, all triggered by excessive admin expense.
Practice leaders feel squeezed: They want operational performance, but admin cost keeps getting in the way.
Proven Strategies for Reducing Administrative Costs

TL; DR
How to reduce administrative costs in healthcare?
- Automate claims and payments to cut manual work and speed up revenue cycles.
- Centralize claims through clearinghouses and standardize authorization policies to reduce complexity.
- Use unified credentialing platforms and national directories to minimize repetitive credentialing tasks.
- Upgrade legacy systems and optimize workflows to improve efficiency and reduce errors.
- Promote industry-wide collaboration and policy harmonization to simplify regulations and cut redundant admin work.
Legacy Technology and Lack of Automation
- Claims automation tools such as CERTIFY Health’s practice management system can auto adjudicate the majority of claims, reduce manual touchpoints, and accelerate payment cycles, slashing both administrative expense and payment delays.
- Payment automation, like automated clearing house (ACH) processing, frees up staff from check cutting and deposit tracking, reducing admin cost.
Centralize Clearinghouses & Standardize Policies
- Move claims processing through a centralized clearinghouse to harmonize workflows, document formats, and transaction standards.
- Standardize prior authorization policies, especially for routine, low, risk treatments, so practices don’t waste admin expense chasing approvals that shouldn’t need them.
Streamline Credentialing and Directory Updates
- Invest in national provider directories, unified credentialing platforms, and automated license verification processes.
- This approach decreases duplicative documents and frees practices from the cycle of responding to every payer’s unique requirements, keeping admin cost in check.
Key insight: Credentialing requirements change constantly. A national unified system lets providers update info once instead of countless times, removing massive admin costs and admin expenses from operations.
Invest in Technology and Workflow Optimization
- Ditch legacy technology. Modern digital platforms like CERTIFY Health automate repetitive tasks (claims, prior auth, credentialing), monitor regulatory changes, and enable process harmonization.
- Upskill admin staff for high, value activities, let automation handle the routine, so staff can focus on high value task, compliance, and patient support.
Foster Public & Private Sector Collaboration
- System-wide reforms driven by collaboration between practices, payers, vendors, and government are vital for process harmonization and real regulatory simplification.
- Industry wide agreements on common credentialing standards, billing formats, and claims processing workflows will cut redundant admin expenses and accelerate care.
Policy Harmonization: Make the rules and procedures consistent across all players, payers, providers, and regulators. That means mandatory standardization and regulatory simplification, reducing unnecessary complexity, and stopping admin cost from spiraling. Collaboration clears the paperwork logjam and wipes out inefficiencies caused by conflicting requirements.
Conclusion
Healthcare administrative costs are a profound threat to the financial health of every practice, and to the care delivered to every patient. Reducing excess admin costs is not optional but urgent, promising to recapture billions each year for direct patient care, staff well, being, and medical innovation.
Healthcare leaders have a choice: keep drowning in spiraling administrative costs, or fight back with automation, standardization, and smarter workflows. The time to act is now, invest in technology, harmonize processes, and reclaim resources for what matters most.
Let’s turn healthcare administration from headaches to competitive advantage.
As a next step, read: How Technology Can Streamline Practice Operations and Augment Staff Retention
























